Little attention has been given to the effect of vascular access site on mortality, while an increasing body of evidence is showing that radial access has much more benefit than femoral access for ST-segment elevation myocardial infarction patients. We aimed to assess the influence of vascular access site on mortality at 30 days and at 1 year in ST-segment elevation myocardial infarction patients.
MethodsWe included all patients with ST-segment elevation myocardial infarction who had undergone primary angioplasty at 2 Galician hospitals between 2008 and 2010. We performed 2 multivariate regression models for each endpoint (30-day and 1-year mortality). The only difference between these models was the inclusion or not of the vascular access site (femoral vs radial). For each of the 4 models we calculated the Hosmer-Lemeshow test and the C-index. We also tested the interaction between hemodynamic instability and vascular access.
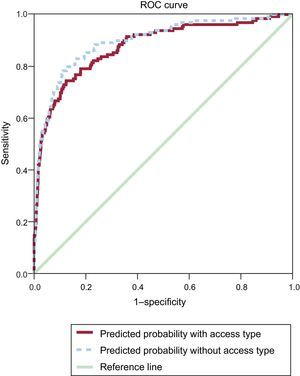
ResultsWe included 1461 patients with a mean age of 64. Of these patients, 86% had radial access and 7.4% had hemodynamic instability. All-cause mortality was 6.8% (100/1461) at 30 days and 9.3% (136/1461) at 1 year. Vascular access site follows hemodynamic instability and age in terms of effect on mortality risk, with an odds ratio of 5.20 (95% confidence interval, 2.80-9.66) for 30-day mortality. A similar effect occurs for 1-year mortality. The C-index slightly improves (without achieving statistical significance) with the inclusion of the vascular access site.
ConclusionsVascular access site should be taken into account when predicting mortality after a primary percutaneous coronary intervention.
Keywords
Myocardial infarction is one of the main causes of mortality and morbidity in developed countries. In recent years, mortality has decreased due to a better control of risk factors and an increased effectiveness of therapeutic treatments, mainly percutaneous coronary interventions (PCI).1,2 Primary angioplasty is considered the best reperfusion strategy for patients with ST-segment elevation myocardial infarction (STEMI) and it should be offered within 90min of contact with the health care system.3
The Galician Health Service, in northwest Spain, enacted a health program in 2005 aimed to improve the attention to myocardial infarction, named PROGALIAM.4,5 This program represents a milestone in Europe and was probably one of the first to implement certain strategies that have improved the care of these patients: a) patients are transferred not to the nearest hospital but to the nearest hospital with PCI capabilities; b) the patient is delivered directly to a cath lab, bypassing the emergency care unit, which shortens the ischemia time,5 and c) radial access is the first choice for PCI.
On the other hand, predicting the risk of death after PCI in patients with myocardial infarction has been a concern for surgeons. Many risk scores have been developed in recent years (TIMI, PAMI, CADILLAC, GRACE, NCDR, EuroHeart-PCI).6–11 Although the included variables are not the same in all scores, most of them include the 2 variables most associated with mortality: hemodynamic instability, followed by age. Recent studies, one of them a meta-analysis, have shown that vascular access is a key variable in successful outcome after a PCI procedure, with radial access reducing mortality by approximately 50%.12,13 Nevertheless, vascular access site has not been considered in the available mortality scores. Femoral artery access has been associated with much higher bleeding complications, and radial access with less kidney injury due to a lower use of contrast.14–16 Despite this biological rationale favoring radial access, the RIVAL study did not find major differences between vascular access sites.14 A result favoring radial access was recently reported by the RIFLE-STEACS study, showing lower morbidity and cardiac mortality. Interestingly, this study was performed in a clinical practice setting instead of being designed as a clinical trial.17 Radial access shortens hospital stay and is probably more cost-effective than femoral access for PCI.
The aim of this paper is to assess the importance of vascular access site when predicting 30-day and 1-year all-cause mortality in patients with STEMI.
METHODSDesign and SettingPatients were recruited at 2 Galician university hospitals, in A Coruña and Santiago de Compostela. The population covered by the A Coruña University Hospital Complex comprises approximately 1 100 000 inhabitants and that of Santiago de Compostela University Hospital Complex is close to 500 000 inhabitants. The study has a retrospective cohort design.
