Keywords
INTRODUCTION
Injury to the coronary microcirculation after acute myocardial infarction (AMI) can occur despite the presence of a patent coronary artery and predicts functional recovery at follow-up.1-3 Microvascular integrity has been measured through intracoronary1-5 or intravenous injections of contrast agents.6-13 Most studies have used a high mechanical index and harmonic gray-scale imaging6 or power Doppler ultrasound.7-13 Real-time myocardial contrast echocardiography (RTMCE) with accelerated intermittent harmonic imaging is a relatively recent method that avoids some of the technical limitations of image acquisition with intermittent harmonic imaging and a high mechanical index.14,15 The aim of this study was to evaluate: a) whether perfusion evaluated with RTMCE predicts recovery of function after AMI, and b) whether the perfusion data are comparable to those obtained with technetium-99m-sestamibi single photon emission computed tomography (SPECT) and magnetic resonance (MR).
PATIENTS AND METHODS
Patients
Eighty-five consecutive patients were included with a first AMI and a moderate probability of having ventricular dyssynergy assessed via clinical and enzymatic parameters. They underwent percutaneous transluminal coronary angioplasty (PTCA) (primary in 60 patients, rescue in 25 patients, and stent implant in 79 patients) which yielded a Thrombolysis In Myocardial Infarction (TIMI) ≥2. The selection criteria for the patients undergoing primary PTCA were characteristic precordial pain over 30 min duration and ST elevation >2 mm in 2 contiguous precordial leads. In patients who underwent rescue PTCA, an increase in creatine kinase (CK) values and/or troponin I greater than twice the normal limit was required.16 The culprit artery causing the AMI was the descending anterior artery in 59 patients, the right coronary artery in 21 patients and the circumflex artery in 5 patients. All the patients gave their informed consent to participate in the study.
Study Protocol
Real-time myocardial contrast echocardiography was done 7±4 days after PTCA. Technetium-99m-sestamibi single photon emission computed tomography or MR with first-pass imaging and delayed hyperenhancement were done at rest in 18 and 32 patients, at an average 30±26 days after AMI, respectively. Echocardiography was done at the same time as myocardial perfusion and at 10±4 weeks later.
Real-Time Myocardial Contrast Echocardiography
A Vivid 5 appliance (GE Medical Systems, Horten, Norway) was used to carry out the RTMCE with pulse inversion harmonic imaging and power Doppler ultrasound. Up to 3 intravenous injections of manually agitated FS-069 were administered slowly (Optison, Molecular Biosystems) and 8 ml of saline serum for 4 min each. Two-, four-,and 5-chamber apical images were acquired.
Power Doppler Ultrasound Controls
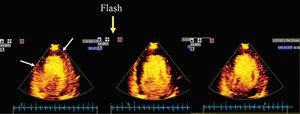
A mechanical index of 0.1 was used throughout the study. The pulse repetition frequency was 2.5 kHz. The frequency of images per second (15.1 ips), dynamic range (6), the power of transmission (-20), gain (20%), image depth (12 cm), wall filter and color scale were kept constant. Focus was placed at the deepest level. When contrast was observed in the myocardial segments the mechanical index was increased to 1.2 ("flash") to ensure that this opacification was really true perfusion (and thus exclude artifacts). In the case of true perfusion, a progressive increase in opacification was observed in the myocardium during the following 3-15 cycles.
Real-Time Myocardial Contrast Echocardiography Analysis
A 16-segment model was used to analyze the RTMCE. Each of the 16 segments was assigned to 1 of the 3 coronary arteries. The RTMCE was scored by 2 observers as follows: 0=absence of perfusion; 0.5=partial perfusion, and 1=complete perfusion. Grade 1 was considered normal and degrees 0.5 and 0 abnormal. An RTMCE index was calculated for each patient according to the score obtained for each dysfunctional segment (hypokinetic, akinetic, or dyskinetic).
Analysis of Wall Motion
A regional (in the region of the culprit artery) and global wall motion index (WMSI) was calculated according to the 16-segment model.17 Each segment was scored as: normal=1; hypokinetic=2; akinetic=3, and dyskinetic=4. The left ventricular ejection fraction and ventricular volumes were measured using apical 2-and 4-chamber views.18 A segment was considered to have improved when it changed from hypokinetic to normal or from akinetic to hypokinetic or normal from the baseline condition until follow-up. With regard to the patients, an improvement in at least 2 hypokinetic segments or 1 akinetic segment was required to be included in the functional recovery group.
