The Interventional Cardiology Association of the Spanish Society of Cardiology (ACI-SEC) presents its annual report on the activity for 2019.
MethodsAll Spanish centers with a catheterization laboratory were invited to participate. Data were introduced online and analyzed by an external company together with the Steering Committee of the ACI-SEC.
ResultsA total of 119 centers participated (83 public, 36 private). In all, there were 165124 diagnostic studies (4.7% more than in 2018). The use of pressure wire and intravascular ultrasound increased by 20% and that of optical coherence tomography by 8.4%. The number of percutaneous coronary interventions (PCI) rose by 4.5% (75 819 procedures). Of these, 22529 were performed in the acute myocardial infarction setting, with 91.8% being primary PCI (6.3% increase). The mean number of primary PCIs per million inhabitants increased to 439. Among PCIs, access was radial in 88.3%. There were 4281 transcatheter aortic valve implantations (21.0% increase), with an average of 90.9 per million inhabitants. Mitral valve repair also rose by 17.4% (n=385), left atrial appendage closure by 43.0% (n=921) and patent foramen ovale closure by 38.1% (n=710).
ConclusionsIn 2019, the use of intracoronary diagnostic techniques increased, as did that of diagnostic and therapeutic coronary procedures, mainly in primary PCI. Of particular note was the marked increase in the number of transcatheter aortic valve implantations, as well as in the number of mitral valve repairs and left atrial appendage and patent foramen ovale closure procedures.
Keywords
One of the primary tasks of the Steering Committee of the Interventional Cardiology Association of the Spanish Society of Cardiology (ACI-SEC) is the collection of health care activity data from Spanish catheterization laboratories to prepare the annual registry. This work has been carried out uninterrupted for 30 years.1–28 The information obtained is highly useful for understanding the changes over time in interventional cardiology, overall and by autonomous community, detecting variations between different regions in terms of the implementation of the distinct percutaneous techniques, determining the outcomes of health care networks, such as that of the Infarction Code Program, and identifying opportunities for improvement. In addition, the data can be compared with those of other countries.
Data are contributed on a voluntary basis via an online database. The variables of the registry are revised every year to keep pace with the incorporation of new techniques and technologies and reflect the actual activity of laboratories and to remove or modify those variables that have become outdated. An external company analyzed the data collected and performed data cleaning, in conjunction with members of the Steering Committee of the ACI-SEC as well as members of the association itself, given that the preliminary results were presented via an online seminar (June 18, 2020) due to the COVID-19 pandemic, which has necessitated the postponement of the annual meeting of the ACI-SEC this year.
This article represents the 29th report on interventional activity in Spain and collects activity from both public and private centers corresponding to 2019.
METHODSThe registry comprises 630 variables to encompass the diagnostic and therapeutic activity of public hospitals and most private hospitals in Spain. Data collection was performed through an online database via a link that was sent by e-mail to the responsible researcher in each center or through the ACI-SEC website.29 Data were provided voluntarily and without audit. Anomalous data or data that deviated from the trend observed in a hospital were referred to the responsible researcher from the center to be confirmed or corrected.
An external company (Tride, Madrid) analyzed the data, with the help of ACI-SEC members, who reviewed the results, detected anomalous data, and compared the data with those of previous years. The results are published in this article, but a preliminary draft was presented as a slideshow in the abovementioned online seminar.
As in previous years, the population-based calculations for both Spain and each autonomous community were based on the population estimates of the Spanish National Institute of Statistics up until July 1, 2019, as published online. The Spanish population was estimated to be 47 100 399 inhabitants (based on provisional data). The number of procedures per million population for the country as a whole was calculated using the total population.30
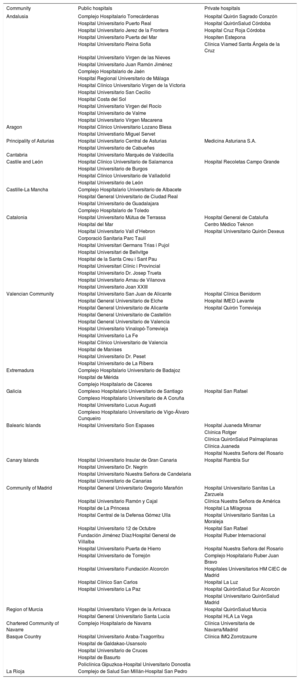
RESULTSInfrastructure and resourcesA total of 119 hospitals participated in this registry, a higher number than in previous years (107 in 2017 and 109 in 2018); 83 were public and 36 were private (appendix 1). This high participation effectively represents Spanish catheterization activity. There were 263 catheterization laboratories: 148 (56.3%) were exclusively for cardiac catheterization, 70 (26.6%) were shared rooms, 30 (11.4%) were hybrid rooms, and 15 (15.7%) were supervised rooms.
