Transesophageal echocardiography (TEE) causes nausea, pain, and anxiety and must be performed under sedation and analgesia. The American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists recommend a number of drugs for this purpose (topical anesthesia, benzodiazepines, opioids, and, with a narrower safety profile, propofol), but they do not specify doses, combinations, or order of administration.1 Midazolam is recommended as the drug of choice by the European Association of Cardiovascular Imaging, which proposes fentanyl as an alternative but does not mention propofol.2 Spanish law does not dictate which physicians are allowed to use propofol. This drug is widely used to induce anesthesia during procedures requiring deep sedation, but its use has spread to TEE, where it is sometimes administered by cardiologists. A study comparing anesthesiologist-administered propofol, midazolam, and midazolam-alfentanil during TEE found that propofol produced deeper, more rapid sedation without major complications.3 Another study comparing propofol administered by anesthesiologists and nonanesthesiologists during TEE found that mild respiratory complications were more common in the first group because the patients had a higher risk profile.4 Propofol has also been shown to be an effective sedation agent in a clinical trial setting.5
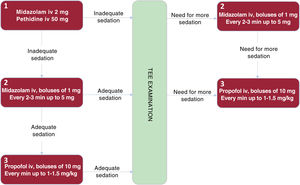
We describe our experience with a sedation and analgesia protocol that includes propofol as a second option when adequate sedation is not achieved with midazolam and pethidine. The anesthesia department at our hospital is familiar with and has endorsed the use of this protocol.
We prospectively included all patients who underwent TEE from May 2020 to April 2021. The study was approved by the local ethics committee. A 10-item safety checklist was administered before each procedure, and propofol was not allowed in patients allergic to peanuts, soy, or eggs. Four expert echocardiographers performed the procedures in a room with cardiopulmonary resuscitation equipment. All patients received oxygen via a nasal cannula (3 L/min) and were administered topical lidocaine at the discretion of the echocardiographer. The protocol is shown in figure 1. Frail patients and patients with a high American Society of Anesthesiologists score were administered half a dose of pethidine (25mg) or none. Following TEE examination, patients were transferred to the recovery room and their intravenous access maintained until they regained consciousness and their vital signs were stable.
Blood pressure, heart rate, oxygen saturation, and sedation level (Ramsay scale) were recorded at baseline and every 3minutes. Sedation time was defined as the time from sedation initiation to probe withdrawal and recovery time as the time from probe withdrawal to discharge from the recovery room. Before leaving the hospital, patients completed a questionnaire in which they were asked to rate the following: a) their perceived level of sedation on a 10-point visual analog scale (VAS), where 10 represented ideal sedation, and b) level of discomfort or pain, where a VAS score of 10 represented the worst possible pain. They were also asked if they would choose the same sedation if they had to repeat the examination and if they would recommend it to another patient. Cardiologists, also scoring from 0 to 10, rated their satisfaction with the sedation regimen in terms of the TEE procedure and ease of image acquisition. They were also asked if they would recommend the regimen and use it again in future TEE examinations.
In total, 286 TEE procedures were performed in 286 patients. Fifty-six patients (19.6%) were administered topical lidocaine. They all received midazolam at a median dose of 3mg [interquartile range, 2.75-4mg]. Pethidine was administered at a dose of 50mg to 259 patients (90.6%) and 25mg to 23 (8%). Four patients (1.4%) did not receive this drug. Propofol at a median dose of 20mg [10-30mg] was administered to 54 patients (18.9%). It was prepared in a 10-mL syringe (10mg propofol/mL) and administered in boluses of 1mL. The reason for its use in all cases was insufficient sedation. There were no paradoxical reactions to midazolam. Eleven of the 54 patients (20.37%) were administered propofol before intubation. Flumazenil was used in 22 of the 286 procedures (7.7%). Naloxone was not used. None of the patients required ventilation with a manual resuscitator or intervention by the anesthesiologist. Baseline clinical characteristics, sedation and recovery times, complications, and patient and cardiologist satisfaction scores are shown in table 1 for the procedures as a whole and according to whether propofol was used or not.