Technetium-99m-Sestamibi Single Photon Emission Computed Tomography (SPECT)
A SPECT was carried out in 18 patients at rest. The same 16-segment model was used to compare it to RTMCE. An independent observer for the RTMCE results scored each segment as normal or abnormal.
First-Pass and Hyperenhancement With Delayed Contrast Magnetic Resonance
A first-pass and delayed hyperenhancement study was carried out in 32 patients. During the first-pass study perfusion defects can be produced by a coronary stenosis or by a reduction in microvascular flow,19-20 whereas in gadolinium-delayed hyperenhancement they indicate irreversible damage.21 For MR, the left ventricle was divided into 17 segments (6 basal, 6 mid-cavity, 4 mid-cavity/apical, and 1 apical segment).22
Coronary Angiography
Angiographic data included stent implant, quantitative luminal narrowing after PTCA/stent in the culprit artery, angiographic TIMI flow,23 the presence of collaterals to the culprit artery and the number of diseased vessels (luminal narrowing ≥50%) after revascularization.
Reproducibility of Real-Time Myocardial Contrast Echocardiography
Intraobserver and interobserver concordance for RTMCE was calculated for normal perfusion in the segment (versus abnormal perfusion in 20 randomized patients). Intraobserver concordance was calculated by analyzing the images a second time after at least 60 days. Kappa coefficients are shown.
Statistical Analysis
Standard software was used for statistical analysis (SPSS version 11.5, SPSS Inc., Chicago, Illinois). The mean ± standard deviation (SD) is shown. Student t test was used to compare independent or paired data when required, and χ² test for comparing qualitative data. Receiver operating characteristic (ROC) curves were constructed to define the most precise perfusion values to predict functional recovery. The values of the area under the curve (AUC) are provided. Multivariable logistic regression analysis was carried out with the inclusion of those variables that were significant in the univariable analysis. P-values <.05 were considered significant. The positive predictive value (PPV) and negative predictive value (NPV) were calculated for every cut-off value obtained with the ROC curves for the different techniques (RTMCE, delayed hyperenhanced MR, and SPECT). Positive predictive value (PPV) is defined as the quotient between the number of patients or segments with normal perfusion that recovered at follow-up and the total number of patients or segments with normal perfusion x100. Negative predictive value (NPV) is defined as the quotient between the number of patients or segments with abnormal perfusion that did not improve at follow-up and the total number patients or segments with abnormal perfusion x100. The percentage of concordance and kappa index were used to analyze concordance between the techniques used for segment evaluation. The intraclass correlation coefficient was used (Cronbach α) to determine whether the RTMCE score was similar to that of the SPECT and MR (delayed hyperenhancement).
RESULTS
Patient Characteristics
Follow-up data were available for 82 of the 85 patients (1 cardiac death and 2 untraceable patients). None of the 82 patients suffered events during follow-up. All of them were in a stable clinical condition and were taking platelet aggregation inhibitors, 63 (77%) were taking beta-blockers and 59 (72%), ACE inhibitors. We split the patients into 2 groups according to echocardiography at rest and at follow-up: the functional recovery group (n=49) and the group without functional recovery (n=33). Table 1 shows the clinical and angiographic characteristics, the number of non-perfused/hypoperfused segments and the perfusion index with RTMCE in both groups. The only significant differences we found between groups were the peak CK value and the RTMCE values. Table 2 presents baseline ventricular function data and at follow-up.
Segment Analysis Via RTMCE
In the baseline condition there were 380 dysfunctional segments (180 hypokinetic, 198 akinetic, and 2 dyskinetic) in the region of the culprit artery: 32 could not be evaluated via RTMCE (8%); 211 had normal perfusion; 36, a patchy pattern; and 101, absence of perfusion. Of the 380 dysfunctional segments, 296 corresponded to the anterior descending artery (78%), 63 to the right coronary artery (17%), and 21 to the circumflex artery (5%). At follow-up there were 252 dysfunctional segments in the region of the artery causing the heart attack (114 hypokinetic, 136 akinetic, and 2 dyskinetic). There was a greater proportion of perfused dysfunctional segments that improved at follow-up than perfused or hypoperfused non-dysfunctional segments. Fifty-six percent of the perfused segments, 31% of the segments with patchy perfusion, and 28% of the segments without perfusion recovered (P<.001 between perfused segments and hypoperfused or non-perfused segments). A similar percentage of hypokinetic and akinetic/dyskinetic segments recovered at follow-up (50% vs 39%). The sensitivity, specificity, PPV, NPV, and the diagnostic precision of RTMCE for detecting segment improvement were 74%, 51%, 56%, 71%, and 63%, respectively.
