The treatment strategy in acute myocardial infarction (AMI) has changed substantially in recent decades. After the enormous impact of fibrinolysis in the 1980s, the situation was further improved in the 1990s by the high level of efficacy and the safety of primary angioplasty, which significantly reduced the rate of in-hospital mortality. However, despite the available evidence,1 the performance of this intervention has not become widespread, and it is associated with a very marked clinical variability. Along the lines of the recommendations of the European and Spanish societies of cardiology, online programs have been set up in Spain to increase the use of and improve access to primary angioplasty for AMI patients, first in a single-province autonomous community (Murcia) in 2001, and later in an autonomous community consisting of 4 provinces2 (Galicia) in mid-2005. This project was the PROgrama GALlego de Atención al Infarto Agudo del Miocardio (PROGALIAM [Galician Program for Acute Myocardial Infarction Care]).
The purpose of PROGALIAM is to promote and facilitate access to primary angioplasty, establishing a single protocol for AMI care at the different health care levels. These efforts are consolidated under an online organizational model, with its node for the southern region of Galicia in the Complejo Hospitalario Universitario de Vigo (CHUVI). The process is coordinated by the center of operations of the 061 emergency transport and medical care service (the 061 service), which organizes the care and transport of patients from the out-of-hospital and in-hospital setting to the CHUVI and, depending on their clinical stability, returns them to the center from which they were referred.
The implementation of PROGALIAM was especially complex because Galicia is a multiprovince community with a widely scattered population of 2 737 370 and poor geographic access. However, in the analysis of isochrones for road transport provided by the 061 service, we observed that 97% of the population could be covered in less than 120min.
The Cardiac Catheterization and Interventional Cardiology Unit of the CHUVI is the referral center for primary angioplasty in southern Galicia. It offers 24-h care and has 7 secondary centers, in which primary angioplasty is not available, at distances ranging between 10km and 125km. The protocol was set in motion upon diagnosis of AMI in the prehospital setting (by the 061 service or by primary care physicians) or in one of the hospitals (mainly in the emergency services) on the basis of clinical suspicion and electrocardiographic confirmation.
Using the data collected for this program, we studied 2353 patients with AMI referred to the Cardiac Catheterization and Interventional Cardiology Unit of the CHUVI for primary angioplasty between 2005 and 2010. Out-of-hospital emergency services were most frequently the first contact of the patients with the health care system (46.4%), followed by hospital emergency services (32.5%), whereas 17% were brought directly to the CCICU by the 061 service. Of the patients whose first contact was a hospital emergency service, 16.5% came initially to the Emergency Service of the CHUVI and 83.5% were transferred from a secondary hospital (23.3% less than 10km away, 40.7% between 10km and 50km away, and 19.5% more than 50km away).
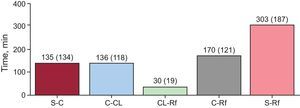
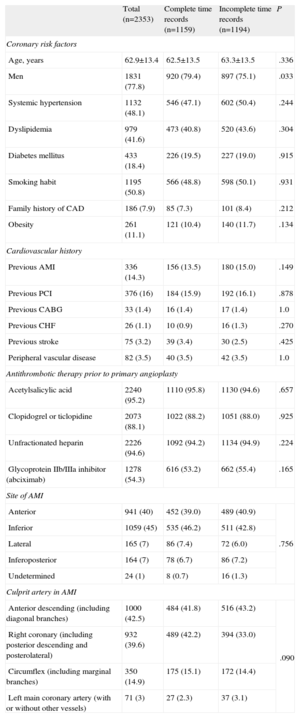
The Table presents the characteristics of the treated population. In all, 72% of the patients underwent implantation of a single stent, which was conventional in 68%, and angiographic success was achieved in over 92% of the cases. The Figure shows the total ischemia-reperfusion times in the 1159 patients for whom a complete record of the response and medical care times was available.