Baseline patient characteristics, procedure times, sedation- and procedure-related complications, and patient and cardiologist satisfaction
| All procedures (n=286) | Procedures without propofol (n=232) | Procedures with propofol (n=54) | P | |
|---|---|---|---|---|
| Age, ya | 66 [53.75-75] | 68 [55.25-76] | 57.50 [42.75-64.25) | <.001b |
| Male sexc | 175 (61.2) | 133 (57.3) | 42 (77.8) | .005b |
| Body surface areaa | 1.90 (0.2) | 1.89 (0.2) | 1.95 (0.19) | .056 |
| Body mass indexa | 27.55 [24.5-31.15] | 27.74 [24.35-30.98] | 26.83 [24.69-31.83] | .98 |
| Patientc | ||||
| Outpatient | 171 (59.8) | 129 (55.6) | 42 (77.8) | .003b |
| Hospitalized | 115 (40.2) | 103(44.4) | 12 (22.2) | |
| Atrial fibrillation/flutterc | 83 (29) | 71 (30.6) | 12 (22.2) | .222 |
| Diabetes mellitusc | 71 (24.8) | 70 (30.2) | 1 (1.9) | <.001b |
| Hypertensionc | 180 (62.9) | 150 (64.7) | 30 (55.6) | .212 |
| Dyslipidemiac | 124 (43.4) | 106 (45.7) | 18 (33.3) | .099 |
| COPDc | 19 (6.6) | 16 (6.9) | 3 (5.6) | .716 |
| Obesityc | 87 (30.4) | 72 (31.0) | 15 (27.8) | .639 |
| Liver diseasec | 7 (2.4) | 5 (2.1) | 2 (3.7) | .529 |
| Alcoholc | 26 (9.1) | 16 (6.9) | 10 (18.5) | .014b |
| Creatininea | 0.95 [0.79-1.15] | 0.96 [0.8-1.19] | 0.90 [0.74-1.05] | .092 |
| LVEF >50%c | 222 (77.6) | 176 (75.9) | 46 (85.2) | .139 |
| ASA scorec | ||||
| ≤2 | 48 (16.8) | 31 (13.3) | 17 (31.5) | .001b |
| >2 | 238 (83.2) | 201 (86.7) | 37 (68.5) | |
| Times | ||||
| Sedation timea | 20.38 [16.26-25.24] | 20.34 [16.17-24.52] | 20.53 [16.77-27.16] | .235 |
| Recovery timea | 31.66 (16-46) | 29.87 (14.81-45.81) | 33.30 (21.00-46.41) | .104 |
| Drugs | ||||
| Lidocaine | 56 (19.6) | 49 (21.1) | 7 (13) | .174 |
| Flumazenil | 22 (7.7) | 18 (7.8) | 4 (7.4) | 1.000 |
| Sedation-related complications | ||||
| Mild hypoxemia (SatO2, 81%-89%)c | 15 (5.2) | 12 (5.2) | 3 (5.6) | 1.000 |
| Mild hypotension (SBP <90mmHg for >3minc | 39 (13.6) | 29 (12.5) | 10 (18.5) | .246 |
| Bradycardiac | 2 (0.7) | 2 (0.9) | 0 (0.0) | 1.000 |
| Procedure-related complications | ||||
| Coughc | 30 (10.5) | 20 (8.6) | 10 (18.5) | .033b |
| Nauseac | 30 (10.5) | 15 (6.5) | 15 (27.8) | <.001b |
| Moderate bleedingc | 3 (1) | 2 (0.9) | 1 (1.9) | .468 |
| Esophageal tearc | 1 (0.3) | 1 (0.3) | 0 (0) | - |
| Patient satisfaction | ||||
| Level of sedationc | ||||
| <8 | 16 (5.7) | 15 (6.5) | 1 (1.9) | .129 |
| ≥8 | 266 (94.3) | 213 (91.8) | 53 (98.1) | |
| Would recommendc | 278 (97.2) | 224 (96.6) | 54 (100) | .19 |
| Would choose againc | 278 (97.2) | 224 (96.6) | 54 (100) | .19 |
| Painb | 35 (12.2) | 28 (12.1) | 7 (12.9) | .891 |
| Cardiologist satisfaction | ||||
| TEE procedurec | ||||
| <8 | 35 (12.2) | 23 (9.9) | 12 (22.2) | .013b |
| ≥ 8 | 251 (87.8) | 209 (90.1) | 42 (77.8) | |
| Image capturec | ||||
| <8 | 37 (12.9) | 21 (9.1) | 16 (29.7) | <.001b |
| ≥8 | 249 (87.1) | 211 (90.9) | 38 (70.3) | |
| Would recommendc | 282 (98.6) | 229 (98.7) | 53 (98.1) | .761 |
| Would acceptc | 281 (98.3) | 229 (98.7) | 52 (96.3) | .269 |
Abbreviations: ASA, American Society of Anesthesiologists; COPD, chronic obstructive pulmonary disease; LVEF, left ventricular ejection fraction; SatO2, oxygen saturation; TEE, transesophageal echocardiography.
Patients administered propofol were significantly younger and more likely to be male, to have been admitted on an outpatient basis, to consume alcohol, and to have an ASA score of 2 or lower. There were no differences in complications between the propofol and nonpropofol groups, although patients in the former had a higher frequency of cough and nausea. Cardiologist satisfaction with the TEE examination and image acquisition was lower in the propofol group, probably because of the greater difficulty in attaining adequate sedation, as reflected by the higher rates of cough and nausea. There were no differences between the groups in terms of patient satisfaction with level of sedation and comfort.
Our findings show that adding propofol to achieve adequate sedation in imaging units when midazolam and pethidine are insufficient is safe and does not affect patient satisfaction. Our findings are limited because we analyzed a small number of cases in a nontrial setting. Multicenter trials with larger samples would be helpful for comparing different sedation regimens.
FundingNone
Authors’ ContributionsI. Paneque and J. López-Haldón: design, analysis, and writing of manuscript. N. Galán-Páez, M.R. Camacho-Fernández de Líger, C. Lao-Peña, and A. Aguilera-Saborido: data collection and manuscript review.
Conflicts of InterestNone.