Inclusion and Exclusion CriteriaAll patients presenting with STEMI between 2008 and 2010 who underwent primary angioplasty were included. The only exclusion criterion was to present a non ST-segment myocardial infarction. STEMI was defined according to the third universal definition of myocardial infarction, recently published by the European Society of Cardiology.18
Follow-up and EndpointsThe vital status of the included patients was assessed at regular intervals by clinicians of the 2 participating centers. When a patient dies, this information is updated in the electronic medical record approximately 2 months after the event. Surviving patients had a follow-up longer than 1 year and the main result was all-cause mortality at 30 days and at 1 year after a PCI for STEMI. This information was retrieved from the electronic medical records of the included patients.
Information RetrievalThe information collected for each patient can be classified as follows: a) demographic characteristics and pre-infarction variables: age, sex, body mass index, hypertension, diabetes, smoking status, dyslipidemia, peripheral artery disease, chronic kidney disease, previous PCI, previous acute myocardial infarction, congestive heart failure, and previous stroke; b) acute myocardial infarction presentation: type of contact with the health system, ischemia time, number of affected arteries, and hemodynamic instability; c) information regarding or obtained through PCI procedure: vascular access site, lesion in left coronary artery, TIMI flow, and d) outcomes: 30-day and 1-year all-cause mortality. Many of these variables were transformed into categorical variables.
Statistical AnalysisWe performed a descriptive univariate analysis of the included variables followed by 2 multivariate logistic regression models, each with the dependent variable of mortality at 30 days and at 1 year. Bivariate analysis compared the characteristics of individuals who underwent different vascular accesses at STEMI presentation. To compare these characteristics by type of vascular access we used Pearson's ji squared test or Mann-Whitney's U as appropriate. We formally tested the possible interaction between hemodynamic instability and vascular access site by calculating the Synergism index (S-index).
For each endpoint (30 days and 1 year) we performed 2 multivariate models. The only difference was to include or not the vascular access site, in order to compare the influence of vascular access type on the risks obtained with the other variables. Most of the included variables in both multivariate logistic regression models were the same as those used in the EuroHeart-PCI score for STEMI.11 We did not use automatic procedures for the inclusion of variables in the models. The results are expressed as odds ratios (OR) with 95% confidence interval (95%CI). For all the models we calculated the Hosmer-Lemeshow calibration test and the C index. We compared the performance of the models with the inclusion of vascular access at 30 days and at one year using receiver operating characteristic (ROC) curves. All the analyses were performed with SPSS v17.0.
RESULTSThe included sample consisted of 1461 individuals, 1001 at the A Coruña Hospital and 460 at the Santiago de Compostela Hospital. There were no differences in patient characteristics between hospitals (Table 1).
Sample Characteristics Before ST-segment Elevation Myocardial Infarction Onset
| Variables | Total (n=1461) |
| Sex male | 1127 (77.1) |
| Age, years | 64 [54-75] |
| Body mass index | 27.7 [25.5-30.4] |
| Diabetes | 308 (21.1) |
| Hypertension | 722 (49.4) |
| Tobacco use* | |
| Current smoker | 756 (51.7) |
| Missing | 4 (0.2) |
| Hypercholesterolemia | 612 (41.9) |
| Peripheral artery disease | 47 (3.2) |
| Chronic renal disease | 79 (5.4) |
| Previous AMI | 112 (7.7) |
| Previous stroke | 62 (4.3) |
| Previous PCI | 116 (7.9) |
| Previous coronary artery bypass graft | 7 (0.5) |
| Congestive heart failure | 96 (6.6) |
AMI, acute myocardial infarction; PCI, percutaneous coronary intervention.
Data are expressed as no. (%) or median [interquartile range].