In terms of staff, there were a total of 502 interventional cardiologists (464 accredited; 92.4%) in these hospitals in 2019. Of the total number of interventional cardiologists recorded, 114 (22.7%) were women, a slight increase vs the previous year (21.4% in 2018). The number of residents in training decreased in 2019 vs the trends seen in previous years (90 in 2018 vs 79 in 2019; a 12.2% decrease). There were 719 registered nurses in the catheterization laboratories and 83 radiology technicians.
Diagnostic proceduresIn 2019, 165 124 diagnostic studies were performed, representing a 4.7% increase vs 2018. This increase was largely due to a higher number of coronary angiograms (140 670 in 2018 vs 145 715 in 2019; a 3.6% increase), with no major changes in other diagnostic procedures.
Regarding the activity per center, 60.5% of the participating hospitals performed more than 1000 diagnostic studies. The radial artery was the access site used in 87.8% of procedures, similar to 2018.
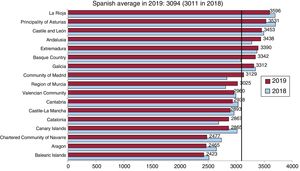
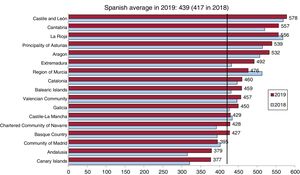
The average number of diagnostic studies was 3506 per million population in Spain (3374 in 2018), whereas that of coronary angiograms was 3094, a slight increase vs 2018 (3011). The distribution of coronary angiograms per million population by autonomous community is shown in figure 1.
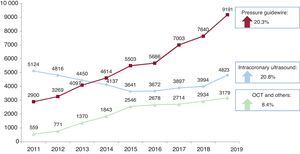
The progressive increase in intracoronary diagnostic techniques seen in previous years was further accentuated in 2019. Both the pressure guidewire, which continued to be the most widely used technique, and intracoronary ultrasound showed an approximate 20% increase vs the previous year, with optical coherence tomography growing by 8.4% (figure 2).
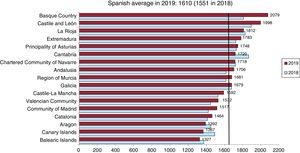
Percutaneous coronary interventionsThe number of percutaneous coronary interventions (PCIs) recorded in 2019 was 75 819, representing a 4.5% increase vs 2018 (75 520). Regarding the distribution per center, 49 hospitals performed between 500 and 1000 annual angioplasties (51 in 2018) while 24 performed more than 1000 (23 in 2018). The PCI/coronary angiogram ratio was 0.52; this figure has remained constant in recent years. The mean number of PCIs per million population increased by 3.8% vs 2018 (1610 in 2019 vs 1551 in 2018) (figure 3). Seven autonomous communities had rates below the Spanish average, the same as in 2018.
In terms of interventional procedures considered complex, there was another increase in the number of procedures performed on the left main vessel (3815 in 2018 and 4133 in 2019; an 8.3% increase). In addition, 79.9% of these procedures involved PCI of the unprotected left main coronary artery. Compared with 2018, there was also a significant 15.1% increase in the number of chronic occlusions and a 15.3% decrease in bifurcation lesions.
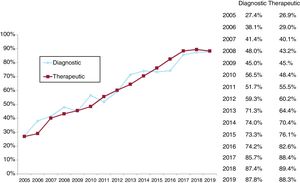
As for diagnostic procedures, radial access was the approach used for most PCIs (88.3%). This figure has been stable in recent years and consolidates this access site as the most widely used approach. The changes in radial access since 2005 are shown in figure 4. A practically linear increase was detected until a plateau was reached 3 years ago.