Baseline Characteristics of the Study Population
| Total (n=2353) | Complete time records (n=1159) | Incomplete time records (n=1194) | P | |
| Coronary risk factors | ||||
| Age, years | 62.9±13.4 | 62.5±13.5 | 63.3±13.5 | .336 |
| Men | 1831 (77.8) | 920 (79.4) | 897 (75.1) | .033 |
| Systemic hypertension | 1132 (48.1) | 546 (47.1) | 602 (50.4) | .244 |
| Dyslipidemia | 979 (41.6) | 473 (40.8) | 520 (43.6) | .304 |
| Diabetes mellitus | 433 (18.4) | 226 (19.5) | 227 (19.0) | .915 |
| Smoking habit | 1195 (50.8) | 566 (48.8) | 598 (50.1) | .931 |
| Family history of CAD | 186 (7.9) | 85 (7.3) | 101 (8.4) | .212 |
| Obesity | 261 (11.1) | 121 (10.4) | 140 (11.7) | .134 |
| Cardiovascular history | ||||
| Previous AMI | 336 (14.3) | 156 (13.5) | 180 (15.0) | .149 |
| Previous PCI | 376 (16) | 184 (15.9) | 192 (16.1) | .878 |
| Previous CABG | 33 (1.4) | 16 (1.4) | 17 (1.4) | 1.0 |
| Previous CHF | 26 (1.1) | 10 (0.9) | 16 (1.3) | .270 |
| Previous stroke | 75 (3.2) | 39 (3.4) | 30 (2.5) | .425 |
| Peripheral vascular disease | 82 (3.5) | 40 (3.5) | 42 (3.5) | 1.0 |
| Antithrombotic therapy prior to primary angioplasty | ||||
| Acetylsalicylic acid | 2240 (95.2) | 1110 (95.8) | 1130 (94.6) | .657 |
| Clopidogrel or ticlopidine | 2073 (88.1) | 1022 (88.2) | 1051 (88.0) | .925 |
| Unfractionated heparin | 2226 (94.6) | 1092 (94.2) | 1134 (94.9) | .224 |
| Glycoprotein IIb/IIIa inhibitor (abciximab) | 1278 (54.3) | 616 (53.2) | 662 (55.4) | .165 |
| Site of AMI | ||||
| Anterior | 941 (40) | 452 (39.0) | 489 (40.9) | .756 |
| Inferior | 1059 (45) | 535 (46.2) | 511 (42.8) | |
| Lateral | 165 (7) | 86 (7.4) | 72 (6.0) | |
| Inferoposterior | 164 (7) | 78 (6.7) | 86 (7.2) | |
| Undetermined | 24 (1) | 8 (0.7) | 16 (1.3) | |
| Culprit artery in AMI | ||||
| Anterior descending (including diagonal branches) | 1000 (42.5) | 484 (41.8) | 516 (43.2) | .090 |
| Right coronary (including posterior descending and posterolateral) | 932 (39.6) | 489 (42.2) | 394 (33.0) | |
| Circumflex (including marginal branches) | 350 (14.9) | 175 (15.1) | 172 (14.4) | |
| Left main coronary artery (with or without other vessels) | 71 (3) | 27 (2.3) | 37 (3.1) | |
AMI, acute myocardial infarction; CABG, coronary artery bypass graft surgery; CAD, coronary artery disease; CHF, congestive heart failure; PCI, percutaneous coronary intervention.
Data are expressed as mean±standard deviation or No. (%).
Total ischemia-reperfusion times (mean [standard deviation]). C-CL, from first medical contact to arrival of the patient in the catheterization laboratory; C-Rf, from first medical contact to coronary reperfusion; CL-Rf, from arrival of the patient in the catheterization laboratory to coronary reperfusion; S-C, from the onset of symptoms to first medical contact; S-Rf, from the onset of symptoms to coronary reperfusion.
The time from first medical contact to reperfusion in patients with direct access provided by the 061 service was reduced by 34% (47min)—median, 83min [interquartile range, 47-115min]—with respect to access through hospital emergency services—median, 130min [105-217min] (P<.001)—and by 37% (50min) when compared with access through out-of-hospital emergency services—median, 133min [90-184min] (P<.001).