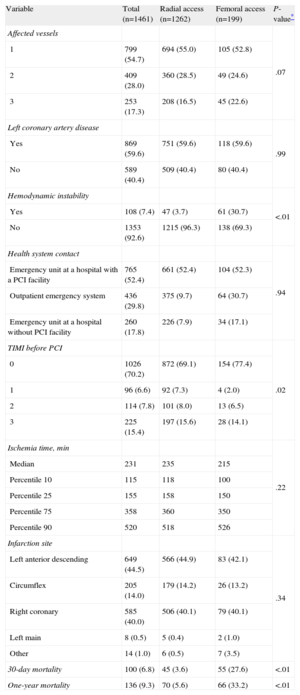
Patient characteristics regarding STEMI presentation are shown in Table 2. Eighty-six percent of patients had radial access and 7.4% had STEMI with hemodynamic instability. All-cause mortality was 6.8% (100/1461) at 30 days and 9.3% (136/1461) at 1 year. There were no losses to follow-up. Individuals with femoral access presented a higher percentage of hemodynamic instability and TIMI 0 and 1 when they arrived at hospital, compared to those who underwent radial access. Crude all-cause mortality was also higher at 1 month and at 1 year for individuals with femoral access (Table 2). If we analyze only those patients with hemodynamic instability, we can observe a crude 30-day mortality of 65.6% for femoral access vs 42.6% for radial access (χ2 test P-value=.017). The same comparison for 1-year mortality is 68.9% for femoral access vs 55.3% for radial access (χ2 test P-value=.149). There is a significant additive interaction between vascular access and hemodynamic instability (S-index=3.06; 95%CI, 1.35-6.69; P=.004) for 30-day mortality but not for 1-year mortality (S-index=1.91; 95%CI, 0.84-4.33; P=.061).
ST-segment Elevation Myocardial Infarction Onset and Percutaneous Coronary Intervention Characteristics, by Vascular Access Site
| Variable | Total (n=1461) | Radial access (n=1262) | Femoral access (n=199) | P-value* |
| Affected vessels | .07 | |||
| 1 | 799 (54.7) | 694 (55.0) | 105 (52.8) | |
| 2 | 409 (28.0) | 360 (28.5) | 49 (24.6) | |
| 3 | 253 (17.3) | 208 (16.5) | 45 (22.6) | |
| Left coronary artery disease | .99 | |||
| Yes | 869 (59.6) | 751 (59.6) | 118 (59.6) | |
| No | 589 (40.4) | 509 (40.4) | 80 (40.4) | |
| Hemodynamic instability | <.01 | |||
| Yes | 108 (7.4) | 47 (3.7) | 61 (30.7) | |
| No | 1353 (92.6) | 1215 (96.3) | 138 (69.3) | |
| Health system contact | .94 | |||
| Emergency unit at a hospital with a PCI facility | 765 (52.4) | 661 (52.4) | 104 (52.3) | |
| Outpatient emergency system | 436 (29.8) | 375 (9.7) | 64 (30.7) | |
| Emergency unit at a hospital without PCI facility | 260 (17.8) | 226 (7.9) | 34 (17.1) | |
| TIMI before PCI | .02 | |||
| 0 | 1026 (70.2) | 872 (69.1) | 154 (77.4) | |
| 1 | 96 (6.6) | 92 (7.3) | 4 (2.0) | |
| 2 | 114 (7.8) | 101 (8.0) | 13 (6.5) | |
| 3 | 225 (15.4) | 197 (15.6) | 28 (14.1) | |
| Ischemia time, min | .22 | |||
| Median | 231 | 235 | 215 | |
| Percentile 10 | 115 | 118 | 100 | |
| Percentile 25 | 155 | 158 | 150 | |
| Percentile 75 | 358 | 360 | 350 | |
| Percentile 90 | 520 | 518 | 526 | |
| Infarction site | .34 | |||
| Left anterior descending | 649 (44.5) | 566 (44.9) | 83 (42.1) | |
| Circumflex | 205 (14.0) | 179 (14.2) | 26 (13.2) | |
| Right coronary | 585 (40.0) | 506 (40.1) | 79 (40.1) | |
| Left main | 8 (0.5) | 5 (0.4) | 2 (1.0) | |
| Other | 14 (1.0) | 6 (0.5) | 7 (3.5) | |
| 30-day mortality | 100 (6.8) | 45 (3.6) | 55 (27.6) | <.01 |
| One-year mortality | 136 (9.3) | 70 (5.6) | 66 (33.2) | <.01 |
PCI, percutaneous coronary intervention; TIMI, Thrombolysis in Myocardial Infarction.