The immediate outcome variables after the PCI were available for between 65% and 77% of the centers, depending on the variable considered. In 2019, 95.3% of the procedures were completed without complications; 1.0% reported severe complications (death, acute myocardial infarction [AMI], or need for urgent cardiac surgery) and only 0.4% reported intraprocedural death.
StentsIn total, 112 845 stents were implanted in 2019, 4.1% more than in the previous year, in line with the increase in PCI activity. The stent/procedure ratio was stable at 1.6. Drug-eluting stents as a percentage of the total number of stents was 93.3%, with no increase vs 2018 after more than 5 years with a progressive increase. The use of bioabsorbable devices fell again, with 224 devices implanted in 2019 (0.2%) vs 488 (0.4%) in 2018. Similar percentages were found vs 2018 for the use of dedicated bifurcation stents (0.2%), self-expanding stents (0.02%), and polymer-free stents (4.9%).
Other devices and procedures used in percutaneous coronary interventionThe use of plaque modification techniques grew again, paralleling the increased treatment of more complex lesions. At 1635 procedures, rotational atherectomy was the most widely used technique, with a 7.8% increase vs 2018. Intracoronary lithotripsy was the technique showing the most growth, with almost 8 times the 2018 number (a 670.2% increase: 47 vs 362 procedures).31 In addition, there was a 20.4% increase in laser atherectomy procedures (88 vs 106) and an 8.7% increase in the use of special balloons.
Drug-coated balloon use grew by 16.9% (2727 in 2018 and 3188 in 2019).
The implantation of short-term circulatory assist devices during complex interventions expanded, mainly due to the Impella, whose use increased by 69.1% (149 in 2018 and 252 in 2019). Extracorporeal membrane oxygenation grew by 3.7% (109 in 2018 and 113 in 2019), whereas balloon pump use declined by 5.4% (1083 in 2018 and 1025 in 2019).
Finally, there was an increase in other PCI procedures: septal ablation (98 in 2018 vs 114 in 2019), coronary fistula closure (29 vs 34), and stem cell infusion (10 vs 25).
Percutaneous coronary interventions in acute myocardial infarctionAfter 2 years with no changes in the numbers of AMI interventions, there was a 6.0% increase in 2019 (21 261 in 2018 vs 22 529 in 2019). At 91.8%, the percentage of primary angioplasties in AMI was practically identical to that of 2018, probably because it is reaching a plateau. These percentages were similar for the pharmacoinvasive strategy. After fibrinolysis, 557 rescue PCIs were recorded (2.5% of the total number of AMI interventions), as well as 1282 delayed or elective PCIs (5.7% of the total number of AMI interventions).
Primary PCI accounted for 27.3% of all angioplasties. The average number of primary PCIs per million population in Spain increased again (382 in 2017, 417 in 2018, and 439 in 2019). Almost all of the autonomous communities showed a higher primary angioplasty rate last year (figure 5). There was an increase in the number of centers that performed more than 300 primary angioplasties per year, from 21 to 26, and, at the other extreme, those that performed less than 50, from 23 to 34.
In terms of the technical aspects of AMI treatment, and in line with what occurred with diagnostic procedures and PCI outside the AMI setting, the preferred approach was radial, which was used in 96.8% of procedures (calculated based on centers reporting this figure). The same occurred with the use of drug-eluting stents, with a median procedural use of 99%. The number of procedures performed using thrombus extractor devices fell slightly, from 29.2% in 2018 (6205) to 26.8% in 2019 (6036).
Finally, immediate outcome variables after PCI were available for 75 of the participating centers, with an angiographic success rate of 94.4% and a 2.4% rate of severe complications (delayed-onset shock, need for revascularization surgery, or death).
