Frailty is an age-associated clinical syndrome characterized by a decrease in physiological reserve in situations of stress, constituting a state of vulnerability that involves a higher risk of adverse events. Its prevalence in Spain is high, especially in elderly individuals with comorbidity and chronic diseases. In cardiovascular disease, frailty is associated worse clinical outcomes and higher morbidity and mortality in all scenarios, in both acute and chronic settings, and could consequently influence diagnosis and treatment. However, frailty is often not addressed or included when planning the management of elderly patients with heart disease. In this article, we review the available scientific evidence and highlight the most appropriate scales for the measurement and assessment of frailty, some of which are more useful and have better predictive capacity than others, depending on the clinical context. We also underline the importance of properly identifying and assessing frailty in order to include it in the treatment and care plan that best suits each patient.
Keywords
The concept of frailty is increasingly considered in the study and treatment of elderly patients with cardiovascular disease (CVD), albeit not always consistently.1 Because of the combination of societal aging in developed countries and advances in the treatment of the major forms of heart disease, most CVD hospital admissions occur in individuals older than 65 years and CVD is the main cause of death in persons older than 75 years. Most clinical trials do not include elderly patients, and those that do have not assessed frailty. There is therefore little scientific evidence available on improving the treatment and care of frail elderly patients with heart disease. This situation has prompted several scientific societies to prioritize research into frailty in elderly heart disease patients in order to define its prognostic significance and identify the best treatment interventions in different clinical contexts.2
DEFINING FRAILTY AND THE IMPORTANCE OF ITS ASSESSMENTFrailty is a syndrome characterized by a decrease in biological reserve during aging. It is produced by the declining function of the body's physiological systems, leaving the individual especially vulnerable to any stressful situation, and is considered an indicator of a person's biological age.3 Among persons older than 65 years living in the community (not institutionalized) and with no disability, the prevalence of frailty ranges from 4% to 14% in several European countries; however, in Spain the prevalence is 21%.4 Frailty is more frequent among patients with CVD, and these 2 conditions are reciprocally related: frail individuals are at higher risk of CVD, and people with clinical or subclinical CVD are at higher risk of a decline in physical function.5
Clinical outcomes of CVD tend to be worse among frail individuals,6 who have higher morbidity and mortality in all acute and chronic clinical scenarios, as detailed in this review. The Canadian Study of Health and Aging reported adjusted 5-year mortality risk values of 4.8 (95% confidence interval, 3.7-6.2) for moderately frail individuals and 7.3 (95% confidence interval, 4.7-11.4) for those with severe frailty.7 Among CVD patients, the Cardiovascular Health Study found a similar association of prefrail and frail status with falls, functional impairment, hospitalization, and mortality over a 3- to 7-year follow-up.8
Finally, frailty is a much stronger predictor than comorbidity of new disability, especially with increasing age.9
Frailty is distinct from comorbidity and disability.8 Comorbidity is defined as the co-occurrence of diseases that can alter the treatment or clinical course of the index disease. Comorbidity does not necesarily imply fraility, although frailty is more frequent in patients with high comorbidity, and therefore its cause should always be assessed. Disability is an impairment that limits a person's ability to carry out daily activities. Frailty can be understood as a predisability state (physical frailty) or as an accumulation of deficits that define a vulnerable status (multidimensional frailty). Frailty should therefore be viewed as one of the main factors associated with advserse outcomes, and as such can be extremely useful in clinical decision-making and in the design of individualized care plans.
MEASURING FRAILTYThere are 2 main approaches to the characterization of frailty. The first views frailty as a phenotype of poor physical function (physical frailty), and is heavily reliant on 2 objective parameters: grip strength and gait speed. The most widely used measure of physical frailty is the Fried scale, which was described and validated in the Cardiovascular Health Study,8 The Fried scale defines frailty as the presence of 3 or more of the following factors, with the presence of 1 or 2 factors indicating a prefrail state:
- 1.
