In 2017 the Cardiovascular Imaging Association of the Spanish Society of Cardiology created the first Cardiovascular Imaging Registry.1 Another online survey was conducted in January 2020 to provide a longitudinal analysis, collecting data from 94 Spanish institutions on activity during the year 2019. Responses were received from 60% of those surveyed; 86% of these were from public institutions, and all autonomous communities except the Canary Islands were represented.
Table 1 lists the human and material resources, as well as the activity levels of the various cardiovascular imaging modalities. A total of 69% of clinicians devoted more than 50% of their work hours to cardiovascular imaging. In echocardiography, 69.3% of machines was less than 10 years old, and more than 50% of those in institutions with more than 500 beds had advanced cardiovascular imaging capabilities (strain and 3D). Records were kept on indications at 47% of echocardiography laboratories, on events at 63%, and on internal quality control at 82%. Clinicians performing echocardiography had obtained accreditation in transthoracic echocardiography (44.2%), transesophageal echocardiography (22.8%), and congenital diseases (4.5%). Scans were performed outside the laboratory by noncardiovascular imaging professionals at 42% of institutions. These were directed scans (up to 67% in emergency rooms) with semiquantitative reports (56%-80%). Scan images were stored in only 60% of cases, although 91% of institutions had storage capability. At 84% of institutions, echocardiography was performed by departments other than cardiology. Agreement on the diagnosis was acceptable or good in 48% of cases in departments supervised by cardiology. Examination results were recorded in only 57% of cases, despite the recommendations of the current consensus document.2
Human and material resources and volume of activity according to hospital size
| Number of beds per site | |||||
|---|---|---|---|---|---|
| <250 | 250-500 | 500-750 | 750-1000 | >1000 | |
| Cardiology department, % | 40 | 80 | 91.6 | 100 | 91.6 |
| Attending physicians in cardiology ward, n | 4 | 12.5 | 19.5 | 28.5 | 30 |
| Cardiovascular imaging section, % | 40 | 90 | 100 | 93.8 | 100 |
| Attending physicians in imaging, n | 1.9 | 3.6 | 4.1 | 4.6 | 4.9 |
| Attending physicians with imaging time > 50%, % | 62 | 47 | 68 | 80 | 74 |
| RNs in imaging, n | 1.2 | 1.5 | 1.7 | 1.6 | 2.5 |
| CNAs in imaging, n | 0.2 | 0.8 | 0.9 | 1.4 | 1.4 |
| MITs in imaging, n | 0 | 0.6 | 0.6 | 0.6 | 0.6 |
| Office staff in imaging, n | 0 | 0.4 | 0.2 | 0.6 | 0.9 |
| Echocardiography machines in cardiology, n | 3 | 6 | 6.5 | 10 | 11 |
| Echocardiography machines in imaging, n | 3 | 4 | 4 | 5 | 5 |
| Ultrasound studies | 2266 | 7599 | 8735 | 12 060 | 12 353 |
| TTE/TEE/stress echocardiography, % | 92/3/4 | 90/3/5 | 90/4/3 | 88/5/3 | 88/4/4 |
| TEE probes, n | 1 | 2 | 3 | 3 | 3 |
| 3D-echocardiography/STE equipment, % | 33/33 | 38/38 | 75/75 | 40/60 | 60/90 |
| Ultrasound devices > 10 years, % | 23 | 33 | 34 | 31 | 29 |
| CT scans, n | 172 | 160 | 304 | 540 | 555 |
| MRI scans, n | 110 | 150 | 435 | 328 | 673 |
| SPECT scans, n | — | 200 | 200 | 532 | 550 |
| MUGA scans, n | — | 20 | — | 10 | 397 |
| PET scans, n | 30 | — | 17.5 | 30 | 50 |
3D, 3-dimensional; CNA, certified nursing assistant; MIT, medical imaging technologist; MUGA, radionuclide ventriculography; PET, positron emission tomography; RN, registered nurse; SPECT, single-photon emission computed tomography; STE, speckle-tracking echocardiography; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography.
Data are expressed as percentages or medians.
Cardiologic studies based on computed tomography (cardiac CT scan) were performed at 35 institutions (64.8%). Eleven of these institutions performed more than 500 scans per year, and 3 performed more than 1000 scans per year. Two specialists participated in 51.4% of cases, only 1 radiologist in 42.9%, and only 1 cardiologist in 5.7%. All cardiac CT scans were acquired using 64-slice scanners with a mean age of 5 years. A cardiologist participated in 63% of scan acquisitions, 78% of analyses, and 67% of report signatures. At 51% of institutions, the cardiology department had a workstation, and the mean time devoted was 8.7h/wk. Radiation exposure levels were recorded at 63% of institutions. A total of 14.7% of cardiologists involved had international accreditation (European, available since 2019).