Percutaneous coronary interventions in structural heart diseaseIn 2019, 549 valvuloplasties were recorded in adults, 323 (59.7%) on the aortic valve, 189 (34.9%) on the mitral valve, and 29 (5.4%) on the pulmonary valve. After a slight increase in 2018, the number of mitral valvuloplasties continued the decrease begun some years ago; 36 fewer such procedures were performed in 2019 vs 2018. There were 5 cases of severe mitral regurgitation and 2 of cardiac tamponade (1 patient had both complications). The number of isolated aortic valvuloplasties, not connected to transcatheter aortic valve implantation (TAVI), increased again, with 55 more procedures than in 2018. Two severe aortic regurgitations were reported, as well as 10 deaths.
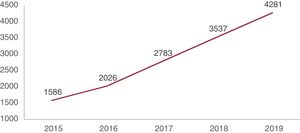
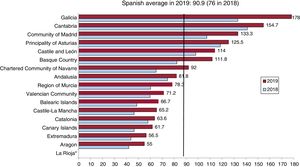
TAVI showed another major increase. This increase has been practically linear in the last 5 years (figure 6). A total of 4281 TAVIs were performed in 2019, representing a 21.0% increase vs the previous year (3537 in 2018). The average number of PCIs per million population in Spain increased from 76 in 2018 to 90.9 in 2019. All autonomous communities showed marked growth in TAVI performance, with Galicia, Cantabria, Madrid, Principality of Asturias, Castile and León, the Basque Country, and the Chartered Community of Navarre showing an above-average number of implantations per million population (figure 7). Most patients treated were older than 80 years of age (67.4%) and 38.7% had surgical contraindication or high surgical risk; the risk was intermediate in 15.8% and not specified in 48.6%. The type of prosthesis implanted was specified in 3499 patients. The expandable balloon valve was used in 1704 (48.7%), whereas the remaining 1795 procedures (51.3%) involved various types of self-expanding valves. The type of approach was specified in 87.1% of implantations. The percutaneous transfemoral approach was the most widely used, with 3173 procedures (85.2%). The remaining percutaneous approaches, such as the transsubclavian/axillary and transcaval, continued to be rare (0.5% and 0.1% of procedures, respectively). Surgical transfemoral access (n = 333, 8.9%) was the preferred alternative to the percutaneous transfemoral approach. The percentages of surgical transsubclavian/axillary (2.8%), transapical (2.2%), and transaortic (0.2%) approaches were similar to those of 2018.
Regarding in-hospital outcomes, 161 major complications (AMI, stroke, or need for vascular surgery) were reported (3.8%) and conversion to surgery was required in 9 procedures (0.2%), 8 of them urgent. The in-hospital mortality rate was 1.8% (77 patients). In addition, 384 patients (9.0%) required definitive pacemaker implantation.
TAVI was performed after the treatment of other valvular heart diseases in 14 patients in the mitral position (12 in 2018), in 18 in the tricuspid position (9 in 2018), and in 29 in the pulmonary position (25 in 2018).
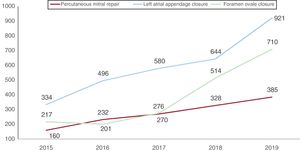
Another notable finding was the significant growth in percutaneous valvular repair with the MitraClip device (figure 8). A total of 385 procedures was recorded, 17.4% more than in 2018, with 538 clips used (1.4 clips per procedure, the same as in 2018).
Functional mitral regurgitation was the most common etiology (60.5%), followed by degenerative (23.7%) and mixed (15.9%). Regarding outcomes, the mitral regurgitation was reduced to ≤ grade 2 in 370 patients (96.1%). Complications were reported in 11 patients.
Percutaneous treatment of tricuspid valve disease also showed significant growth, although it is still rare. A total of 49 such procedures were performed in 2019, a 63.3% increase vs 2018 (30 procedures). The MitraClip was used in 18 patients (the same number as in the previous year), as well as a bicaval valve in 6 patients (2 in 2018) and a tricuspid prosthesis in 7 (1 in 2018). In addition, TAVI was performed in the tricuspid position in 18 patients (9 in 2018).
Regarding nonvalvular structural heart interventions, there was marked growth in atrial appendage closure procedures (42.0%), which increased from 644 procedures in 2018 to 921 in 2019 (figure 8). The Amulet device was used in 513 patients (55.7%), the Watchman in 313 (34.0%), and the LAmbre device in the remaining 95 (10.3%). Twelve procedural complications (tamponade, embolism, or death) were reported (1.3% of the total).