Unintentional weight loss > 4.5kg or> 5% in the last year
- 2.
Self-rated exhaustion in the previous week, assessed from the responses to 2 statements in the Center for Epidemiological Studies-Depression (CES-D) scale:
- –
Did you feel that everything you did was an effort?
- –
Did you feel that you could not get going?
The responses can be a) rarely or none of the time (< 1 day)=0; b) 1 or 2 days=1; c) 3 or 4 days=2; or d) most or all of the time=3. A response scoring ≥ 2 to either question is considered a positive frailty indicator.
- –
- 3.
Weakness, determined from the maximum grip strength measured with a dynamometer and adjusted for sex and body mass index (BMI). The patient should be seated and preferably use his or her dominant arm, with the elbow at 90°. The patient makes 3 attempts separated by 1minute, and the highest score is used. In men, the cutoff values for different BMI categories are as follows: BMI ≤ 24, grip strength ≤ 29; BMI ≤ 28, grip strength ≤ 30; and BMI> 28, grip strength ≤ 32. For women, the cutoffs are BMI ≤ 23, grip strength ≤ 17; BMI 23.1-26, grip strength ≤ 17.3; BMI 26.1-29, grip strength ≤ 18; and BMI> 29, grip strength ≤ 21.
- 4.
Low gait speed, measured as the time taken to walk 4.57 meters at usual speed, adjusted for sex and height. The cutoffs for a low gait speed for men are ≥ 7sec for height ≤ 173cm and ≥ 6 s for height> 173cm; for women, the criteria are ≥ 7sec for height ≤ 159cm and ≥ 6sec for height> 159cm.
- 5.
Low physical activity, estimated as the weekly energy expenditure. The cutoff values are <383kcal/wk for men and <270kcal/wk for women. These figures correspond to <2.30h/wk for men and <2h/wk for women spent walking or in another activity such as swimming, cycling, or tennis.
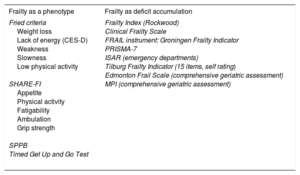
To improve applicability to specific clinical scenarios, other scores have been proposed based on the frailty phenotype or some of its properties (Table 1).10 The SHARE-FI index is based on the Fried criteria and assesses 4 self-reported items and grip strength measured with a dynamometer.
The Most Widely Used Frailty Indices in Cardiology, Grouped According to the 2 Main Conceptions of Frailty
| Frailty as a phenotype | Frailty as deficit accumulation |
|---|---|
| Fried criteria Weight loss Lack of energy (CES-D) Weakness Slowness Low physical activity SHARE-FI Appetite Physical activity Fatigability Ambulation Grip strength SPPB Timed Get Up and Go Test | Frailty Index (Rockwood) Clinical Frailty Scale FRAIL instrument: Groningen Frailty Indicator PRISMA-7 ISAR (emergency departments) Tilburg Frailty Indicator (15 items, self rating) Edmonton Frail Scale (comprehensive geriatric assessment) MPI (comprehensive geriatric assessment) |
CES-D, Center for Epidemiological Studies-Depression; MPI, Multidimensional Prognostic Index; SPPB, Short Physical Performance Battery.
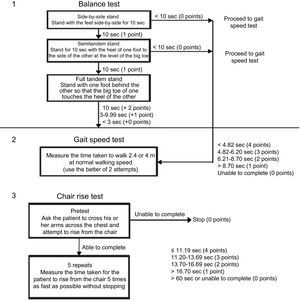
The recommended physical performance test for frailty in clinical trials is the Short Physical Performance Battery (SPPB) (Committee for Medicinal Products for Human Use, European Medicines Agency, 2015). The SPPB tests 3 parameters: balance, gait speed, and the ability to stand unaided from a chair 5 times (Figure 1).
