The SAMe-TT2R2 score has been proposed as a way to predict the acceptability of anticoagulation control in patients with nonvalvular atrial fibrillation.1 This score has been shown to be useful in different cohorts,2 but there have been no assessments of its usefulness in patients with recently decompensated heart failure (HF).
Given that atrial fibrillation and HF often occur concurrently and that HF is associated with poor anticoagulation control,1 we believe that validation of the SAMe-TT2R2 score in patients with HF could be a useful exercise for clinical practice. Thus, with the aim of extending the validity of this scale, we assessed its predictive and discriminative capacity in a cohort of patients with nonvalvular atrial fibrillation receiving anticoagulation therapy with vitamin K antagonists and with recently decompensated HF.
The study was conducted according to the tenets of the Declaration of Helsinki. The retrospective analysis used data collected for a prospective registry in the cardiology department of a tertiary hospital between January 2008 and September 2011. The study included all patients with nonvalvular atrial fibrillation who received anticoagulant therapy with vitamin K antagonists after discharge following an episode of acute decompensated heart failure. Patients with a contraindication for the new anticoagulants and those with fewer than 2 international normalized ratio (INR) measurements in the 6 months after hospital discharge were excluded (n=19). The SAMe-TT2R2 score was calculated at the time of inclusion for all patients. The time in therapeutic range (TTR) was estimated according to the Roosendaal method and poor anticoagulation control was defined as TTR<65%. A binary logistic regression analysis was conducted to assess the association between SAMe-TT2R2 score and INR control. Discriminatory capacity was analyzed by calculating the area under the receiver operating characteristic (ROC) curve. The model was calibrated using the Hosmer-Lemeshow goodness of fit test.
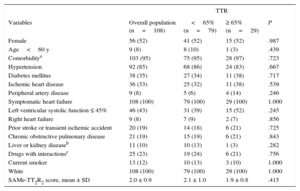
In total, 108 patients were included. The median number of INR measurements was 8 (interquartile range [IQR], 6.25-10; range, 3-16). The median SAMe-TT2R2 score was 2 (IQR, 1-2). Overall, 70% (n=76) of the patients had an SAMe-TT2R2 score ≥ 2. The mean estimated TTR during follow-up was 48% ± 24% and 73% (n=79) had a TTR<65%. As shown in the Table, of the components of the score, no factor was significantly associated with poor INR control in this population.
Distribution of Different Variables According to Anticoagulation Quality During Follow-up
| TTR | ||||
|---|---|---|---|---|
| Variables | Overall population (n=108) | <65% (n=79) | ≥ 65% (n=29) | P |
| Female | 56 (52) | 41 (52) | 15 (52) | .987 |
| Age<60 y | 9 (8) | 8 (10) | 1 (3) | .439 |
| Comorbiditya | 103 (95) | 75 (95) | 28 (97) | .723 |
| Hypertension | 92 (85) | 68 (86) | 24 (83) | .667 |
| Diabetes mellitus | 38 (35) | 27 (34) | 11 (38) | .717 |
| Ischemic heart disease | 36 (33) | 25 (32) | 11 (38) | .539 |
| Peripheral artery disease | 9 (8) | 5 (6) | 4 (14) | .246 |
| Symptomatic heart failure | 108 (100) | 79 (100) | 29 (100) | 1.000 |
| Left ventricular systolic function ≤ 45% | 46 (43) | 31 (39) | 15 (52) | .245 |
| Right heart failure | 9 (8) | 7 (9) | 2 (7) | .856 |
| Prior stroke or transient ischemic accident | 20 (19) | 14 (18) | 6 (21) | .725 |
| Chronic obstructive pulmonary disease | 21 (19) | 15 (19) | 6 (21) | .843 |
| Liver or kidney diseaseb | 11 (10) | 10 (13) | 1 (3) | .282 |
| Drugs with interactionsc | 25 (23) | 19 (24) | 6 (21) | .756 |
| Current smoker | 13 (12) | 10 (13) | 3 (10) | 1.000 |
| White | 108 (100) | 79 (100) | 29 (100) | 1.000 |
| SAMe-TT2R2 score, mean ± SD | 2.0 ± 0.9 | 2.1 ± 1.0 | 1.9 ± 0.8 | .415 |
TTR, time in therapeutic range.
Data are expreseed as no. (%) or mean ± standard deviation.
History of 2 or more of the following: hypertension, diabetes mellitus, ischemic heart disease, peripheral artery disease, heart failure, stroke or transient ischemic accident, pulmonary disease, and liver or kidney disease.
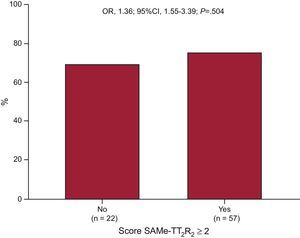
The SAMe-TT2R2 score was similar in patients with TTR ≥ 65% and in those with TTR<65% (1.9 ± 0.8vs 2.1 ± 1.0, respectively; P=.415). The percentage of patients with SAMe-TT2R2 score ≥ 2 did not differ between those with TTR ≥ 65% and those with TTR<65% (69% vs 75%, respectively; P=.504; Figure). The calibration of the score was good (Hosmer-Lemeshow test, P=.75). However, in the discrimination analysis, the area under the ROC curve was 0.54 with a 95% confidence interval of 0.42-0.66 and so it was not possible to establish a cutoff to predict INR control.
In our cohort of patients with nonvalvular atrial fibrillation and recently decompensated HF, INR control was poor and the SAMe-TT2R2 score was not useful for identifying patients with good or poor anticoagulation with vitamin K antagonists. These results contrast with those of a study in which prior HF was not significantly associated with worse INR control in patients with nonvalvular atrial fibrillation (TTR<65%: 47.4% in patients with HF vs 52.6% in other patients; P=.189).3 However, we believe that it is not history of HF that is responsible for poor anticoagulation control but rather the severity of HF. In our study, all patients had recently decompensated HF, placing them in a high risk group. In view of our results, we believe that these patients should be more closely monitored, or they could be treated with direct oral anticoagulants given the poor anticoagulation control with vitamin K antagonists in most cases. In fact, in large randomized phase III trials with currently available direct anticoagulants, patients with HF were well represented (between 32.0% and 62.5%) and, in the subgroup analysis, there was no statistically significant heterogeneity with respect to efficacy or safety in the treatment of these patients.4–6 Our results show the need for additional validation studies for the SAMe-TT2R2 score in these patients. One of the main limitations of the study is the small sample size and its retrospective design. The clinical profile of our patients (as in other series of acute HF), with SAMe-TT2R2 scores > 2 in 70%, can be explained by the low discriminatory capacity in this context. Finally, it would be clinically useful to develop new scoring systems that could identify patients who will have poorly controlled anticoagulation with vitamin K antagonists in this scenario.