December 2017 marked 50 years since Dr. Barnard performed the first ever heart transplantation (HTx) in Cape Town, South Africa. Since then, more than 100 000 patients worldwide have received a HTx, about 8000 in Spain alone.1 In these 5 decades, HTx has been indisputably consolidated as the alternative treatment of choice for patients with refractory heart failure (HF).
Thanks to the subsequent successive therapeutic advances that have been made, the average survival of HTx recipients has progressively increased, reaching about 12 years in the most recent cohorts.1 In parallel, there has been an expansion in the indications for the procedure, which currently has few absolute contraindications. The main Achilles heel of HTx is still the small number of available organs, which makes it difficult for this therapy to extend to the entire population of patients who could benefit from it.
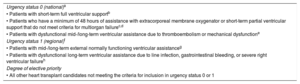
The Spanish heart donor distribution system is based on priority criteria that are agreed among all HTx groups in the country and were extensively revised in 2017 (Table). The current system prioritizes candidates requiring short-term mechanical circulatory assist devices, who are conferred the highest priority level, called “urgency status 0” (high-urgent), given their high risk of short-term death. In recent years, the prolongation of waiting times for HTx has caused a progressive increase in the number of candidates receiving a transplantation through an urgent priority code.1
Priority Criteria for the Distribution of Heart Donors in Adult Patients in Spain in 2017
| Urgency status 0 (national)a |
| • Patients with short-term full ventricular supportb |
| • Patients who have a minimum of 48 hours of assistance with extracorporeal membrane oxygenator or short-term partial ventricular support that do not meet criteria for multiorgan failurec,d |
| • Patients with dysfunctional mid-/long-term ventricular assistance due to thromboembolism or mechanical dysfunctione |
| Urgency status 1 (regional)f |
| • Patients with mid-/long-term external normally functioning ventricular assistanceg |
| • Patients with dysfunctional long-term ventricular assistance due to line infection, gastrointestinal bleeding, or severe right ventricular failureh |
| Degree of elective priority |
| • All other heart transplant candidates not meeting the criteria for inclusion in urgency status 0 or 1 |
Table prepared with data from the Spanish National Transplant Organization.
The multicentre study ASIS-TC2 reviewed the results of the Spanish protocol for high-urgent HTx during the 2010 to 2015 period. This work showed the good performance of the system, which enabled 79% of the patients included in the waiting list with the highest priority level to receive a HTx with an average delay slightly longer than 7 days. In this series, early mortality after urgent HTx was high, especially among patients requiring preoperative support with biventricular devices or extracorporeal membrane oxygenation.
Another consequence of the limited availability of heart donors is the progressive increase in their average age and the acceptance of organs with long ischemia times.1 Although some studies have shown good HTx results with these suboptimal donors, there is still reluctance regarding its widespread use. There is controversy as well, such as the need to perform angiography to exclude coronary heart disease from all donors older than 60 years.
Recently, some strategies have been proposed to increase the number of potential heart donors. First and foremost, ex vivo normothermic perfusion systems of the donated heart3 allow the transport of beating and metabolically active hearts, which increases their ischemic tolerance and preserves their functionality. Some groups have also presented promising initial results from the use of hearts of deceased donors after circulatory-determined death.4 Finally, some countries have implemented scouting programs involving the retrieval teams of the transplant centers, achieving a significant increase in the proportion of donated hearts that are finally implanted in a recipient.
In the current context of a limited availability of heart donors, the development of long-term left ventricular assist devices (LVADs) is of particular interest. In recent years, intracorporeal continuous-flow LVADs have replaced other support modalities, due to their excellent results in terms of survival and quality of life, whether when used a bridge to HTx or as destination therapy.
In this field, the most recent advance is the third-generation LVADs, whose best-known examples are the Heartware HVAD and the Heartmate III. These devices are characterized by their modern system of magnetic levitation-enabled friction-free rotation, which theoretically offers certain advantages in terms of biocompatibility and long-term durability. In addition, given their small size, they can be implanted using a less invasive surgical approach that does not necessarily require a median sternotomy. Two multicentre clinical trials evaluating the results of these new third-generation LVADs were published in 2017.
In the MOMENTUM study 3,5 294 patients with refractory HF were randomized to receive either a Heartmate II or Heartmate III LVAD as a bridge to HTx or as destination therapy. The patients treated with a Heartmate III had a longer disabling stroke-free survival or reoperation for LVAD removal or replacement due to dysfunction at 6 months of follow-up. This result was due almost exclusively to the absence of pump thrombotic events in the group treated with the Heartmate III, with no significant differences between the groups in terms of the other events analyzed.
In the ENDURANCE study,6 297 patients were randomized to receive either a Heartmate II LVAD or Heartware HVAD as destination therapy. No significant differences were observed between the 2 groups regarding the primary composite study end point (disabling stroke-free survival or LVAD removal due to dysfunction at 2 years of follow-up). Patients treated with the Heartware HVAD had a lower incidence of LVAD removal due to dysfunction than those treated with the Heartmate II; however, the incidence of disabling stroke was higher in the Heartware HVAD group.