In recent years, secondary prevention strategies for acute coronary syndrome (ACS) have focused on reducing plasma levels of low-density lipoprotein cholesterol (LDL-C).1 Total cholesterol, however, in addition to LDL-C, is composed of high-density lipoprotein cholesterol (HDL-C), which is rich in apolipoprotein A-I, and other low-density lipoproteins (known as remnant cholesterol or triglyceride-rich lipoproteins [TRLs]), which contain apolipoprotein B-100 and apolipoprotein B-48.2 Plasma triglyceride levels >260mg/dL result in increased TRLs, which have been linked to an increased cardiovascular risk, although the evidence is less robust in this area than it is for LDL-C.2
The aim of this study was to assess the likelihood of ACS recurrence within 12 months of the index event according to TRL levels during hospitalization. We conducted a retrospective study of all consecutive patients admitted to a tertiary hospital for ACS between January 1, 2013 and December 31, 2017. We analyzed sociodemographic variables, cardiovascular risk factors, atrial fibrillation, chronic obstructive pulmonary disease, chronic kidney disease, coronary revascularization procedure, left ventricular ejection fraction, and medical treatment on discharge. Lipid profiles during the first 72hours of admission were evaluated in all patients known to have fasted for at least 12hours. We also calculated TRL levels, defined as total cholesterol minus HDL-C and LDL-C, and non–HDL-C. TRLs and non–HDL-C were defined dichotomously on the basis of median values for the sample. Both were nonnormally distributed continuous quantitative variables.
Study variables were compared between patients with and without a new coronary event. The t test was used for quantitative variables and the chi-square test for qualitative variables. Variables with significant differences (P<.05) in the univariate analysis were analyzed by multivariable logistic regression. Statistical analyses were performed in the Stata statistical software package (release 14, StataCorp LP). The study was approved by the local ethics committee. Due to the retrospective study design and the anonymous nature of the data, informed consent from patients was not deemed necessary.
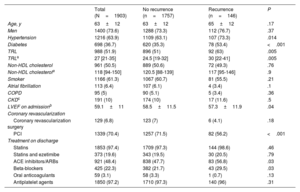
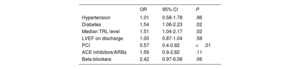
We collected data on 2234 patients, 1903 of whom were included in the final analyses. Reasons for exclusion were death during hospitalization and missing data. Mean±SD age of the patients (73% male) was 64±12 years. Patient characteristics are summarized in table 1 according to the occurrence or nonoccurrence of a new coronary event. Patients with recurrence had a lower left ventricular ejection fraction on discharge and were more likely to undergo percutaneous revascularization, receive neurohormonal blockade drug therapy, and have hypertension and diabetes. These patients also had a TRL level above the median for the sample, which was 27 [interquartile range, 21-35] mg/dL. The differences with controls without an ACS recurrence were significant in all cases. Median non–HDL-C for the sample was 118 [94–150] mg/dL, with no significant differences between the groups (table 1). In the multivariable analysis, admission TRL >27mg/dL was predictive of ACS recurrence within 12 months of the index event (odds ratio=1.51; 95% CI, 1.04-2.17; P=.02) (table 2).
Baseline characteristics of patients admitted for acute coronary syndrome according to whether or not they experienced recurrence in the first 12 months of follow-up
| Total (N=1903) | No recurrence (n=1757) | Recurrence (n=146) | P | |
|---|---|---|---|---|
| Age, y | 63±12 | 63±12 | 65±12 | .17 |
| Men | 1400 (73.6) | 1288 (73.3) | 112 (76.7) | .37 |
| Hypertension | 1216 (63.9) | 1109 (63.1) | 107 (73.3) | .014 |
| Diabetes | 698 (36.7) | 620 (35.3) | 78 (53.4) | <.001 |
| TRL | 988 (51.9) | 896 (51) | 92 (63) | .005 |
| TRLa | 27 [21-35] | 24.5 [19-32] | 30 [22-41] | .005 |
| Non-HDL cholesterol | 961 (50.5) | 889 (50.6) | 72 (49.3) | .76 |
| Non-HDL cholesterola | 118 [94-150] | 120.5 [88-139] | 117 [95-146] | .9 |
| Smoker | 1166 (61.3) | 1067 (60.7) | 81 (55.5) | .21 |
| Atrial fibrillation | 113 (6.4) | 107 (6.1) | 4 (3.4) | .1 |
| COPD | 95 (5) | 90 (5.1) | 5 (3.4) | .36 |
| CKDc | 191 (10) | 174 (10) | 17 (11.6) | .5 |
| LVEF on admissionb | 59.1±11 | 58.5±11.5 | 57.3±11.9 | .04 |
| Coronary revascularization | ||||
| Coronary revascularization surgery | 129 (6.8) | 123 (7) | 6 (4.1) | .18 |
| PCI | 1339 (70.4) | 1257 (71.5) | 82 (56.2) | <.001 |
| Treatment on discharge | ||||
| Statins | 1853 (97.4) | 1709 (97.3) | 144 (98.6) | .46 |
| Statins and ezetimibe | 373 (19.6) | 343 (19.5) | 30 (20.5) | .79 |
| ACE inhibitors/ARBs | 921 (48.4) | 838 (47.7) | 83 (56.8) | .03 |
| Beta-blockers | 425 (22.3) | 382 (21.7) | 43 (29.5) | .03 |
| Oral anticoagulants | 59 (3.1) | 58 (3.3) | 1 (0.7) | .13 |
| Antiplatelet agents | 1850 (97.2) | 1710 (97.3) | 140 (96) | .31 |
ACE, angiotensin-converting enzyme; ARBs, angiotensin II receptor blockers; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; HDL, high-density lipoprotein; PCI, percutaneous coronary intervention; TRL, triglyceride-rich lipoprotein.
