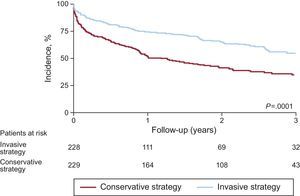
The last year has seen important advances in the treatment of acute coronary syndrome (ACS) in the elderly. In the After Eighty trial,1 457 patients aged 80 years or older with non⿿ST-segment elevation ACS (NSTEACS) were randomized to either an invasive or a conservative treatment strategy. The invasive strategy group showed a reduction in the primary outcome (acute myocardial infarction [AMI], urgent revascularization, stroke, and death during follow-up) (40.6% vs 61.4%; P<.0001) (Figure), with no differences in bleeding complications. Some aspects of the study merit discussion: a) only 457 (23.2%) of the 1973 patients who could be included were randomized to a group, calling into question the external validity of the results; b) no data were available on frailty and other aging-related variables, although the prevalence of comorbidities was relatively low; and c) the excessive patient restriction in the conservative strategy group fails to reflect the real-world situation.
The MOSCA trial2 included 106 patients aged 70 years or older with non-ST elevation AMI and considerable comorbidity (defined as at least 2 of the following: renal failure, dementia, peripheral vascular disease, chronic obstructive pulmonary disease, and anemia). Patients were randomized to an invasive strategy (routine coronary angiography, n=52) or a conservative strategy (coronary angiography only in patients with recurrent ischemia or heart failure during hospitalization, n=52). The main endpoint was the composite of all-cause mortality, AMI, and readmission for cardiac problems during follow-up. The invasive strategy failed to reduce the incidence of the primary outcome (incidence rate ratio, 0.946; 95% confidence interval [95%CI], 0.946-1.918), although there was a tendency for reduced mortality and mortality or reinfarction at 3 months, indicating that the comorbidity weight could dilute the long-term benefits of revascularization. The authors propose exploration of the tendency for short-term benefits in larger studies. In addition, the low revascularization rate in the invasive branch (58%) could reflect the severity and complexity of the coronary anatomy in these patients.
The prognostic impact of frailty in ACS has been confirmed in a registry3 that included 202 patients aged 75 years or older with type I AMI treated in 4 Spanish hospitals. Frailty was evaluated using the SHARE-FI index, which evaluates self-perceived fatigue, appetite, functional difficulties, physical activity, and grip strength. In total, 71 patients (35.1%) met the criteria for frailty. The frail patients were older and had more comorbidities (mean Charlson Comorbidity Index, 8.4 vs 6.6; P<.001). Despite showing a higher-risk profile, with higher scores on the GRACE (154.4 vs 141.0; P<.001) and CRUSADE (48.2% vs 34.1%; P<.001) scales, frail patients underwent fewer coronary angiography studies (66.2% vs 93.1%; P<.001). The main endpoint (cardiac death or infarction during hospitalization) was more frequent in frail patients (9.9% vs 1.5%; P=.006), largely due to higher mortality. The incidence of major bleeding (a hemoglobin decrease > 3g/dL or need for surgery or transfusion during hospitalization) was also higher in frail patients (19.7% vs 9.2%; P=.032). Despite the small sample size, frailty could predict mortality independently of age, sex, creatinine, diabetes mellitus, and GRACE score.
In a subsequent publication, González Salinas et al.4 analyzed the ability of frailty to predict bleeding risk in 190 patients from the same series. Frailty predicted a higher incidence of bleeding complications, despite a lower use of dual antiplatelet therapy and the invasive strategy; this predictive ability was independent of age (hazard ratio, 2.7; 95%CI, 1.2-5.7; P=.012).
Thus, these findings strengthen the association of frailty with conservative treatment and worse prognosis in ACS. The question underlying all of these findings is whether frail patients should really be treated differently.5 In an attempt to respond to this question, the LONGEVO-SCA registry6 has been designed, with funding from the Geriatric Cardiology Section of the Spanish Society of Cardiology. The registry plans to include 500 patients aged 75 years or older with NSTEACS from more than 50 Spanish hospitals; a comprehensive geriatric assessment will be performed (frailty, comorbidities, functional and cognitive status, quality of life) and the researchers will analyze the association of these variables with treatment and prognosis at 6 months.