Unless otherwise indicated, data are expressed as no. (%).
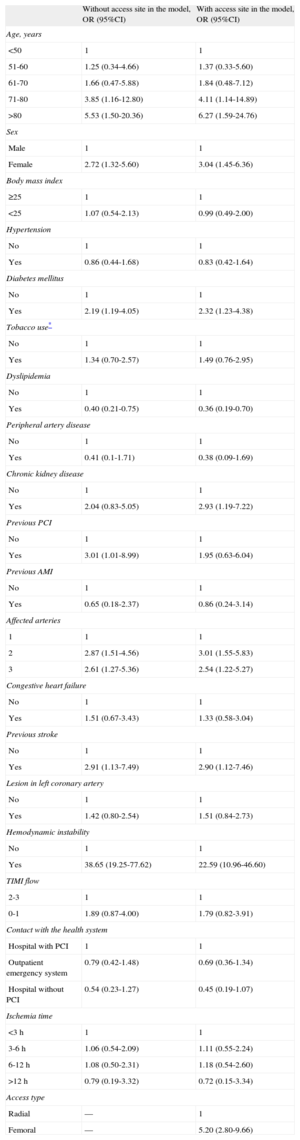
When calculating 30-day all-cause mortality in a multivariate model not including the vascular access site, we observed that the most important variable is hemodynamic instability (OR=38.65; 95%CI, 19.25-77.62), followed by age (OR for those older than 80=5.53; 95%CI, 1.50-20.36) and previous PCI (OR=3.01; 95%CI, 1.01-8.99). The results for each of the variables included in this model are shown in Table 3. There were no important differences in the effect of vascular access site when the participating centers were analyzed separately. The Hosmer-Lemeshow P-test value is=0.41 (χ2 value=8.27) and the C index is 0.909 (95%CI, 0.877-0.942; P<.001). When we introduce the vascular access site into the model, the most important variable is hemodynamic instability (OR=22.59; 95%CI, 10.96-46.60), followed by age (OR for those older than 80=6.27; 95%CI, 1.59-24.76) and access site, with those undergoing femoral access having 5.20 (95%CI, 2.80-9.66) higher probability of death at 30 days, compared with radial access. There were slight differences between the models in the risks posed by other variables (Table 3). The Hosmer-Lemeshow P-test value for the 30-day mortality model including vascular access is=0.28 (χ2 value=9.74) and the C index is 0.928 (95%CI, 0.900-0.956; P<.001). Figure 1 displays the ROC curve for both models, with the only difference being the inclusion or not of the vascular access site. Slightly better performance can be observed for the model including vascular access site. There were no statistical differences between the C indexes.