Analysis of Real-Time Myocardial Contrast Echocardiography by Patients
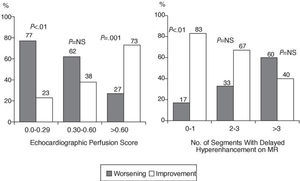
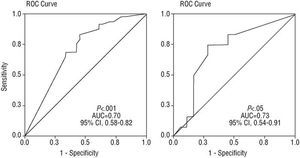
An RTMCE score ≥0.60 was the most precise value to predict regional recovery, with a PPV of 73% and an NPV of 69% (P<.001; AUC=0.70; 95% confidence interval [CI], 0.58-0.82), in the group of patients as a whole. In patients who had an anterior AMI, PPV, and NPV were 81% and 60%, respectively, (P<.01; AUC=0.71; 95% CI, 0.57-0.85). Figure 1 shows the percentage of patients who recovered ventricular function and those who did not according to the different RTMCE scores. A logistic regression analysis was carried out introducing the 2 variables that were significant in the between-group comparison: peak CK value and the RTMCE score. Both were identified as independent predictors of functional recovery: peak CK value (odds ratio [OR] =1.4 per every 1000 U; 95% CI, 1.0-1.9; P<.05); RTMCE score (OR=8.8; 95% CI, 1.9-39.3; P<.01). Figures 2-7 show examples of patients with "poor" and "good" RTMCE scores, respectively.
Fig. 1. Percentage of patients who recovered and who did not recover regional ventricular function at follow-up according to the echocardiographic perfusion score (left) and the number of segments with delayed hyperenhancement under magnetic resonance (right).
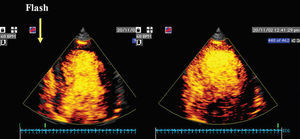
Fig. 2. Patient with "poor" echocardiographic perfusion score ( <0 60 in the region of descending anterior artery notice wide perfusion defect between arrows before and after flash
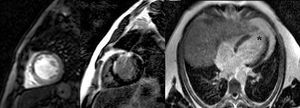
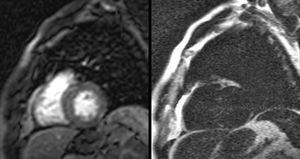
Fig. 3. Magnetic resonance images of the same patient as in Figure 2. A first-pass defect is evident in the intraventricular septum in the short-axis plane (arrows in left-hand image). Delayed hyperenhancement can be observed in the same area in the short-axis image (arrows in the middle image) and in the apical region in a longitudinal view (asterisk in the right-hand image).
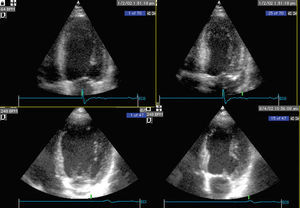
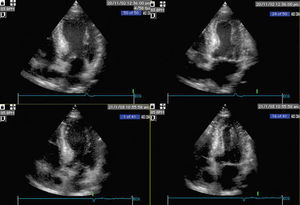
Fig. 4. The same patient as in Figure 2; the lack of recovery of left ventricular function is observed at follow-up. Above: baseline; below: follow-up; left: diastole; right: systole.
Fig. 5. Patient with normal perfusion in the region of the anterior descending artery in the images after the "flash."
Fig. 6. Magnetic resonance images of the same patient as in Figure 5, in which no defects are observed in the first-pass study (left) or in the delayed hyperenhancement (right).
Fig. 7. The same patient as in Figure 5; notice the lack of recovery of left ventricular function at follow-up. Above: baseline; below: follow-up; left: diastole; right: systole.