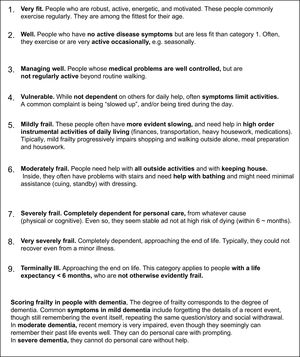
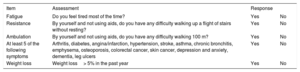
Whereas the physical frailty approach views frailty as a state preceding dependency, the second approach (multidimensional frailty) views frailty as the consequence of an accumulation of deficits including comorbidities, disabilities, symptoms, and laboratory results associated with poor outcomes. The measurement of multidimensional frailty thus includes comorbidity and dependency. The Frailty Index views frailty as a continuum and assesses more than 70 deficits to calculate a ratio of deficits present to the total number of deficits assessed, thus producing a score between 0 and 1.11 A derivative of the Frailty Index is the Clinical Frailty Scale (CFS), which is a screening tool based on the clinical judgment of the attending health care professional (Figure 2).12 The deficit accumulation approach is also used in the Electronic Frailty Index, which forms part of digital patient records in the United Kingdom and is used in the assessment of all elderly patients awaiting surgery.13 Another screening tool developed for the general population is the FRAIL Scale; this simple-to-use scale takes less than 2minutes to complete as it consists entirely of questions to the patient, with no physical or laboratory tests (Table 2).14
Clinical Frailty Scale. Reproduced with permission from Rockwood et al.12.
FRAIL Scale (Frailty Diagnosed if 3 or More of the Following 5 Criteria Are Met)
| Item | Assessment | Response | |
|---|---|---|---|
| Fatigue | Do you feel tired most of the time? | Yes | No |
| Resistance | By yourself and not using aids, do you have any difficulty walking up a flight of stairs without resting? | Yes | No |
| Ambulation | By yourself and not using aids, do you have any difficulty walking 100 m? | Yes | No |
| At least 5 of the following symptoms | Arthritis, diabetes, angina/infarction, hypertension, stroke, asthma, chronic bronchitis, emphysema, osteoporosis, colorectal cancer, skin cancer, depression and anxiety, dementia, leg ulcers | Yes | No |
| Weight loss | Weight loss> 5% in the past year | Yes | No |
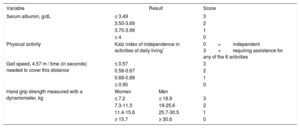
The ISAR (Identification of Seniors at Risk) scale includes 6 questions and has been used to screen for frailty in the emergency setting; this scale can help in the selection of patients likely to benefit from a geriatric assessment (Table 1).15 In certain specific clinical contexts, disease prediction scales have been developed that include clinical and analytical parameters together with measures of physical function. Examples are the Green score (Table 3), developed for the assessment of patients with aortic stenosis (AS), and the Essential Frailty Toolset, which predicts poor outcome among patients with severe AS awaiting transcatheter aortic valve implantation (TAVI). These instruments have not been validated as frailty scales against a reference geriatric assessment measure in the general population; however, they have proved useful in specific clinical contexts, as described below.
The Green Score
| Variable | Result | Score | |
|---|---|---|---|
| Serum albumin, g/dL | ≤ 3.49 | 3 | |
| 3.50-3.69 | 2 | ||
| 3.70-3.99 | 1 | ||
| ≥ 4 | 0 | ||
| Physical activity | Katz index of independence in activities of daily living* | 0=independent 3=requiring assistance for any of the 6 activities | |
| Gait speed, 4.57 m / time (in seconds) needed to cover this distance | ≤ 0.57 | 3 | |
| 0.58-0.67 | 2 | ||
| 0.68-0.89 | 1 | ||
| ≥ 0.90 | 0 | ||
| Hand grip strength measured with a dynamometer, kg | Women | Men | |
| ≤ 7.2 | ≤ 18.9 | 3 | |
| 7.3-11.3 | 19-25.6 | 2 | |
| 11.4-15.6 | 25.7-30.5 | 1 | |
| ≥ 15.7 | ≥ 30.6 | 0 | |
*The Katz index is a simple scale composed of 6 items that evaluate basic daily activities to provide a measure of independence. It allows a general assessment of a patient's functional state, comparison of individuals and groups, and the detection of changes over time.