Thirty-day Risk of Death After ST-segment Elevation Myocardial Infarction With or Without Radial Access
| Without access site in the model, OR (95%CI) | With access site in the model, OR (95%CI) | |
| Age, years | ||
| <50 | 1 | 1 |
| 51-60 | 1.25 (0.34-4.66) | 1.37 (0.33-5.60) |
| 61-70 | 1.66 (0.47-5.88) | 1.84 (0.48-7.12) |
| 71-80 | 3.85 (1.16-12.80) | 4.11 (1.14-14.89) |
| >80 | 5.53 (1.50-20.36) | 6.27 (1.59-24.76) |
| Sex | ||
| Male | 1 | 1 |
| Female | 2.72 (1.32-5.60) | 3.04 (1.45-6.36) |
| Body mass index | ||
| ≥25 | 1 | 1 |
| <25 | 1.07 (0.54-2.13) | 0.99 (0.49-2.00) |
| Hypertension | ||
| No | 1 | 1 |
| Yes | 0.86 (0.44-1.68) | 0.83 (0.42-1.64) |
| Diabetes mellitus | ||
| No | 1 | 1 |
| Yes | 2.19 (1.19-4.05) | 2.32 (1.23-4.38) |
| Tobacco use* | ||
| No | 1 | 1 |
| Yes | 1.34 (0.70-2.57) | 1.49 (0.76-2.95) |
| Dyslipidemia | ||
| No | 1 | 1 |
| Yes | 0.40 (0.21-0.75) | 0.36 (0.19-0.70) |
| Peripheral artery disease | ||
| No | 1 | 1 |
| Yes | 0.41 (0.1-1.71) | 0.38 (0.09-1.69) |
| Chronic kidney disease | ||
| No | 1 | 1 |
| Yes | 2.04 (0.83-5.05) | 2.93 (1.19-7.22) |
| Previous PCI | ||
| No | 1 | 1 |
| Yes | 3.01 (1.01-8.99) | 1.95 (0.63-6.04) |
| Previous AMI | ||
| No | 1 | 1 |
| Yes | 0.65 (0.18-2.37) | 0.86 (0.24-3.14) |
| Affected arteries | ||
| 1 | 1 | 1 |
| 2 | 2.87 (1.51-4.56) | 3.01 (1.55-5.83) |
| 3 | 2.61 (1.27-5.36) | 2.54 (1.22-5.27) |
| Congestive heart failure | ||
| No | 1 | 1 |
| Yes | 1.51 (0.67-3.43) | 1.33 (0.58-3.04) |
| Previous stroke | ||
| No | 1 | 1 |
| Yes | 2.91 (1.13-7.49) | 2.90 (1.12-7.46) |
| Lesion in left coronary artery | ||
| No | 1 | 1 |
| Yes | 1.42 (0.80-2.54) | 1.51 (0.84-2.73) |
| Hemodynamic instability | ||
| No | 1 | 1 |
| Yes | 38.65 (19.25-77.62) | 22.59 (10.96-46.60) |
| TIMI flow | ||
| 2-3 | 1 | 1 |
| 0-1 | 1.89 (0.87-4.00) | 1.79 (0.82-3.91) |
| Contact with the health system | ||
| Hospital with PCI | 1 | 1 |
| Outpatient emergency system | 0.79 (0.42-1.48) | 0.69 (0.36-1.34) |
| Hospital without PCI | 0.54 (0.23-1.27) | 0.45 (0.19-1.07) |
| Ischemia time | ||
| <3 h | 1 | 1 |
| 3-6 h | 1.06 (0.54-2.09) | 1.11 (0.55-2.24) |
| 6-12 h | 1.08 (0.50-2.31) | 1.18 (0.54-2.60) |
| >12 h | 0.79 (0.19-3.32) | 0.72 (0.15-3.34) |
| Access type | ||
| Radial | — | 1 |
| Femoral | — | 5.20 (2.80-9.66) |
95%CI, 95% confidence interval; AMI, acute myocardial infarction; PCI, percutaneous coronary intervention; OR, odds ratio; TIMI, Thrombolysis in Myocardial Infarction.