Technetium-99m-Sestamibi Single Photon Emission Computed Tomography and MR Data
Tables 3 and 4 show the perfusion score and the number of segments with perfusion defects with SPECT and MR in both groups of patients. The finding of 4 or fewer perfusion defects with SPECT had a PPV of 85% and NPV of 100% for recovery of t he left ventricular regional function (P<.01; AUC=0.82; 95% CI, 0.53-1.10). Regarding MR, 47% of the patients had a segment with a first-pass perfusion defect, and 65% one with delayed hyperenhancement. Ninety-four percent of the patients with a first-pass defect also had delayed hyperenhancement in the same region, and the correlation between the number of segments with a first-pass defect and delayed hyperenhancement was significant (r=0.64; P<.001). However, the number of segments with a first-pass defect was of no use in differentiating the patients who recovered from those who did not. In contrast, the number of segments with delayed hyperenhancement was greater in those who did not recover regional function. Findings of delayed hyperenhancement in less than 4 segments had a PPV of 80% and an NPV of 63% (P<.05; AUC=0.73; 95% CI, 0.54-0.91) for regional function recovery, whereas a score for the transmural extent of delayed hyperenhancement <1 6 had a ppv of 81 and an npv 64 P<.05; AUC=0.71; 95% CI, 0.52-0.91). Figure 1 shows the percentage of patients who recovered ventricular function and those who did not according to the number of segments observed with delayed hyperenhancement under MR. Figure 8 shows ROC curves for RTMCE and the MR (number of segments with delayed hyperenhancement).
Fig. 8. Receiver operating characteristic curves for prediction of recovery of regional function according to echocardiographic perfusion (left) and the number of segments with delayed hyperenhancement under magnetic resonance (right). CI indicates confidence interval.
Comparison Between Real-Time Myocardial Contrast Echocardiography and Technetium-99m-Sestamibi Single Photon Emission Computed Tomography
The concordance between RTMCE and SPECT for the detection of abnormal perfusion versus normal perfusion in an analysis of the dysfunctional segments was 78% (P<.001; κ=0.49), with a significant intraclass correlation in the perfusion scores with both techniques (α=.79; P<.01; 95% CI, 0.45-0.92).
Comparison Between Real-Time Myocardial Contrast Echocardiography and 99mTc-Sestamibi Single Photon Emission Computed Tomography
During an analysis of the dysfunctional segments, concordance between RTMCE and the findings of delayed hyperenhancement under MR was 70% (P<.001; κ=0.35), although we did not find any intraclass correlation between the RTMCE score and the score for the transmural extent of delayed hyperenhancement (α=.2; P=.7; 95% CI, 1.6 to 0.42).
Reproducibility of Real-Time Myocardial Contrast Echocardiography
The concordance between observers for the definition of a segment with normal or abnormal perfusion via RTMCE was 89% (P<.001; κ=0.70), and 92% for intraobserver concordance (P<.001; α=0.75).
DISCUSSION
The main points of interest in this study are: a) it was done with a broad series of patients with "reperfused" AMI (patent artery and TIMI flow ≥2), and b) it was compared with an innovative technique to study function and perfusion after AMI, such as MR. The main findings were:
1. Real-time myocardial contrast echocardiography is of moderate value to predict recovery of left ventricular function after AMI in an analysis by patient.
2. The RTMCE and the CK values have independent prognostic value for the recovery of left ventricular function.
3. The RTMCE is in moderate agreement with SPECT, but less so with the delayed hyperenhanced magnetic resonance study in AMI patients.
Most studies with perfusion echocardiography which have focused on the recovery of left ventricular function after AMI have used harmonic imaging with a high mechanical index,10-13 whereas only a few have used a low mechanical index with a high frequency of images per second.24-26 Intermittent harmonic imaging with a high mechanical index can be more sensitive, but is technically more difficult to carry out and normally requires higher doses of contrast agents.
Predictive Value of Real-Time Myocardial Contrast Echocardiography
A low PPV for RTMCE has been previously described regarding functional recovery after AMI, and our study confirms this.24,25 In the present article, RTMCE was carried out at least 2 days after AMI (mean, 7±4 days). It has been demonstrated that performing RTMCE earlier after AMI can cause underestimations of the actual area of hypoperfusion due to reactive hyperemia.27 Thus, the time to carry out RTMCE appears to be correct for PPV. However, the NPV obtained in our series was smaller than that reported in other studies. There might be different reasons for the false negative perfusion defects:
1. The time at which the RTMCE was carried out. If we had done the RTMCE later after the AMI, we would probably have achieved better results for the NPV. Some studies have reported a progressive improvement in the perfusion indexes due to recovery of microcirculation during the first months after AMI, which suggests the existence of recovery of microvasculature in some patients.28-30
2. On the other hand, the artifacts caused by attenuation and shadow due to the costal bones can explain some of the false negative defect.