In total, 203 patients underwent paravalvular leak treatment; there was an increase in the closure of aortic leaks (64 in 2018 vs 90 in 2019) and a decrease in that of mitral leaks (130 in 2018 vs 113 in 2019). Complications were reported in 6 patients (embolism or death).
There was an increase in endovascular aortic repair procedures (36 in 2018 vs 50 in 2019), renal denervation (29 vs 39), balloon pericardiotomy (53 vs 64), and percutaneous treatment of pulmonary embolism (112 vs 133). Also implanted were 9 coronary sinus reducer devices and 9 atrial septal defect devices, figures similar to those of 2018.
Percutaneous coronary interventions in adult congenital heart diseaseA total of 1268 procedures were performed for adult congenital heart diseases, 364 more than in 2018, with an increase in practically all procedure types. Foramen ovale closure, in line with the trends of recent years, showed the most growth, with 710 procedures in 2019 vs 514 in 2018 (a 38.1% increase) (figure 8). One device embolization was reported, as well as 5 implantation failures without complications. The number of atrial septal defect closures increased by 17.7% (294 in 2018 and 346 in 2019), with 4 cases of device embolization and 6 of implantation failure without complications. There were 37 patent ductus arteriosus closures (22 in 2018) and 59 atrial septal defect closures (12 in 2018); 59 aortic coarctations were treated (62 in 2018). Finally, 14 more percutaneous pulmonary valve implantations were performed than in 2018 (a total of 59), with a 98% success rate and without major complications.
DISCUSSIONThe registry activity data of the ACI-SEC for 2019 reveal an overall increase in diagnostic and therapeutic activity in Spain. The main findings are that: a) intracoronary diagnostic techniques continue to show significant growth, particularly the pressure guidewire; b) PCI use has increased by about 4.5% vs the previous year; c) the radial access is the approach of choice for both diagnostic and therapeutic procedures, with rates close to 90%; d) after a plateau, the use of PCI in AMI has expanded, due to a 6.3% increase in primary angioplasties; and e) the field of structural heart interventions shows the most growth, particularly TAVI, percutaneous mitral valve repair, and left atrial appendage and patent foramen ovale closures.
The tendency seen in recent years for an expanded use of intracoronary diagnostic techniques was accentuated in 2019. The most commonly used such technique was the pressure guidewire, with a 20% increase vs the previous year. The recommendations in the latest revascularization guidelines,32 together with the scientific evidence on nonhyperemic indices,33–35 have helped to boost the implementation of the technique. Intracoronary ultrasound has also shown growth of 20% (a highly pertinent finding after the decrease until 2015 and the subsequent slow increase) and optical coherence tomography increased by 8.4%. Once again, the more frequent management of complex lesions and better adherence to guidelines have contributed to the adoption of these techniques, which have been proven to improve patient prognosis.32,36
The use of PCI grew by 4.5% from 2018 to 2019 and showed an average of 1610 per million population in Spain. Although this is far below the European average (2478 PCIs per million population),37 the rate has progressively increased in recent years (1551 in 2018). Another noteworthy aspect is the higher treatment of complex lesions such as the left main coronary artery (8.3%, unprotected in 79.9%) or total chronic occlusions (15.1%), with more centers incorporating the technique. In addition, the significant growth in plaque modification devices indirectly indicates the improved management of calcified lesions. Despite the growing complexity of coronary lesions, radial access has been consolidated as the approach of choice in 88.3% of procedures, an indicator of the quality of the interventional activity performed.
After a plateau period, there was a notable increase in PCI procedures in AMI, with 22 529 interventions. Another important finding was the 6.3% increase in the number of primary angioplasties, which represent 91.8% of AMI procedures. The number of primary angioplasties per million population was 439 (417 in 2018), very close to the 468 per million reported as the European average,37 a reflection of the implementation of infarction care networks in all autonomous communities.
