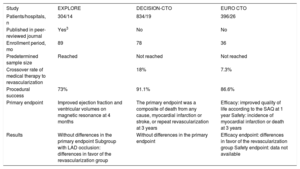
Chronic occlusion is currently the most complex setting for percutaneous treatment of coronary lesions. Until recently, this type of intervention had a success rate of about 50% to 60%, and the main limiting step was the crossing of the coronary guidewire to the distal true lumen. Despite these poor results, the international interventional cardiologist community was not discouraged and continued to perform new procedures while incorporating new techniques and new materials1; the current success rates in specialized units are about 85% to 90%. Notably, during the 30-year history of this type of procedure,2 no randomized study has compared its outcomes with those of medical therapy. However, 3 such articles have been published in the last year: EXPLORE,3 DECISION-CTO (NCT01078051), and EURO CTO (NCT01760083). Each of these studies has completely different inclusion criteria, primary endpoints, and results (Table). Crucially, none found a significant reduction in “hard” endpoints such as cardiac mortality, which is why these results have caused some pessimism in the international scientific community about the use of percutaneous revascularization in patients with chronic occlusions. However, before changing our clinical practice, we need to discuss some general and specific aspects that may have influenced the results of these studies. First, there are 3 situations of interest: a) the procedural success rate is variable (73%-91%) and lower than that of other types of coronary revascularizations and, of course, if it is low, it greatly penalizes the intervention group; b) the number of patients that cross from one group to another, if high, affects the validity of the comparison; and c) a long inclusion period in high-volume centers means that many patients eligible for the study have not been included. Therefore, the findings cannot be generalized and are applicable only to a selected group of patients who are often the least symptomatic.
Randomized Studies of Chronic Occlusions: Percutaneous Revascularization Versus Medical Therapy
| Study | EXPLORE | DECISION-CTO | EURO CTO |
|---|---|---|---|
| Patients/hospitals, n | 304/14 | 834/19 | 396/26 |
| Published in peer-reviewed journal | Yes3 | No | No |
| Enrollment period, mo | 89 | 78 | 36 |
| Predetermined sample size | Reached | Not reached | Not reached |
| Crossover rate of medical therapy to revascularization | 18% | 7.3% | |
| Procedural success | 73% | 91.1% | 86.6% |
| Primary endpoint | Improved ejection fraction and ventricular volumes on magnetic resonance at 4 months | The primary endpoint was a composite of death from any cause, myocardial infarction or stroke, or repeat revascularization at 3 years | Efficacy: improved quality of life according to the SAQ at 1 year Safety: incidence of myocardial infarction or death at 3 years |
| Results | Without differences in the primary endpoint Subgroup with LAD occlusion: differences in favor of the revascularization group | Without differences in the primary endpoint | Efficacy endpoint: differences in favor of the revascularization group Safety endpoint: data not available |
LAD, left anterior descending artery; SAQ, Seattle Angina Questionnaire.
The EXPLORE study3 randomized 304 patients with AMI treated with primary angioplasty and with chronic occlusion of a vessel in a second stage to medical therapy or percutaneous revascularization of the chronic occlusion. The primary endpoint was an improvement in ejection fraction and ventricular volumes on magnetic resonance imaging at 4 months. In the general study, there were no differences in the ejection fraction between the groups (44.1%±12.2% versus 44.8%±11.9%; P=not significant). However, in the subgroup of patients with chronic occlusion of the left anterior descending artery, the differences were significant in favor of the group of patients who underwent percutaneous coronary intervention (47.2%±12.3% versus 40.4%±11.9%; P <.02). One of the major limitations was the low rate of primary success (73%), which was below the current standards. The main features of this study are summarized in the Table.
In the DECISION-CTO study, 834 patients with chronic occlusion were randomized to medical therapy or percutaneous intervention. The primary endpoint was the composite of death from any cause, myocardial infarction, stroke, or repeat revascularization at 3 years. Although there were no significant differences between the groups, this study also suffers from some limitations. For example, the predetermined sample size (1284 patients) was not reached due to slow inclusion (6.5 years) in high-volume centers, meaning that a methodological deficit can be added to the above limitation regarding the applicability of the results. In addition, the crossover rate from the medical therapy group was relatively high (18%).
Finally, the EURO CTO study included 396 patients with chronic occlusion who were randomized 2:1 to percutaneous intervention or medical therapy. The primary efficacy endpoint was an improvement in quality of life according to the Seattle Angina Questionnaire (SAQ) at 1 year; the safety endpoint was the incidence of myocardial infarction or death at 3 years. The study was positive with regard to the efficacy endpoint; however, the 3-year follow-up data are not available. Because this study also failed to reach the predetermined sample size (600 patients for the efficacy endpoint and 1200 for the safety), it also has methodological limitations similar to those already mentioned.
Hoping that a randomized study with sufficient statistical power and without major limitations can demonstrate reduced mortality, the scientific community will continue to be divided between those who believe that there is some evidence for its usefulness based on observational studies4,5 and clinical experience (Figure) and those who maintain that there is no evidence to systematically recommend the interventionist strategy. In the meantime, the latest North American and European clinical guidelines for revascularization both confer the percutaneous treatment of chronic occlusion in experienced centers a IIA level of evidence, grade of recommendation B.
Changes in ejection fraction on magnetic resonance imaging 3 months after the procedure in a patient with chronic occlusion of the RCA and LAD, which were recanalized in 2 stages. EDV, end-diastolic volume; ESV, end-systolic volume; LAD, left anterior descending artery; LVEF, left ventricular ejection fraction; RCA, right coronary artery.
.