From 2015 to 2016, several important studies have been published on ischemic heart disease. The present article will mention some of the most salient studies.
In chronic ischemic heart disease, a notable publication was the report of the long-term results of the COURAGE1 trial. In this trial, 2287 stable patients were randomized to initially receive optimal medical treatment or additional coronary angioplasty. The data from 1211 patients (53% of the original sample) with a median follow-up of 6.2 years are in line with those of the original study; that is, no differences were found in mortality between the 2 treatment groups (24% vs 25%; P=.76).1
Several recent studies have reported that control of cardiovascular risk factors is inadequate, even in secondary prevention. The EVITA2 trial analyzed the efficacy of varenicline in achieving smoking cessation in patients with a recent acute coronary syndrome. In this multicenter, controlled, double-blind trial, 302 patients hospitalized for an acute coronary event (mean age, 55 years; 75% males; ST-segment elevation in 56%; mean number of cigarettes smoked, 21/d) were randomized to receive varenicline or placebo for 12 weeks. The primary aim was abstinence at 24 weeks, confirmed by determination of exhaled carbon dioxide. Patients who received the drug smoked significantly less than the control cohort (abstinence, 47.3% vs 32.5%), with a similar rate of adverse events at 30 days after treatment discontinuation.2
Beyond cardiovascular risk, a Swedish group has confirmed the importance of periodontal disease in the genesis of myocardial infarction. The PAROKRANK3 trial researchers analyzed 805 patients aged<75 years with a first myocardial infarction (mean age, 62 years; 81% male) using a dental examination and orthopantomography, and compared them with a similar, matched control group. Periodontal disease was more common in the cases (43% vs. 33%), and the authors reported an increased risk of infarction in the case group (odds ratio,1.49; 95% confidence interval, 1.03-1.60) after adjustment for other relevant variables (smoking, diabetes, educational level, and marital status).3
Acute coronary syndrome is increasingly common in our setting and is a leading cause of hospitalization in elderly persons, who comprise a growing percentage of the population.4 Although a prompt, invasive strategy is currently recommended in these patients, data from clinical trials are scarce in this age group. To fill this gap, Tegn et al.4 published the After Eighty study, a multicenter, controlled European trial in patients aged 80 years or older, hospitalized for a non–ST-segment elevation acute myocardial infarction. Participants were randomized to receive a prompt invasive strategy or optimal medical treatment (229 and 228 patients, respectively). After a mean follow-up of 1.53 years, an intention-to-treat analysis revealed that the incidence of the composite primary outcome measure (myocardial infarction, stroke, urgent revascularization requirement, and death) was 40.6% in patients assigned to the invasive strategy vs 61.4% in those who received medical treatment alone. Separate analyses of the individual variables yielded significant differences for infarction and urgent revascularization, but not for stroke or death. With a similar rate of major complications (1.7% and 1.8%), the authors concluded that the prompt, invasive strategy is superior to the conservative approach, with no clear differences in bleeding complications. However, they also state that the differences in efficacy diminished over time.
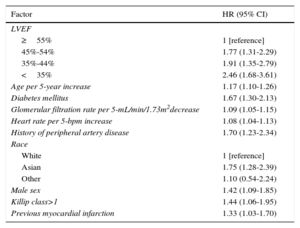
Another hot topic is characterization of the probability of sudden cardiac death following a myocardial infarction. Hess et al.5 carried out a joint analysis of 4 clinical trials (APPRAISE-2, PLATO, TRACER, and TRILOGY-ACS) with 37 555 patients who experienced a non–ST-segment acute coronary syndrome (mean age, 65 years; 67.4% males), with the aim of determining the incidence of sudden death and deaths due to cardiovascular causes after a mean follow-up of 12.1 months. The cumulative incidence of sudden cardiac death was 0.79%, 1.65%, and 2.27% at 6, 18, and 30 months, respectively (one third of cardiovascular deaths). The authors conclude that adequate clinical stratification is feasible and suggest related factors and propose a risk score (Table).
Factors Associated With the Development of Sudden Cardiac Death Following a Non–ST-segment Myocardial Infarction
| Factor | HR (95% CI) |
|---|---|
| LVEF | |
| ≥55% | 1 [reference] |
| 45%-54% | 1.77 (1.31-2.29) |
| 35%-44% | 1.91 (1.35-2.79) |
| <35% | 2.46 (1.68-3.61) |
| Age per 5-year increase | 1.17 (1.10-1.26) |
| Diabetes mellitus | 1.67 (1.30-2.13) |
| Glomerular filtration rate per 5-mL/min/1.73m2decrease | 1.09 (1.05-1.15) |
| Heart rate per 5-bpm increase | 1.08 (1.04-1.13) |
| History of peripheral artery disease | 1.70 (1.23-2.34) |
| Race | |
| White | 1 [reference] |
| Asian | 1.75 (1.28-2.39) |
| Other | 1.10 (0.54-2.24) |
| Male sex | 1.42 (1.09-1.85) |
| Killip class>1 | 1.44 (1.06-1.95) |
| Previous myocardial infarction | 1.33 (1.03-1.70) |
95% CI, 95% confidence interval; HR, hazard ratio; LVEF, left ventricular ejection fraction
Created with data reported by Hess et al.5
Finally, in the PRAGUE-186 trial, presented at the 2016 Congress of the European Society of Cardiology held in Rome, 1230 patients with ST–segment-elevation myocardial infarction were randomized to receive antiplatelet therapy with either prasugrel or ticagrelor. No relevant differences in efficacy or safety were detected between the 2 drugs at 7 and 30 days of follow-up. The study was criticized during the presentation session because it lacked power and was prematurely terminated (according to the authors, for futility).6
CONFLICTS OF INTERESTE. Abu-Assi is an Associate Editor of Revista Española de Cardiología.