The most notable finding concerns structural heart interventions, which is the area showing the most growth, as also seen in previous years. TAVI continues to be the predominant procedure in structural heart interventions, with 90.9 implantations per million population and a marked increase in all autonomous communities. The scientific evidence supporting this technique and the extension of the indication to patients with low and intermediate surgical risk indicates that this increase will continue to be prominent in the coming years.38–42 Percutaneous mitral valve repair also stands out, with a 17.4% increase in the number of procedures. The fall in readmissions due to heart failure and mortality documented in the COAPT study—maintained at 3 years—have reinforced the use of this technique,43 which additionally permits the identification of the ideal candidates for this approach. Although the percutaneous management of the tricuspid valve is still rare, the development of different technologies and the growing interest in this valve disease suggest that major growth will be seen in the coming years.
One notable aspect of structural heart intervention is the increase in atrial appendage closure procedures, related to the fall in complications and improved success in the latest international registries, as well as the publication of consensus documents supporting the usefulness of this technique in selected patients.44,45
Finally, patent foramen ovale closure continued its upward trend due to the scientific evidence showing its superiority over medical therapy in terms of recurrence in patients with cryptogenic stroke.46,47
CONCLUSIONSThe Spanish Registry of Cardiac Catheterization and Interventional Cardiology for 2019 has shown a general increase in diagnostic and therapeutic activity. Notable aspects of the coronary activity include the increase in intracoronary diagnostic techniques and the growth in PCI, largely in the setting of ST-segment elevation AMI and complex coronary lesions. Finally, radial access has been consolidated as the approach of choice in all procedures and exceeds 95% in the context of AMI. The field of structural heart interventions has shown the most expansion, particularly in terms of the number of TAVIs. Percutaneous mitral valve repair, left atrial appendage closure, and patent foramen ovale repair are other procedures showing a significant increase.
CONFLICTS OF INTERESTNone.
The Steering Committee of the ACI-SEC would like to thank the directors of catheterization laboratories throughout Spain and all of their colleagues for their work and dedication, which have enabled fair and first-rate patient care. In addition, we thank those in charge of data collection for their excellent participation in the registry, despite the difficult and exceptional situation created by the COVID-19 pandemic.
| Community | Public hospitals | Private hospitals |
|---|---|---|
| Andalusia | Complejo Hospitalario Torrecárdenas | Hospital Quirón Sagrado Corazón |
| Hospital Universitario Puerto Real | Hospital QuirónSalud Córdoba | |
| Hospital Universitario Jerez de la Frontera | Hospital Cruz Roja Córdoba | |
| Hospital Universitario Puerta del Mar | Hospiten Estepona | |
| Hospital Universitario Reina Sofía | Clínica Viamed Santa Ángela de la Cruz | |
| Hospital Universitario Virgen de las Nieves | ||
| Hospital Universitario Juan Ramón Jiménez | ||
| Complejo Hospitalario de Jaén | ||
| Hospital Regional Universitario de Málaga | ||
| Hospital Clínico Universitario Virgen de la Victoria | ||
| Hospital Universitario San Cecilio | ||
| Hospital Costa del Sol | ||
| Hospital Universitario Virgen del Rocío | ||
| Hospital Universitario de Valme | ||
| Hospital Universitario Virgen Macarena | ||
| Aragon | Hospital Clínico Universitario Lozano Blesa | |
| Hospital Universtiario Miguel Servet | ||
| Principality of Asturias | Hospital Universitario Central de Asturias | Medicina Asturiana S.A. |
| Hospital Universitario de Cabueñes | ||
| Cantabria | Hospital Universitario Marqués de Valdecilla | |