Implementation of these scales in daily clinical practice is not straightforward, as some of them are time consuming or not feasible in an acute setting. In simple terms, scales based on physical frailty (presence of the frailty phenotype) should be used for patients with no established disability, whereas scales based on multidimensional frailty (deficit accumulation) are valid for patients with any level of disability, although they are more suited to patients with moderate-to-advanced disability. In acute situations, the most suitable scales are those that rely on self rating or the clinical judgment of the attending health care professionals.16 Numerous studies have demonstrated the usefulness of these instruments in a variety of contexts, but none provides sufficient sensitivity or specificity for the individualized identification of frailty in a given patient and a specific clinical context.17
The most widely validated assessment in clinical practice and with the strongest evidence of benefit is the Comprehensive Geriatric Assessment (CGA).18 This index uses clinical, functional, cognitive, social, and nutritional assessments by different professionals for the design of a treatment and management plan. The CGA is the best diagnostic tool for frailty and provides both an overview and a complete situational diagnosis. The systematic use of the CGA increases an elderly individual's chances of long-term survival and home living after hospital discharge.18 The main limitations of the CGA are that it is time consuming and requires specialized personnel. To circumvent these limitations, scales derived from the CGA have been developed to enable nongeriatric physicians to conduct an abbreviated assessment; examples are the Multidimensional Prognostic Index and the Edmonton Frail Scale (EFS).
FACTORS TO BE CONSIDERED IN RELATION TO FRAILTY ASSESSMENT IN DIFFERENT SCENARIOSThe following factors need to be considered:
- •
Frailty should be distinguished from comorbidity and disability.
- •
Ideally, frailty should be measured in the community, so that the evaluation is available to medical teams should the patient attend hospital or experience an acute event.
- •
Frailty in patients with no severe disability can potentially be prevented or even reversed to some degree through the control of specific diseases, a medication review, specific nutritional interventions, or personalized exercise programs.
- •
The absence of severe disability does not contraindicate intervention. The frail elderly individual with CVD has a high risk of mortality, morbidity, and medical complications. Diagnostic and therapeutic decision making should involve specialists from multiple disciplines and take account of patient values and preferences. The detection of frailty always identifies a patient who will require close monitoring and early intervention in modifiable characteristics in order to improve outcomes.
Most (80%) of heart failure (HF) patients are older than 65 years, and diagnosis frequently occurs in individuals older than 80 years.19 In the treatment of elderly patients, it is important to consider not only patient age, but also the presence of other factors associated with a poor prognosis, such as comorbidities and geriatric syndromes,6,8,20 depression,21 and cognitive impairment.22 These patients also have a high level of dependency in daily activities.
Frailty is highly prevalent in HF patients20,23; among elderly HF patients in the Cardiovascular Health Study, the frailty prevalence rate was 7.5 times higher than in the general population,24 and frailty is associated with a higher risk of a worsening functional class and a doubling of the risk of readmission and in-hospital death.25
The most widely used criteria for identifying frailty in HF patients are the Fried criteria (Table 1). Nonetheless, the CFS (Figure 2) has been demonstrated to predict institutionalization and mid-term mortality, even in hosptitalized patients.12,26 Due to its ease of use and and prognostic value, the CFS is recommended for the assessment of frailty in elderly HF outpatients.
