Contrast-induced acute kidney injury (CI-AKI) is an important cause of hospital-acquired acute renal failure and has a poor prognosis. Serum creatinine (sCr) exhibits shortcomings because its elevation is relatively slow and is influenced by extrarenal factors.1 Recently, neutrophil gelatinase-associated lipocalin (NGAL) has emerged as an early, sensitive, noninvasive biomarker for predicting CI-AKI in different cardiovascular conditions.2,3 However, the role of early measurements of NGAL for predicting sCr changes in unselected patients with acute coronary syndrome (ACS) and receiving iodixanol, an iso-osmolar nonionic contrast agent, has not been defined. The aim of this study was to evaluate the usefulness of early determinations of NGAL for predicting sCr changes within 48 hours after coronary-angiography (ΔCr-48 h) in ACS patients receiving iodixanol.
We included 105 consecutive patients with ACS undergoing coronary-angiography and receiving iodixanol (Visipaque). Serum creatinine was measured before and 24 and 48 hours after angiography. Serum NGAL was measured before and 4, 8, and 24 hours postprocedure. Per protocol, iodixanol was used in all patients. Additional measures for preventing CI-AKI were individualized according to the attending physician. CI-AKI was defined as an increase in sCr of > 25% or > 0.5 mg/dL from baseline within 48 hours postprocedure. NGAL was measured with a fluorescence-immunoassay. Estimated glomerular filtration rate (eGFR) was estimated by applying the 4-variable Modification of Diet in Renal Disease (MDRD) formula. The primary endpoint was to determine the association between NGAL measurements within 24-hours and the maximum absolute ΔCr-48 h. The secondary endpoints were to evaluate: a) whether NGAL measurements were associated with the risk of CI-AKI and, b) the association between volume of contrast and ΔCr-48 h. Continuous variables were expressed as mean ± standard deviation (SD) or median [interquartile range (IQR)] when appropriate, and discrete variables as percentages. Linear regression analysis was used to determine the association between NGAL and ΔCr-48 h measurements. The risk of CI-AKI was assessed using a logistic regression model. A 2-sided P-value of < .05 was considered to be statistically significant.
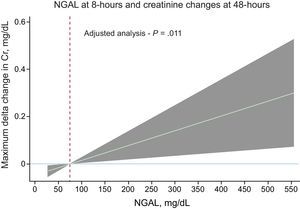
The baseline characteristics of the sample are summarized in the Table. NGAL values (median [IQR]) increased at each time point: 63 (49, 112), 69 (56, 116), 75 (50, 114), and 77 (64, 174) ng/mL, for baseline and 4, 8, and 24-hours, respectively. The mean sCr on admission and ΔCr-48 h (mg/dL) were 0.98 ± 0.35 and 0.06 ± 0.24, respectively. Six patients (5.7%) developed CI-AKI at 48 hours. There was a positive linear association between NGAL and ΔCr-48 h in the whole sample irrespective of time point (P < .05 for all comparisons) as shown in the . On multivariate analysis, including age, diabetes mellitus, eGFR < 60 min/mL/1.73m2, type of ACS, and Killip > I on admission, NGAL-8 h remained positive, significant and linearly associated with ΔCr-48 h [β coefficient, per 100 ng/mL: 0.63; 95% confidence interval (95%CI), 0.15-1.11; P = .011]. The gradient of risk of NGAL-8 h for predicting ΔCr-48 h is shown in the Figure. This model accounted for 33% of the variability in ΔCr-48 h. Ranked in order of importance (drop in R2), NGAL-8 h (40%), eGFR < 60 min/mL/1.73 m2 (21.5%) and diabetes mellitus (17.3%) were the most important covariates predicting ΔCr-48 h. Likewise, NGAL-24 h was independently related to ΔCr-48 h (β coefficient, per 100 ng/mL: 0.62; 95%CI, 0.08-1.17; P = .026), whereas baseline-NGAL and NGAL-4 h remained borderline associated with ΔCr-48 h (). In a univariate analysis, baseline-NGAL, NGAL-4 h, NGAL-8 h and NGAL-24 h, per increase in 10 ng/mL were borderline associated to CI-AKI. The receiving operating curve of NGAL-8 h showed a high discriminative ability for predicting CI-AKI (area under the curve of 0.788). A value ≥ 92 ng/mL showed a sensitivity of 100% and a specificity of 60.6%. The volume of contrast administration (149.2 ± 66.4 mL) was not associated with ΔCr-48 h in the univariate (β coefficient, per 100 mL: 0.02; 95%CI, −0.09-0.07; P = .698) or multivariate analysis (β coefficient, per 100 mL: 0.03; 95%CI, −0.05-0.10; P = .451).