3. Finally, in some cases, an insufficient quantity of the contrast agent may have been injected or it may have undergone massive destruction.
Technetium-99m-Sestamibi Single Photon Emission Computed Tomography and Magnetic Resonance
Technetium-99m-sestamibi single photon emission computed tomography and MR were done on the average 4 weeks after RTMCE, which means that some perfusion defects observed in RTMCE might have recovered by the time SPECT or MR were done. Despite this, the concordance with SPECT was reasonable and suggested that RTMCE might be clinically useful to evaluate myocardial perfusion.
Previous studies have already reported a highly predictive value for SPECT for the recovery of left ventricular function after AMI,31 as was found in our study. On the other hand, MR has not been widely studied. The first-pass defects that indicate coronary or microvascular obstruction have been associated with the lack of recovery of function in patients with AMI who underwent percutaneous revascularization.19 In our study, first-pass defects were less frequent than delayed hyperenhancement, probably due to the elapsed time between the AMI and the MR study compared to RTMCE. The first-pass defects were not associated with the lack of functional recovery. However, the delayed hyperenhancement in the area of the infarction was usually observed in the group without functional recovery and was related to the lack of recovery, which was more probable the greater the intramural extent of the defect. A cut-off value of 37% for intramural extension had high sensitivity and specificity for the detection of viable myocardium in a previous study.32 In our study, a cut-off value of 1.6 for the extension of the delayed hyperenhancement score had a PPV of 81% for the recovery. Delayed hyperenhancement indicating fibrosis has been associated with the lack of recovery in patients with chronic myocardial dysfunction who had undergone revascularization20,21,33 and in patients after AMI34 It is also strongly correlated with viability determined via 18F-fluorodeoxyglucose positron emission tomography (PET).32
Limitations
Segment analysis was similar with RTMCE and SPECT, but not with MR, due to the different segment configuration of the latter technique. The calculation of the baseline global and regional ventricular function and at follow-up was made through echocardiography for practical reasons. Although the reproducibility of MR is greater than that of echocardiography (<4% vs <10%),35 both the calculation of the ejection fraction and the volumes and the regional wall motion index with harmonic imaging have been satisfactorily correlated with MR and with gated-SPECT in several studies.36,37
We have already highlighted that SPECT and MR were done relatively late compared with RTMCE. Only a minority of the patients underwent SPECT and relatively few underwent MR, which means that we might have obtained extreme results.
We carried out an analysis based on the patient and an analysis based on the dyssynergic regions. From a practical standpoint, the first type of analysis seems more suited to the aim of knowing which patient has a greater probability of improving depending on the amount of non-perfused or hypoperfused myocardium. However, this aim would have had more impact if we had st (e.g. only patients with anterior AMI and/or rescue PTCA).
Systematic coronary angiography was not done during follow-up, which means that we cannot exclude the probability of restenosis. However, the possibility of restenosis in the artery causing the heart attack at 2 months is relatively low.
Previous studies have described the drawbacks of RTMCE to suitably study the anterior and lateral wall of the left ventricle.27 A poor lateral window might prevent the study of perfusion defects when the circumflex artery is causing the infarct, as occurred in three of our patients. Attenuation of the anterior wall could have impeded the study of perfusion at that level in patients with extensive infarcts due to the anterior descending artery, although the majority of anterior infarcts affected only or mainly the septoapical region.
CONCLUSIONS
Real-time myocardial contrast echocardiography carried out before hospital discharge has a moderate predictive value for functional recovery after reperfused AMI. The RTMCE and SPECT findings were in agreement, but less so with those of MR. However, the delayed hyperenhancement findings had a reasonable PPV for functional recovery. The relative value of RTMCE and MR after AMI remains to be determined, as well as the time after the acute event when such explorations should be carried out.
Correspondence: Dr. J. Peteiro.
Ronda, 5, 4.º izqda. 15011 A Coruña. España.
E-mail: pete@canalejo.org