The use of coronary physiology as an invasive method for identifying hemodynamically significant coronary stenosis in stable patients dates back to the 1990s. However, following the results of the DEFER trial1 and particularly the FAME trial,2 which demonstrated that the use of fractional flow reserve (FFR) to guide revascularization reduced major adverse cardiac events (MACE) compared with angiography-guided revascularization, the technique has gained importance in clinical decision-making regarding patients with multivessel coronary disease.
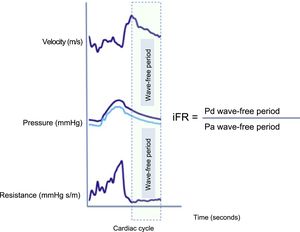
Against this background, the emergence in recent years of a new invasive index for assessing coronary disease severity at rest without the need for induction of hyperemia has revolutionized the scientific community. Specifically, the instantaneous wave-free ratio (iFR) (Figure 1) shows a similar or even better ability than FFR to precisely detect myocardial ischemia. However, until 2017, there were no clinical studies that compared the use of iFR-guided vs FFR-guided revascularization. The DEFINE-FLAIR trial3 included more than 2000 patients with intermediate coronary stenosis, with questionable severity, who were randomized to receive FFR-guided or iFR-guided revascularization. That trial was a noninferiority study for MACE at 1 year of follow-up. The cutoff values for indication for revascularization were FFR ≤ 0.80 and iFR ≤ 0.89. Although a similar number of lesions were analyzed in both groups, there were fewer functionally significant lesions in the iFR group (451 vs 557; P = .004). Consequently, significantly fewer lesions were revascularized in the iFR group than in the FFR group. At 1 year of follow-up, the primary endpoint of noninferiority of iFR to FFR was reached. In addition, there were fewer adverse events and symptoms related to adenosine use during the procedure and the procedure time was shorter (4.5min) in the iFR group.
Illustration of microvascular flow velocity, pressure and resistance waves during the cardiac cycle. There is a period during diastole when flow velocity is high and pressure is low. This leads to lower microvascular resistance during the wave-free period. The iFR is calculated using an automatic algorithm that calculates the ratio at rest between the distal coronary pressure and the aortic pressure during the wave-free period. iFR, instantaneous wave-free ratio; Pa, aortic pressure; Pd, distal coronary pressure.
The second published study was the iFR-SWEDEHEART trial,4 with a very similar design to the DEFINE-FLAIR trail. This was a randomized noninferiority trial, with the same primary endpoint. Unlike the previous study, it included a somewhat higher percentage of unstable patients; furthermore, although the number of stenoses assessed was significantly higher in the iFR group, the number of functionally significant lesions was significantly lower in that group. Once again, iFR use was demonstrated to be noninferior to FFR for incidence of events at 1 year of follow-up (Table 1). Research on iFR as a useful diagnostic tool in patients with coronary disease culminated with the SYNTAX II study.5 This was a multicenter, all-comers, open-label, single arm study that compared clinical outcomes in patients with multivessel disease revascularized according to the SYNTAX II strategy with historical cohorts from the SYNTAX I study. The SYNTAX II strategy includes the use of the SYNTAX II score6 (a clinical tool that combines anatomical and clinical characteristics) for risk assessment according to revascularization method. All patients with multivessel lesions were presented in a multidisciplinary (Heart Team) session; the study included patients whose probability of events at 4 years was similar whether they received surgical or percutaneous revascularization. All patients were revascularized with coronary physiology guidance (in 73.8% of the lesions, iFR was used alone) and stents were optimized with intravascular ultrasound. Finally, 454 patients were considered suitable for angioplasty. At 1 year of follow-up, the SYNTAX II strategy was superior to the SYNTAX I PCI cohort due to a significant reduction in MACE rate, mainly due to a lower incidence of infarction and need for revascularization. The rates of all-cause mortality and death from stroke were similar in the 2 groups, and the rate of definite stent thrombosis was lower in the SYNTAX II group. In conclusion, iFR has been confirmed as a useful parameter in the diagnosis and treatment of patients with multivessel lesions; this will simplify the procedure and will undoubtedly promote its rapid uptake in catheterization laboratories nation-wide.
Table Summarizing the Different Studies That Have Used Coronary Physiology to Guide Percutaneous Revascularization
| Trial | Trial design | No. of patients | Endpoint | Results |
|---|---|---|---|---|
| DEFER1 | Randomized 3 groups: – FFR> 0.75 randomized to PTCA or deferred treatment – FFR <0.75 PTCA (reference group) | 325 patients sent for PTCA without documented ischemia | Absence of adverse cardiac events at 24 months of follow-up | > 0.75 group: event-free survival similar between the PTCA group and deferred group (83% vs 89%) <0.75 group: significant reduction in events (78%) |
| DEFER-15 YEARS2 | — | — | — | Mortality was similar in the 3 groups: 33.0% in the deferred group, 31.1% in the PTCA group, and 36.1% in the reference group (P=.79). The rate of myocardial infarction was significantly lower in the deferred group (2.2%) than in the PCTA group (10.0%) (P = .03) |
| FAME3 | Randomized angiography-guided vs FFR-guided (> 0.80) revascularization | 1005 with multivessel disease | Mortality rate, nonfatal AMI and need for revascularization at 1 year of follow-up | Rate of events lower in the FFR-guided group (13.1% vs 18%; P=.029) |
| FAME-5 YEARS2 | — | — | — | MACE rate similar at 5 years (31% vs 28%; P=.31) |
| FAME-II2 | Patients with at least 1 lesion with FFR <0.80 randomized to PCI or medical treatment | 1220 with stable angina | Combined endpoint of death from all causes, nonfatal AMI, and urgent revascularization at 2 years | The MACE rate was significantly lower in the PCI group (8.1% vs 10.5%; P <.001) |
| DEFINE-FLAIR3 | Patients with intermediate lesions randomized to revascularization with iFR or with FFR iFR ≤ 0.89 or FFR ≤ 0.80 | 2492 (80% were stable) | Combined endpoint of death from all causes, nonfatal AMI and unplanned revascularization at 1 year | The rate of events was 6.8% in the iFR group and 7.0% in the FFR group (P <.001 for noninferiority) |
| SWEDE-HEART4 | Patients with intermediate lesions randomized to revascularization with iFR or with FFR iFR ≤ 0.89 or FFR ≤ 0.80 | 2037 with intermediate coronary lesions | Combined endpoint of death from all causes, nonfatal AMI and unplanned revascularization at 1 year | The rate of events was 6.7% in the iFR group and 6.1% in the FFR group (P <.007 for noninferiority) |
AMI, acute myocardial infarction; FFR, fractional flow reserve; iFR, instantaneous wave-free ratio; MACE, major adverse cardiac events; PCI, percutaneous coronary intervention; PTCA, percutaneous transluminal coronary angioplasty.
.