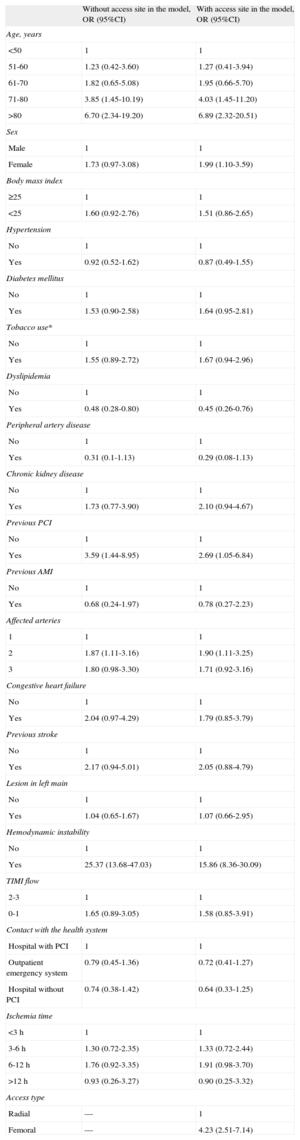
Table 4 displays the differences between risk models at 1 year when including or not vascular access type. In the model not including vascular access, the most important variable is hemodynamic instability (OR=25.37; 95%CI, 13.68-47.03), followed by age (OR for those older than 80=6.70; 95%CI, 2.34-19.20) and previous PCI (OR=3.59; 95%CI, 1.44-8.95). The Hosmer-Lemeshow P-value for this regression is=0.53 (χ2 value=7.10) and the C-index is 0.877 (95%CI, 0.842-0.913; P<.001). When the regression model includes vascular access type, the most predictive variable is hemodynamic instability (OR=15.86; 95%CI, 8.36-30.09), followed by age (OR for those older than 80=6.89; 95%CI, 2.32-20.51) and vascular access, with femoral access posing an OR of 4.23 (95%CI, 2.51-7.14) compared with radial access. The Hosmer-Lemeshow test P-value is=0.76 (χ2 value=14.22) and the C-index is=0.897 (95%CI, 0.865-0.928; P<.001). Figure 2 displays the ROC curves for both models with or without vascular access. There were no statistical differences between the C indexes. When each of the participating centers was analyzed separately, 1-year mortality was slightly higher for one of the participating hospitals, probably due to a higher percentage of patients presenting hemodynamic instability (10.2% vs 6.1%).
One-Year Risk of Death After ST-segment Elevation Myocardial Infarction With or Without Radial Access
| Without access site in the model, OR (95%CI) | With access site in the model, OR (95%CI) | |
| Age, years | ||
| <50 | 1 | 1 |
| 51-60 | 1.23 (0.42-3.60) | 1.27 (0.41-3.94) |
| 61-70 | 1.82 (0.65-5.08) | 1.95 (0.66-5.70) |
| 71-80 | 3.85 (1.45-10.19) | 4.03 (1.45-11.20) |
| >80 | 6.70 (2.34-19.20) | 6.89 (2.32-20.51) |
| Sex | ||
| Male | 1 | 1 |
| Female | 1.73 (0.97-3.08) | 1.99 (1.10-3.59) |
| Body mass index | ||
| ≥25 | 1 | 1 |
| <25 | 1.60 (0.92-2.76) | 1.51 (0.86-2.65) |
| Hypertension | ||
| No | 1 | 1 |
| Yes | 0.92 (0.52-1.62) | 0.87 (0.49-1.55) |
| Diabetes mellitus | ||
| No | 1 | 1 |
| Yes | 1.53 (0.90-2.58) | 1.64 (0.95-2.81) |
| Tobacco use* | ||
| No | 1 | 1 |
| Yes | 1.55 (0.89-2.72) | 1.67 (0.94-2.96) |
| Dyslipidemia | ||
| No | 1 | 1 |
| Yes | 0.48 (0.28-0.80) | 0.45 (0.26-0.76) |
| Peripheral artery disease | ||
| No | 1 | 1 |
| Yes | 0.31 (0.1-1.13) | 0.29 (0.08-1.13) |
| Chronic kidney disease | ||
| No | 1 | 1 |
| Yes | 1.73 (0.77-3.90) | 2.10 (0.94-4.67) |
| Previous PCI | ||
| No | 1 | 1 |
| Yes | 3.59 (1.44-8.95) | 2.69 (1.05-6.84) |
| Previous AMI | ||
| No | 1 | 1 |
| Yes | 0.68 (0.24-1.97) | 0.78 (0.27-2.23) |
| Affected arteries | ||
| 1 | 1 | 1 |
| 2 | 1.87 (1.11-3.16) | 1.90 (1.11-3.25) |
| 3 | 1.80 (0.98-3.30) | 1.71 (0.92-3.16) |
| Congestive heart failure | ||
| No | 1 | 1 |
| Yes | 2.04 (0.97-4.29) | 1.79 (0.85-3.79) |
| Previous stroke | ||
| No | 1 | 1 |
| Yes | 2.17 (0.94-5.01) | 2.05 (0.88-4.79) |
| Lesion in left main | ||
| No | 1 | 1 |
| Yes | 1.04 (0.65-1.67) | 1.07 (0.66-2.95) |
| Hemodynamic instability | ||
| No | 1 | 1 |
| Yes | 25.37 (13.68-47.03) | 15.86 (8.36-30.09) |
| TIMI flow | ||
| 2-3 | 1 | 1 |
| 0-1 | 1.65 (0.89-3.05) | 1.58 (0.85-3.91) |
| Contact with the health system | ||
| Hospital with PCI | 1 | 1 |
| Outpatient emergency system | 0.79 (0.45-1.36) | 0.72 (0.41-1.27) |
| Hospital without PCI | 0.74 (0.38-1.42) | 0.64 (0.33-1.25) |
| Ischemia time | ||
| <3 h | 1 | 1 |