Cardiac magnetic resonance imaging (cardiac MRI) was performed at 38 (64.8%) of institutions: scan volume was over 500 scans per year at 10 institutions and over 1000 scans per year at 3. Stress MRI was performed at 15 institutions (more than 100 scans/y at 4 institutions), accounting for 7% of all cardiovascular MRI activity. Of these scans, 42.1% were performed jointly, 44.7% only by radiology, and 13.2% only by cardiology. 1.5-T MRI machines were used in 68% of scans, and 3.0-T MRI machines were used in the rest; the mean machine age was 7 years. A cardiologist participated in 67% of scan acquisitions, 76% of analyses, and 67% of report signatures. A workstation was available in the cardiology department at 46% of institutions, and the time devoted was 12.2h/wk. A total of 48.7% of cardiologists involved had international accreditation.
Nuclear medicine was reported at 26 institutions (48.2%): 10 institutions performed more than 500 single-photon emission computed tomography scans per year, and 4 institutions carried out more than 1000. Positron emission tomography was reported at 12 institutions (22.2%), but only 1 institution performed more than 100 scans per year. A total of 4647 ventricular function studies were performed at institutions with echocardiography. Cardiologist participation was lower (21% in scan acquisitions, 38% in analyses, and 35% in signing reports; 5 h/wk). Radiation exposure levels were recorded at 53% of institutions.
In terms of cardiovascular imaging training, 76% of institutions had cardiology residents. The mean length of training was 6.5 months in echocardiography, 1.1 months in cardiac CT, 1.3 months in cardiac MRI, and 0.5 months in nuclear medicine. In addition, 24% of institutions also had postresidency training programs in cardiovascular imaging. Most programs lasted 12 months and covered echocardiography (100%), cardiac MRI (59%), cardiac CT imaging (65%), and nuclear medicine (18%).
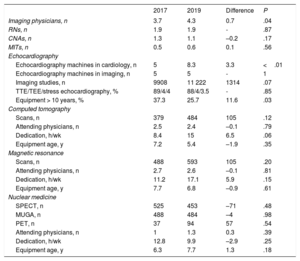
In general, the profile of participating institutions differed from that observed in the first registry in 2017 (institutions with fewer than 500 beds: 27% in 2019 vs 54% in 2017; P <.01). Table 2 provides details on the 34 institutions participating in both registries and reveals an increase in the number of attending physicians, total activity, and time devoted to cardiovascular imaging, as well as modernization of the technology available. A noticeable increase was also seen in the number of echocardiography devices outside the imaging laboratory.
Comparison of the 34 participating institutions in the first and second cardiovascular imaging registry in Spain*
| 2017 | 2019 | Difference | P | |
|---|---|---|---|---|
| Imaging physicians, n | 3.7 | 4.3 | 0.7 | .04 |
| RNs, n | 1.9 | 1.9 | - | .87 |
| CNAs, n | 1.3 | 1.1 | –0.2 | .17 |
| MITs, n | 0.5 | 0.6 | 0.1 | .56 |
| Echocardiography | ||||
| Echocardiography machines in cardiology, n | 5 | 8.3 | 3.3 | <.01 |
| Echocardiography machines in imaging, n | 5 | 5 | - | 1 |
| Imaging studies, n | 9908 | 11 222 | 1314 | .07 |
| TTE/TEE/stress echocardiography, % | 89/4/4 | 88/4/3.5 | - | .85 |
| Equipment > 10 years, % | 37.3 | 25.7 | 11.6 | .03 |
| Computed tomography | ||||
| Scans, n | 379 | 484 | 105 | .12 |
| Attending physicians, n | 2.5 | 2.4 | –0.1 | .79 |
| Dedication, h/wk | 8.4 | 15 | 6.5 | .06 |
| Equipment age, y | 7.2 | 5.4 | –1.9 | .35 |
| Magnetic resonance | ||||
| Scans, n | 488 | 593 | 105 | .20 |
| Attending physicians, n | 2.7 | 2.6 | –0.1 | .81 |
| Dedication, h/wk | 11.2 | 17.1 | 5.9 | .15 |
| Equipment age, y | 7.7 | 6.8 | –0.9 | .61 |
| Nuclear medicine | ||||
| SPECT, n | 525 | 453 | –71 | .48 |
| MUGA, n | 488 | 484 | –4 | .98 |
| PET, n | 37 | 94 | 57 | .54 |
| Attending physicians, n | 1 | 1.3 | 0.3 | .39 |
| Dedication, h/wk | 12.8 | 9.9 | –2.9 | .25 |
| Equipment age, y | 6.3 | 7.7 | 1.3 | .18 |
CNA, certified nursing assistant; MIT, medical imaging technologist; MUGA, radionuclide ventriculography; PET, positron emission tomography; RN, registered nurse; SPECT, single-photon emission computed tomography; TTE, transthoracic echocardiography.
Data are expressed as percentages or medians.
Registries are an essential tool for ensuring consistency within the health system and reducing variability in patient care. The results of this second registry add to information gained from initiatives such as RECALCAR (Resources and Quality in Cardiology Units)3 and are consistent with the criteria described for managing technological assets used in cardiovascular imaging.4 Areas of ongoing improvement include ensuring uniform echocardiography quality both inside and outside the imaging laboratory, enhancing echocardiography resources, increasing certification and participation of the cardiology department in advanced cardiovascular imaging, and using echocardiography studies (particularly when 3D and strain studies are available) rather than radionuclide ventriculography for ventricular function studies.