Frailty assessment can guide important clinical decisions by providing a greater understanding of the patient's vulnerability and risk level.27 There is also emerging evidence that frailty can be modulated, to the extent that the frailty phenotype in younger HF patients can to some extent be a consequence of the disease itself and thus could be reversed with advanced therapies such as circulatory support devices or heart transplant.28 The extent to which improvements of this type are possible in frail elderly patients is uncertain; however, these data underline the importance both of optimizing HF therapy and of conducting a multidimensional frailty assessment in elderly HF patients that addresses geriatric syndromes, which can be reversed, at least in part.
Acute Heart FailureThe prevalence of frailty among acute HF patients ranges from 50% to 70%,29–32 and frailty in these patients is associated with adverse outcomes in the short- and long-term.29,31,33,34 There are no established guidelines on the best tool or timing for frailty diagnosis in elderly patients with acute HF not previously assessed as frail.35 The identification of frailty during the acute phase could help in risk stratification, decision-making about hospital admission, and the design of an individualized patient care plan.36 The question of individualized patient care programs is important because 1 in 4 patients treated for acute HF at Spanish hospitals is discharged home.37 However, frailty assessment in the acute phase is not straightforward due to the difficulty of calculating some scores (especially for scales involving physical performance tests) and the lack of both time and an appropriate space in which to carry out the assessment. Given these concerns, in the acute phase it is more practical to use scales based on self rating or the clinical judgment of the attending health care personnel, postponing objective physical performance tests until the patient's clinical situation has stabilized.36 A number of fast and simple scales are available that could be suitable for use in the acute phase; however, evidence for their applicability in acute HF is lacking. One self-rating frailty scale based on the Fried criteria has proved useful in the emergency department setting for the identification of increased 30-day mortality risk among acute HF patients aged 65 years or older who have no established severe disability.38
Other scales, such as the FRAIL Scale39 (Table 2), combine self-rating questionaires based on the Fried criteria with assessment of comorbidity, whereas others are based on deficit accumulation; for example, ISAR, CFS,12,15 and TFI (Tilburg Frailty Indicator).40
Frailty prevalence and its prognostic repurcussions have also been evaluated during and immediately following hospitalization for HF; however, to date no consensus has been reached on which index provides the most effective measure of frailty in this setting. Most studies have adopted the frailty phenotype approach, using the Fried criteria31,32,41 or physical performance tests such as the SPPB.29,34 Some authors have also drawn a clear distinction between frailty and disability, excluding patients with moderate or severe dependency in order to ensure assessment of frailty as an independent risk marker.31 Frailty measured using these approaches has been associated with an increased risk of 1-year mortality and also of readmission and incident disability or functional decline.31,41 This relationship is maintained after adusting for associated disability, comorbidity, and HF severity.
Some studies have also assessed the independent prognostic value of individual frailty phenotype components in HF patients. The frailty parameters shown to independently predict death and rehospitalization due to HF are physical inactivity31,41 and a mean gait speed <0.6 m/sec.31,42
The Fried criteria provide the best measure of frailty defined as a predisability risk state, and it is thus appropriate to use this scale once the acute sypmtoms have stabilized and it is safe for the patient to carry out the physical performance tasks, either in the final days of hospitalization or after discharge. For HF patients with moderate or severe dependency, it may be appropriate to use more general scales, such as the CFS, or indices based on a comprehensive geriatric assessment, such as the MPI.43 These approaches can help in the organization of health care resources, especially for advanced disease stages.