| Castile and León | Hospital Clínico Universitario de Salamanca | Hospital Recoletas Campo Grande |
| Hospital Universitario de Burgos | ||
| Hospital Clínico Universitario de Valladolid | ||
| Hospital Universitario de León | ||
| Castille-La Mancha | Complejo Hospitalario Universitario de Albacete | |
| Hospital General Universitario de Ciudad Real | ||
| Hospital Universitario de Guadalajara | ||
| Complejo Hospitalario de Toledo | ||
| Catalonia | Hospital Universitario Mútua de Terrassa | Hospital General de Cataluña |
| Hospital del Mar | Centro Médico Teknon | |
| Hospital Universitario Vall d’Hebron | Hospital Universitario Quirón Dexeus | |
| Corporació Sanitaria Parc Taulí | ||
| Hospital Universitari Germans Trias i Pujol | ||
| Hospital Universitari de Bellvitge | ||
| Hospital de la Santa Creu i Sant Pau | ||
| Hospital Universitari Clínic i Provincial | ||
| Hospital Universitario Dr. Josep Trueta | ||
| Hospital Universitario Arnau de Vilanova | ||
| Hospital Universitario Joan XXIII | ||
| Valencian Community | Hospital Universitario San Juan de Alicante | Hospital Clínica Benidorm |
| Hospital General Universitario de Elche | Hospital IMED Levante | |
| Hospital General Universitario de Alicante | Hospital Quirón Torrevieja | |
| Hospital General Universitario de Castellón | ||
| Hospital General Universitario de Valencia | ||
| Hospital Universitario Vinalopó-Torrevieja | ||
| Hospital Universitario La Fe | ||
| Hospital Clínico Universitario de Valencia | ||
| Hospital de Manises | ||
| Hospital Universitario Dr. Peset | ||
| Hospital Universitario de La Ribera | ||
| Extremadura | Complejo Hospitalario Universitario de Badajoz | |
| Hospital de Mérida | ||
| Complejo Hospitalario de Cáceres | ||
| Galicia | Complexo Hospitalario Universitario de Santiago | Hospital San Rafael |
| Complexo Hospitalario Universitario de A Coruña | ||
| Hospital Universitario Lucus Augusti | ||
| Complexo Hospitalario Universitario de Vigo-Álvaro Cunqueiro | ||
| Balearic Islands | Hospital Universitario Son Espases | Hospital Juaneda Miramar |
| Clıínica Rotger | ||
| Clínica QuirónSalud Palmaplanas | ||
| Clínica Juaneda | ||
| Hospital Nuestra Señora del Rosario | ||
| Canary Islands | Hospital Universitario Insular de Gran Canaria | Hospital Rambla Sur |
| Hospital Universitario Dr. Negrín | ||
| Hospital Universitario Nuestra Señora de Candelaria | ||
| Hospital Universitario de Canarias | ||
| Community of Madrid | Hospital General Universitario Gregorio Marañón | Hospital Universitario Sanitas La Zarzuela |
| Hospital Universitario Ramón y Cajal | Clínica Nuestra Señora de América | |
| Hospital de La Princesa | Hospital La Milagrosa | |
| Hospital Central de la Defensa Gómez Ulla | Hospital Universitario Sanitas La Moraleja | |
| Hospital Universitario 12 de Octubre | Hospital San Rafael | |
| Fundación Jiménez Díaz/Hospital General de Villalba | Hospital Ruber Internacional | |
| Hospital Universitario Puerta de Hierro | Hospital Nuestra Señora del Rosario | |
| Hospital Universitario de Torrejón | Complejo Hospitalario Ruber Juan Bravo | |
| Hospital Universitario Fundación Alcorcón | Hospitales Universitarios HM CIEC de Madrid | |
| Hospital Clínico San Carlos | Hospital La Luz | |
| Hospital Universitario La Paz | Hospital QuirónSalud Sur Alcorcón | |
| Hospital Universitario QuirónSalud Madrid | ||
| Region of Murcia | Hospital Universitario Virgen de la Arrixaca | Hospital QuirónSalud Murcia |
| Hospital General Universitario Santa Lucía | Hospital HLA La Vega | |
| Chartered Community of Navarre | Complejo Hospitalario de Navarra | Clínica Universitaria de Navarra/Madrid |
| Basque Country | Hospital Universitario Araba-Txagorritxu | Clínica IMQ Zorrotzaurre |
| Hospital de Galdakao-Usansolo | ||
| Hospital Universitario de Cruces | ||
| Hospital de Basurto | ||
| Policlínica Gipuzkoa-Hospital Universitario Donostia | ||
| La Rioja | Complejo de Salud San Millán-Hospital San Pedro |
The data from the Fundación Jiménez Días and the Hospital General de Villalba are grouped.