| 3-6 h | 1.30 (0.72-2.35) | 1.33 (0.72-2.44) |
| 6-12 h | 1.76 (0.92-3.35) | 1.91 (0.98-3.70) |
| >12 h | 0.93 (0.26-3.27) | 0.90 (0.25-3.32) |
| Access type | ||
| Radial | — | 1 |
| Femoral | — | 4.23 (2.51-7.14) |
95%CI, 95% confidence interval; AMI, acute myocardial infarction; PCI, percutaneous coronary intervention; OR, odds ratio; TIMI, Thrombolysis in Myocardial Infarction.
This study shows the importance of the vascular access site to all-cause mortality at 30 days and at 1 year after a PCI procedure for STEMI. For both endpoints, vascular access is the third independent risk factor for mortality, preceded by hemodynamic instability and age, with those individuals undergoing femoral access having 4 or 5 times higher mortality risks than patients undergoing radial access.
These results might be of particular importance when predicting mortality with the available mortality scores. To date, no mortality score has included vascular access type as a predictive variable, which might underestimate the risk of mortality for patients having PCI through femoral access and overestimate the risk of those who have undergone radial access. Although the increase in the C-index is small (a 2%) when vascular access type is included in the model, the discrimination value is extremely good for 30-day mortality (C-index of 0.93). The calibration of the models is poor, though much higher than that observed in the EuroHeart-PCI score.11
In other health settings, such as Scotland,12 choice of vascular access site depends on operator preferences or skills and the use of radial access has increased from 0% in 2000 to 80.5% in 2009. In the EuroHeart-PCI score, which included patients recruited between 2005 and 2008, only 15% of patients received radial access.11 This percentage is not given for the subgroup including only STEMI patients. The variables included in the multivariate model of the EuroHeart-PCI score and in the present model are very similar, and in the case of the EuroHeart-PCI the 3 variables posing the greatest risks are hemodynamic instability followed by age and left main disease. The risks posed by EuroHeart-PCI variables are also very similar to ours. The use of a 30-day mortality endpoint provides a homogeneous follow-up within hospitals and reflects all possible complications that have occurred, not only immediately after STEMI. The effect of vascular access site is lower for 1-year vs 30-day mortality (4.23 vs 5.20), as expected.
The literature points to much better results when using radial access compared with femoral access. Radial access has been shown to have less risk for all-cause mortality (approximately half), fatal or non-fatal myocardial infarction, and fatal or non-fatal stroke at 30 days and at 1 year post-STEMI.12 Similar results were obtained by a meta-analysis of randomized clinical trials by Mamas et al., including in this case major adverse cardiac events.13 The recently published RIFLE-STEACS study has observed that cardiac mortality at 30 days is close to half for patients undergoing radial access and that these patients also have a shorter hospital stay.17 It is necessary to highlight that all clinical trials except the RIFLE study included in that meta-analysis excluded patients with cardiogenic shock and some studies excluded patients older than 75 years. The observed mortality is therefore very low for arms using radial or femoral accesses.