Acute Coronary SyndromeFrailty Assessment in the Acute Phase of Acute Coronary SyndromeAmong patients with acute coronary syndrome (ACS), frailty is associated with high incidences of complications, in-hosptital mortality, and readmission; moreover, patients meeting frailty criteria are often excluded from recommended treatments and invasive strategies.43-54 However, it unknown whether the prognosis associated with frailty can be modified, and there is no established basis for deciding how the presence of frailty should inform treatment. There is therefore controversy regarding the prognostic impact of invasive strategies in elderly ACS patients without ST-segment elevation who meet frailty criteria. It has been proposed that percutaneous revascularization could be especially beneficial in frail non–ST-segment elevation ACS patients55; however, evidence is scarce because these patients are systematically excluded from clinical trials and there are currently no randomized trials in frail patients.56 An independent association has been reported between frailty and the appearance of bleeding complications during hospitalization for ACS57; however, these complications could simply reflect the higher level of comorbidity in frail patients, and geriatric assessment therefore appears to contribute little to the prediction of bleeding risk.58
The acute phase of ACS is presumably preceded by frailty; however, frailty assessment is impeded by the acute disease, the potential need to immobilize the patient, and interference from equipment, such as monitor cables, cannulas, and catheters. Therefore, frailty should be assessed on admission using simple and rapidly completed scales that do not involve physical tests. The most practical scales in this situation are probably the FRAIL Scale14 and the CFS.44 The FRAIL Scale (Table 2) predicts a poor prognosis independently of the GRACE scale and chronological age.52 Frailty assessed by the CFS (Figure 2) has shown a consistent association with short-term and mid-term mortality and with conservative treatment.44,45
Frailty Assessment After the Acute Phase of Acute Coronary SyndromeA more complete frailty assessment that includes parameters requiring ambulation can be conducted in stable patients 24 to 48hours after the onset of ACS. Such an assessment should provide a more precise picture of frailty and mid-term prognosis, thus supporting decision-making about elective interventions (eg, revascularization and rehabilitation). The following frailty indices are appropriate for this phase:
- 1.
SHARE-FI. Frailty measured with this scale is associated with the incidence of early complications, short-term and mid-term survival, and initially conservative therapy.48,57 If a dynamometer is available, the SHARE-FI provides an alternative to the scales described above for the early assessment of frailty.
- 2.
The Fried criteria. This scale is used extensively wth ACS and ischemic heart disease patients undergoing coronary revascularization. The Fried score is an acceptable predictor of short-term and mid-term mortality.47
- 3.
The Green score. This scale is a better risk predictor than the Fried criteria in ACS patients.46,53
- 4.
Gait speed. This physical test is classed as a moderately complex frailty index because it requires the patient to be clinically stable and independent. Gait speed is one of the Fried criteria but has significant predictive value when used alone. Slow gait speed is an independent predictor of mid-term mortality in myocardial infarction patients.49
- 5.
The EFS. This moderately complex multidimensional scale can be completed in approximately 5minutes. A free iOS-compatible tablet application is available to help with data collection. Frailty measured with the EFS is associated with mid-term and long-term mortality in ACS patients.50,51
The main characteristics and applications of these frailty indices are summarized in Table 4. In general, complex scales tend to have more predictive capacity than simpler ones. Thus, in patients no longer in the acute phase, it may be beneficial to use scales that include physical tests or laboratory parameters. Nevertheless, it remains unclear whether frailty should be assessed on admission, during hospitalization, or after discharge or whether assessment at various times would provide additional information.
Characteristics and Requirements of Different Frailty Assessment Indices and Evidence for Their Usefulness in Acute Coronary Syndrom Patients
| Phase and index | Simplicity | Physical tests | Laboratory tests | Evidence for usefulness in ACS |
|---|---|---|---|---|
| Acute phase | ||||
| FRAIL Scale | +++ | – | – | ++ |
| Clinical Frailty Scale | ++ | – | – | +++ |
| SHARE-FI | ++ | +* | – | ++ |
| Stable phase | ||||
| Fried criteria | ++ | + | – | +++ |
| SHARE-FI | ++ | + | – | ++ |
| Green score | + | + | + | ++ |
| Edmonton Frail Scale | ++ | + | – | ++ |
| Gait speed | ++ | + | – | + |
ACS, acute coronary syndrome.
