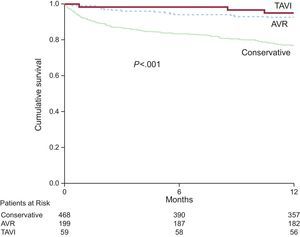
Severe aortic stenosis (AS) is a condition with poor prognosis that predominantly affects the elderly. There is little real-life information on its treatment and prognosis. Accordingly, the data from the IDEAS registry,1 coordinated by the Geriatric Cardiology Section of the Spanish Society of Cardiology, are particularly timely. This multicenter registry included 726 consecutive patients with severe AS and a mean age of 77 years, with a 1-year follow-up. The most frequent treatment was conservative (65%), followed by aortic valve replacement (27%) and transcatheter aortic valve implantation (TAVI) (8%), with 1-year survival rates of 76%, 95%, and 93%, respectively (Figure 1). These data confirm the need for intervention in patients with severe symptomatic AS and highlight the relatively infrequent use of such procedures. Notably, the intervention rates in this registry were significantly lower when the patients were managed in nontertiary centers. Further important results were provided by the recently published PARTNER 2 trial.2 In that study, 2032 patients with severe AS and intermediate surgical risk were randomized to TAVI (76.3% transfemoral access, 23.7% transthoracic access) or aortic valve surgery. The primary endpoint (death from any cause or disabling stroke at 2 years) was similar in the 2 groups (P = .001 for noninferiority). The primary endpoint occurred in 19.3% of the patients in the TAVI group and in 21.1% of the patients in the surgical group (TAVI group, hazard ratio [HR], 0.89; 95% confidence interval [95%CI], 0.73-1.09, P = .25). Notably, there was a significant reduction in the primary endpoint with the transfemoral approach vs surgery (HR, 0.79, 95%CI, 0.62-1.00; P = .05), but there was no significant difference with transthoracic access. Other benefits of TAVI were a greater aortic area and a lower frequency of acute kidney injury, life-threatening bleeding, and atrial fibrillation. Surgery was associated with a lower rate of vascular complications and residual aortic regurgitation. This study vindicates the widespread practice in many Spanish groups characterized by TAVI in elderly patients with AS and intermediate risk.
The importance of geriatric factors such as functional status, frailty, dependency, and comorbidity in elderly patients with heart failure (HF) is well known.3 Accordingly, the work of Vidán et al.4 is particularly interesting. This study highlights the importance of frailty detection in elderly patients hospitalized for HF because frailty⿿apart from being highly prevalent, even in independent ambulatory patients⿿is an independent predictor of disability and of future events such as readmission and mortality. According to recent data, the list of geriatric factors should also include malnutrition. A recent study by Honda et al.5 has shown that nutritional status is one of the strongest prognostic predictors in patients older than 65 years with acute HF. This work validates and stresses the considerable usefulness of an easily obtained parameter, the Geriatric Nutritional Risk Index, which has better prognostic value than other nutritional indices. In addition, it supports the incorporation of this parameter in risk evaluation and stratification in elderly patients with HF.
The prognostic value of natriuretic peptides is well known. A recent work, based on 7 European registries and conducted in patients older and younger than 75 years hospitalized for acute HF, studied the prognostic value and reasons for success or failure of a reduction in N-terminal pro⿿B-type natriuretic peptide (NT-proBNP) (in absolute values or as a percentage vs admission levels) to target values at discharge.6 Older patients were more likely to be women, with nonischemic HF and preserved ejection fraction, higher NT-proBNP concentrations at admission and discharge, and a lower glomerular filtration rate. The higher the absolute NT-proBNP values and the lower their relative decrease, the higher the 6-month mortality in both groups; this increase was significant in the older group. With similar NT-proBNP values, mortality was very similar, independently of age. Thus, NT-proBNP showed a prognostic value in acute HF that was independent of age, but certain factors more frequent in older patients (such as higher NT-proBNP values at admission, anemia, and nonischemic etiology) made it more difficult to achieve lower values and greater reductions in this marker at discharge, with a consequent increase in mortality.