This report presents the findings of the 2019 Spanish Catheter Ablation Registry.
MethodsData collection was retrospective. A standardized questionnaire was filled by each of the participant centers.
ResultsData sent by 102 centers were analyzed, with a total number of ablation procedures performed of 18549 (the highest historically reported in this registry) for a mean of 181.9±137.0 and a median of 144.5 procedures per center. The ablation targets most frequently treated were atrial fibrillation (n=5164; 27.8%), cavotricuspid isthmus (n=3925; 21.1%) and atrioventricular nodal reentrant tachycardia (n=3768; 20.3%). A new peak is observed in the ablation of atrial fibrillation, increasing the distance from the other substrates. The overall success rate was again 91%. The rate of major complications was 1.9%, and the mortality rate was 0.03%. An electroanatomic mapping system was used in 44.5% of all procedures, with contact force-sensing irrigated catheters become the preferred for complex substrates, as atrial fibrillation (84.8%) or ventricular tachycardia (around 90%). 1.5% of the ablations were performed in pediatric patients.
ConclusionsThe Spanish Catheter Ablation Registry enrolls systematically and uninterruptedly the ablation procedures performed in Spain, showing a progressive increasing in the number of ablations over the years with a high success rate and low percentages of complications.
Keywords
The progressive complexity of catheter ablation techniques and the growing number of laboratories and professionals involved have strengthened the need for reliable and independent data on the treatments used and their outcomes. The Spanish Catheter Ablation Registry, the Official Report of the Heart Rhythm Association (previously the Electrophysiology and Arrhythmias Section) of the Spanish Society of Cardiology, whose 19th edition is presented in this article, represents the largest experience in existence and has been published uninterrupted since 2001.1–18 This annual registry is a voluntary nationwide record of almost all data obtained from arrhythmia units operating in Spain.
Its main objectives are to independently describe the changes over time in the interventional treatment of cardiac arrhythmias in Spain and to provide reliable information on the type of activity performed and the facilities available in Spanish arrhythmia units.
METHODSData were retrospectively collected using a similar methodology to that of the previous year.18 In January 2020, the standardized data collection form, available on the website of the Heart Rhythm Association,19 was sent to all electrophysiology laboratories participating in the association. The completed forms were anonymized. The information collected concerned the technical and human resources available in the arrhythmias units, the procedures performed, and their results and complications.
Since the first registry,1 the arrhythmias and arrhythmogenic substrates have been grouped in 10 categories: atrioventricular nodal reentrant tachycardia (AVNRT), accessory pathways, the atrioventricular node, focal atrial tachycardia (FAT), cavotricuspid isthmus (CTI), macroreentrant atrial tachycardia (MAT), atrial fibrillation (AF), idiopathic ventricular tachycardia (IVT), ventricular tachycardia associated with myocardial infarction (VT-AMI), and ventricular tachycardia not associated with myocardial infarction (VT-NAMI). The following variables common to these substrates were analyzed: number of patients and procedures, including the number of pediatric patients (younger than 15 years), success rate, types of ablation catheter used, and procedure-related complications, including periprocedural death. In addition, the numbers of procedures performed with a navigation system and of those performed without fluoroscopy were also recorded for all substrates. Also analyzed were a number of ablation target-specific variables.
The success rate refers only to the immediate postprocedural data (acute success rate). As for complications, only those occurring during the hospital stay after the procedure were reported.
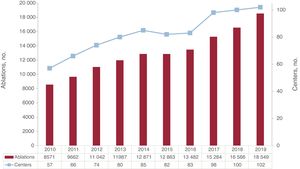
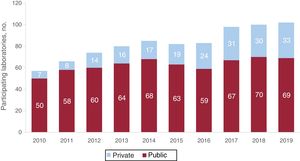
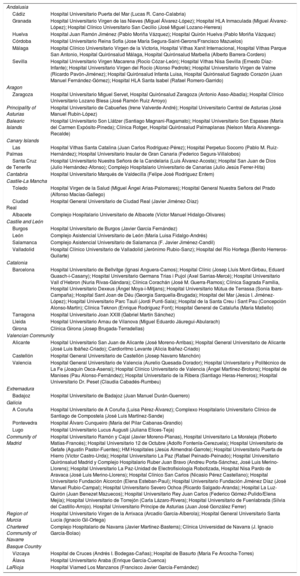
RESULTSThe number of participating centers once again rose to a historic high in 2019, reaching 102 (appendix 1 and appendix 2), a 2% increase vs the previous year (figure 1). Of these, 69 (67.7%) were public and 33 (32.3%) were private, proportions that are similar to those of the previous registry (figure 2).