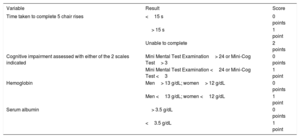
Although there has been no published validation in elderly AS patients, our view is that the FRAIL Scale (Table 2) is potentially useful for an initial assessment. Frailty assessed with the Fried criteria (Table 1) is associated with mortality in AS patients59 and with readmission to rehabilitation centers after TAVI.60 The CFS (Figure 2) predicts mortality after TAVI61; however, doubts have been raised about reproducibility due to its subjective input, which necessitates diligent assessor training. The more recent Essential Frailty Toolset (Table 5) includes a short physical test called the Mini Mental State Examination as well as measures of hemoglobin and albumin. While this scale is more complex, in elderly patients with severe AS undergoing aortic valve replacement, it has shown a superior predictive capacity than other frailty scales (Fried, Fried+, Rockwood, SPPB, Bern, and Columbia).62 The Green score (Table 3) is more complex as it includes 2 physical tests, the Katz index, and a blood parameter. Frailty assessed with the Green score is strongly associated with 1-year mortality in AS patients undergoing TAVI.63
Essential Frailty Toolset
| Variable | Result | Score |
|---|---|---|
| Time taken to complete 5 chair rises | <15 s | 0 points |
| > 15 s | 1 point | |
| Unable to complete | 2 points | |
| Cognitive impairment assessed with either of the 2 scales indicated | Mini Mental Test Examination> 24 or Mini-Cog Test> 3 | 0 points |
| Mini Mental Test Examination <24 or Mini-Cog Test <3 | 1 point | |
| Hemoglobin | Men> 13 g/dL; women> 12 g/dL | 0 points |
| Men <13 g/dL; women <12 g/dL | 1 point | |
| Serum albumin | > 3.5 g/dL | 0 points |
| <3.5 g/dL | 1 point |
The frailty indices most widely studied in patients with severe AS are gait speed and the SPPB (Figure 1). Both measures are of low-to-intermediate complexity, are objective and reproducible, and can be completed in under 5min. Moreover, in elderly patients with severe AS, frailty assessed with the SPPB shows a correlation with systolic dysfunction and coronary and cerebrovascular disease.64 Low gait speed over 5 meters correlates with mortality after TAVI.65 Comorbidity is closely associated with frailty and is an indicator of poor prognosis in elderly severe AS patients66 and is of low benefit from interventional aortic valve therapy.67,68
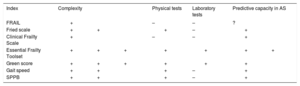
The advantages and disadvantages of the main frailty indices and their prognostic value in elderly severe AS patients are summarized in Table 6. The best evidence available supports the use of the Fried scale, the Essential Frailty Toolset, and the SPPB and gait speed physical performance tests.
Advantages and Disadvantages of Frailty Indices in Patients With Aortic Stenosis
| Index | Complexity | Physical tests | Laboratory tests | Predictive capacity in AS |
|---|---|---|---|---|
| FRAIL | + | – | – | ? |
| Fried scale | ++ | + | – | + |
| Clinical Frailty Scale | + | – | – | + |
| Essential Frailty Toolset | +++ | + | + | ++ |
| Green score | +++ | + | + | + |
| Gait speed | ++ | + | – | + |
| SPPB | ++ | + | – | + |
AS, aortic stenosis; SPPB, Short Physical Performance Battery.
The available evidence reveals a prognostic impact of frailty in distinct CVD scenarios. Several valid frailty scales are available; however, some are more useful than others or have a higher predictive capacity in specific clinical scenarios. Frailty can limit patients’ diagnostic and therapeutic options, and it is therefore of paramount importance that health care professionals be able to identify its presence and establish an individualized and specific care and management plan adapted to each patient. Due to the characteristics of the treated population, this is especially important in cardiology services.
In summary, frailty is associated with poor prognosis in elderly patients with heart disease and should be assessed systematically. Planning the care of elderly patients requires an understanding of frailty by both health care personnel and family members and carers.
CONFLICTS OF INTERESTNone declared.