Values are expressed as No. (%) for dichotomous variables, median [interquartile range] for nonnormally distributed continuous variables,a and mean±standard deviation for normally distributed variables.b
Results of logistic regression analysis according to recurrence of acute coronary syndrome in the first 12 months of follow-up
| OR | 95% CI | P | |
|---|---|---|---|
| Hypertension | 1.01 | 0.58-1.78 | .96 |
| Diabetes | 1.54 | 1.06-2.23 | .02 |
| Median TRL level | 1.51 | 1.04-2.17 | .02 |
| LVEF on discharge | 1.00 | 0.87-1.04 | .58 |
| PCI | 0.57 | 0.4-0.82 | <.01 |
| ACE inhibitors/ARBs | 1.59 | 0.9-2.82 | .11 |
| Beta-blockers | 2.42 | 0.97-6.08 | .06 |
ACE, angiotensin-converting enzyme; ARBs, angiotensin II receptor blockers; LVEF, left ventricular ejection fraction; OR, odds ratio; PCI, percutaneous coronary intervention.
This is the first study to show that high TRL levels increase the risk of ACS in the 12 months following an index event. The recommended target for LDL-C in patients with previous coronary heart disease (CHD) is <55mg/dL, and a goal of <85mg/dL in plasma has even been recommended for non-HDL-C.1 No targets, however, have been recommended for TRL.
This study shows that high TRL levels on admission for ACS may predict a new coronary event, an association not observed for non–HDL-C. Patients with high TRL levels have an increased cardiovascular risk. Among patients with previous CHD, the risk can be reduced by TRL lowering with statins.3 Duran et al.4 showed that ACS and peripheral arterial disease risk increased with TRL levels. These lipoproteins may even be an independent predictor of cardiovascular events in patients with previous CHD and LDL-C <70mg/dL.5
Secondary prevention strategies have focused more on LDL-C than on TRLs because the latter have a longer half-life and are less abundant in plasma.2 Apolipoproteins E and C III transported by TRLs are essential for endocytosis. In the case of LDL-C particles, prior oxidation is necessary for foam cell formation, but TRLs are more potent inducers of this process as they are directly phagocytized by macrophages.2,4 Cardiovascular risk in this setting may thus be linked to more efficient cholesterol deposition by TRLs and greater atherogenicity.
The main limitations of this study are those inherent to any retrospective, observational study. Our data suggest that secondary prevention measures in patients with previous CHD should also target TRLs. While they do not allow for definitive conclusions, they do suggest a scenario with potential clinical implications in which TRL levels could be used to predict new coronary events during follow-up.
FundingThe authors declare that they received no funding for this study.
Authors’ ContributionsN. Báez-Ferrer: study design, coordination of working group, and drafting of manuscript. M.A. Rivero-García and J.J. Castro-Martín: collection of clinical data. A. Domínguez-Rodríguez and P. Avanzas: critical review of intellectual content. N. Báez-Ferrer and P. Abreu-González: revision of manuscript and final approval.
Conflicts of InterestP. Avanzas is associate editor of Revista Española de Cardiología. The journal's editorial process was followed to guarantee impartiality. The other authors declare that they have no conflicts of interest.