It would have been interesting to have studied specific causes of mortality but this data was not available. In our opinion, all-cause mortality reflects quite well the possible adverse effects of femoral access that sometimes can lead to death. In fact, major bleeding and transfusion after PCI are associated with increased in-hospital stay and 1-year mortality, as observed in the MORTAL study.19 Major bleeding at the access site can lead to hemodynamic instability and blood transfusion with a range of deleterious effects. Radial access has been strongly associated with less risk of major bleeding in many studies, with risks around half or one third when compared with femoral access.14,15,17,20
Since we performed a multivariate analysis, our results should not be affected by other participant characteristics such as hemodynamic instability. We observed a significant additive interaction between hemodynamic instability and vascular access site. This means that the effect of vascular access site differs depending on the presence or not of hemodynamic instability. In the case of 30-day mortality, the interaction between vascular access and hemodynamic instability is statistically significant. In the group of patients without hemodynamic instability, femoral access is associated with a 6-fold higher risk of mortality compared with radial access, whereas the group with hemodynamic instability with the risk is 3.5 times higher with femoral access. At 1 year a similar interaction effect is observed, without reaching statistical significance (data not shown). This interaction was not significant for 1-year mortality in either group. These results could place radial access as the first option even for patients with hemodynamic instability, excluding those where this access cannot be performed for anatomical reasons, hypotension, or operator criteria.
The important shortcoming of the available mortality scores, which do not consider vascular access, shows the need to include this variable when trying to predict all-cause mortality after PCI for STEMI. With the limited sample of the present study, we cannot build a robust score because we cannot construct training and validation cohorts. Although these scores are very similar when predicting mortality,21 their behavior should be tested if the vascular access site is included.
The possible effect of the setting where this study has been performed also should be considered: a) all patients with STEMI in Galicia are transferred directly upon symptoms onset to a PCI-capable hospital, bypassing any closer non-PCI hospital; b) immediately on arrival, they are taken to the catheterization laboratory, without stopping at the emergency department if they have accessed the outpatient emergency system, and c) the availability of radial access as the first option for PCI could have an important positive impact on the overall mortality results after STEMI. This is reflected in the 6.8% rate for 30-day mortality, which includes unstable patients and also elderly patients. The percentage of elderly (25% older than 75 and 10% older than 80) is high in our study, compared to others (12.7% older than 75 in Johnman's et al.12). In-hospital mortality for STEMI patients in EuroHeart-PCI was 5.4% and 30 day all-cause mortality in a Scottish study was 8.5%.12 This relatively low mortality could also reflect that participating operators are skilled in radial access because it has been the first choice for STEMI since 2005 in our region and this study includes patients recruited between 2008 and 2010. The RIVAL study showed that high-volume cath labs using radial access reduced major adverse cardiac events in all patients with acute coronary syndromes, not only in those presenting with STEMI.15 The 2 participating units cover more than 1.5 million inhabitants. Other programs established in other regions have also shown their effectiveness in reducing the attention time and presenting better clinical profiles when patients reach the hospital.22
Strengths and LimitationsThe present study has some advantages. Perhaps the main one is that it was performed in a setting where radial access for STEMI has been the first choice since mid-2005. For those patients with hemodynamic instability, femoral access is usually performed, although radial access is preferred when possible. Another advantage is that we have not excluded any patient due to clinical condition, as has been the case for cardiogenic shock in many clinical trials that are the basis for some mortality scores, undermining their external validity.7,8
This research also has some limitations. Perhaps the most important is that we do not have information on adverse effects directly related to the vascular access. Nevertheless, 30-day and 1-year all-cause mortality are hard variables that integrate all adverse events after PCI and integrate quite well the specific adverse events related to the access site. A further limitation is the sample size, which is too limited to develop a mortality score including the effect of vascular access site. Finally, few patients (n=108) underwent femoral access, although the observed percentage of these patients is to be expected in a clinical setting where radial access is the preferred option for STEMI.
CONCLUSIONSTo conclude, the effect of vascular access site on mortality after a PCI for STEMI is an important variable when predicting mortality risk after this procedure. Radial access should be considered in all hospitals with a cath lab available, and operators should be trained in this procedure. Mortality scores should assess vascular access site as a predictive variable for patients presenting with STEMI.
FUNDINGThis research has been partially funded by the Spanish Ministry of Health, Social Services, and Equality within the framework of the Quality Plan of the National Health Service.
CONFLICTS OF INTERESTNone declared.
We are grateful to María Piñeiro, statistician, for her advice on the interaction assessment.