Of the patients with access through hospital emergency services, those with initial access to the emergency service of the CHUVI had a median time from first medical contact to reperfusion of 144min [79-189min] and those transferred to the CHUVI from a secondary center, of 142min [101-211min] (P=.682).
The overall in-hospital mortality rate was 5.8% (4.9% for distances of less than 10km from the CHUVI, 4.8% for distances of 10km to 50km, and 6.2% for those greater than 50km; P=.670), and the mortality after 1 year of follow-up was 7.9%. We observed a direct linear association between lower mortality rate and shorter time to reperfusion: 4.7% (51 patients) when less than 120min; 6.8% (74 patients) when 120 to 180min; 7.0% (76 patients) when 181 to 360min, and 10.0% (109 patients) when greater than 360min (P<.001). Similar findings were recorded in the PROGALIAM program in northern Galicia,3 with a 30-day mortality of 0.9% among patients with symptom onset to balloon times of less than 2h and 6.7% when this interval was over 2h. In our study, the incidences of adverse events during the hospital stay and after 1 year of follow-up were less than 4% for reinfarction and less than 1% for stroke and major bleeding, similar to those reported for the Infarction Code Program in the southern metropolitan area of Barcelona, Spain.4
PROGALIAM for the Area of Southern Galicia demonstrates that, with a structured health network model, the rapid transfer of AMI patients from the different care levels to a primary angioplasty center is feasible and safe, even in areas of difficult access and a widely scattered population, and that high rates of reperfusion and low mortality rates are obtained.
In our population, we detected a considerable delay from the onset of symptoms to the first medical contact, a circumstance that has a negative impact on the times to reperfusion. However, the activation of the system from the 061 service shortens the delay from first medical contact to reperfusion by one third compared to other available modes of access to primary angioplasty and thus it is essential to promote its use. Likewise, the optimization of strategies for early diagnosis and transfer from in-hospital and out-of-hospital settings by standardizing a single management protocol is vital for maintaining the benefit of primary angioplasty and achieving greater compliance with the times recommended by the guidelines. It is necessary to implement educational programs focusing on cardiovascular health for the general population, and to inform health care professionals and intermediate entities of the protocols, in order to reduce ischemia-reperfusion times and thus improve the prognosis of these patients.
.

![Total ischemia-reperfusion times (mean [standard deviation]). C-CL, from first medical contact to arrival of the patient in the catheterization laboratory; C-Rf, from first medical contact to coronary reperfusion; CL-Rf, from arrival of the patient in the catheterization laboratory to coronary reperfusion; S-C, from the onset of symptoms to first medical contact; S-Rf, from the onset of symptoms to coronary reperfusion. Total ischemia-reperfusion times (mean [standard deviation]). C-CL, from first medical contact to arrival of the patient in the catheterization laboratory; C-Rf, from first medical contact to coronary reperfusion; CL-Rf, from arrival of the patient in the catheterization laboratory to coronary reperfusion; S-C, from the onset of symptoms to first medical contact; S-Rf, from the onset of symptoms to coronary reperfusion.](https://static.elsevier.es/multimedia/18855857/0000006600000006/v1_201307091102/S1885585713000443/v1_201307091102/en/main.assets/thumbnail/gr1.jpeg?xkr=eyJpdiI6ImFjTkd4QmF6WHYrU0NQM0hOOHVXSEE9PSIsInZhbHVlIjoiR0pRMForMnFKdkNhWjNLNG5SMlR4T2lEZ3RWZHY3czVyM1NUVUtaRGZsND0iLCJtYWMiOiIxNjVkODUzZjJhZjQ5YTM4NDhiYTQyMmRhZDBiYTIzYjc5ZjE0OTRjNzM5NDY1YjA1YTlkOTkzY2ZjODJjY2RkIiwidGFnIjoiIn0=)