Baseline Characteristics
| Total sample (n = 105) | |
|---|---|
| Age, y | 65 ± 11 |
| Male, n (%) | 69 (66) |
| Weight, kg | 78.7 ± 22.5 |
| Height, cm | 160.9 ± 17 |
| Hypertension, n (%) | 78 (74) |
| Diabetes mellitus, n (%) | 24 (23) |
| Insulin-dependent diabetes mellitus, n (%) | 6 (6) |
| Dyslipidemia, n (%) | 63 (60) |
| Current smoker, n (%) | 60 (57) |
| Previous smoker, n (%) | 12 (11) |
| Prior history of MI, n (%) | 24 (23) |
| Prior chronic kidney disease, n (%) | 6 (5.7) |
| Killip class >I on admission, n (%) | 24 (23) |
| Systolic blood pressure, mmHg | 135 ± 31 |
| Diastolic blood pressure, mmHg | 74 ± 14 |
| Prior history of PCI, n (%) | 21 (20) |
| Indication for PCI at index admission, n (%) | |
| STEMI | 66 (63) |
| NSTEMI | 39 (37) |
| Number of coronary vessels affected, n (%) | |
| 0 | 6 (6) |
| 1 | 60 (57) |
| 2 | 24 (23) |
| 3 | 18 (17) |
| PCI, n (%) | 87 (83) |
| Serum creatinine at admission, mg/dL | 0.98 ± 0.34 |
| eGFRaat admission, mL/min/1.73 m2 | 83.6 ± 28.5 |
| eGFRaat admission < 60 mL/min/1.73 m2, n (%) | 21 (20) |
| Serum NGALbat admission, ng/mL | 63 (49, 112) |
eGFR, estimated glomerular filtration rate; MI, myocardial infarction; NGAL, neutrophil gelatinase-associated lipocalin; NSTEMI, non–ST-elevation acute myocardial infarction: PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
Data are expressed as no. (%), mean ± standard deviation or median [interquertile range].
This study shows that NGAL measurements before and early after angiogram predict absolute changes in sCr in ACS patients receiving iodixanol as contrast-agent. Nevertheless, NGAL-8 h postprocedure showed the best diagnostic performance. NGAL has shown, in the absence of diagnostic increases in sCr, to detect patients with subclinical CI-AKI who have an increased risk of adverse outcomes.2 Prior studies demonstrate the usefulness of NGAL as an early biomarker of CI-AKI in different scenarios, especially after contrast administration.3 However, the optimal timing for its determination following coronary angiography has not yet been well elucidated. Herein, a formal comparison among different time points revealed that all of them were predictive of ΔCr-48 h. Nevertheless, the best performance of NGAL-8 h may help clinicians to identify those patients at higher risk of developing CI-AKI who could benefit from preventive strategies.4 In this regard, and in agreement with recent findings,5 we note that the volume of iodixanol was not related to CI-AKI.
Some limitations need to be addressed. This is a small single-center study. The low incidence of CI-AKI precludes obtaining robust estimates of risk regarding this endpoint. A confounding variable such as volume of fluid administration before angiography was not routinely registered, precluding analysis of its influence. Lastly, we did not evaluate CI-AKI beyond 48 hours.
In conclusion, NGAL measurements 8 hours postprocedure predict creatinine changes in ACS patients undergoing coronary-angiography and receiving iodixanol as contrast agent.
FundingThis study was supported by an unrestricted grant from GE Healthcare-Medical Diagnostics and Red de Investigación Cardiovascular; Programa 7 (RD12/0042/0010) FEDER.