The number of ablation procedures in 2019 (18 549) was also significantly higher than that of the previous year, with a 12.0% increase (figure 1).
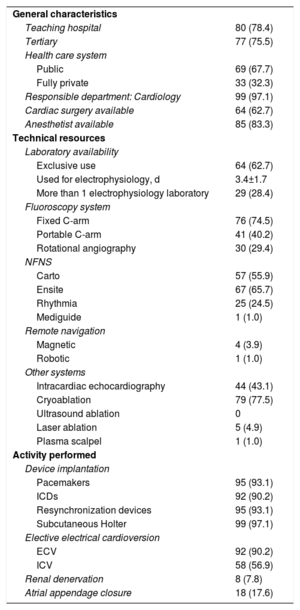
Infrastructure and resourcesThe technical and human resources available in the participating laboratories, as well as the activity performed, are presented in table 1 and table 2.
General characteristics, technical resources, and activity (in addition to catheter ablation) of the 102 electrophysiology laboratories in the 2019 registry
| General characteristics | |
| Teaching hospital | 80 (78.4) |
| Tertiary | 77 (75.5) |
| Health care system | |
| Public | 69 (67.7) |
| Fully private | 33 (32.3) |
| Responsible department: Cardiology | 99 (97.1) |
| Cardiac surgery available | 64 (62.7) |
| Anesthetist available | 85 (83.3) |
| Technical resources | |
| Laboratory availability | |
| Exclusive use | 64 (62.7) |
| Used for electrophysiology, d | 3.4±1.7 |
| More than 1 electrophysiology laboratory | 29 (28.4) |
| Fluoroscopy system | |
| Fixed C-arm | 76 (74.5) |
| Portable C-arm | 41 (40.2) |
| Rotational angiography | 30 (29.4) |
| NFNS | |
| Carto | 57 (55.9) |
| Ensite | 67 (65.7) |
| Rhythmia | 25 (24.5) |
| Mediguide | 1 (1.0) |
| Remote navigation | |
| Magnetic | 4 (3.9) |
| Robotic | 1 (1.0) |
| Other systems | |
| Intracardiac echocardiography | 44 (43.1) |
| Cryoablation | 79 (77.5) |
| Ultrasound ablation | 0 |
| Laser ablation | 5 (4.9) |
| Plasma scalpel | 1 (1.0) |
| Activity performed | |
| Device implantation | |
| Pacemakers | 95 (93.1) |
| ICDs | 92 (90.2) |
| Resynchronization devices | 95 (93.1) |
| Subcutaneous Holter | 99 (97.1) |
| Elective electrical cardioversion | |
| ECV | 92 (90.2) |
| ICV | 58 (56.9) |
| Renal denervation | 8 (7.8) |
| Atrial appendage closure | 18 (17.6) |
ECV, external cardioversion; ICD, implantable cardioverter-defibrillator; ICV, internal cardioversion; NFNS, nonfluoroscopic navigation system.
Values represent No. (%) or mean ± standard deviation.
Changes in the human resources in the electrophysiology laboratories of hospitals participating in the registry since 2010
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Staff physicians | 2.8 | 2.6 | 2.7 | 2.8 | 2.8 | 3.0 | 3.0 | 3.2 | 3.5 | 3.2 |
| Full-time physicians | 2.3 | 2.2 | 2.1 | 2.0 | 1.9 | 2.4 | 2.1 | 2.2 | 2.3 | 2.1 |
| Residents/y | 0.7 | 0.7 | 0.7 | 0.6 | 0.6 | 0.8 | 0.7 | 0.9 | 0.6 | 0.6 |
| RNs | 2.4 | 2.3 | 2.3 | 2.2 | 2.3 | 2.7 | 2.7 | 2.8 | 2.7 | 2.8 |
| RTs | 0.3 | 0.3 | 0.3 | 0.3 | 0.4 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 |
RN, registered nurse; RT, radiologic technologist.
In total, 61 centers (63.7%) were equipped with at least 1 dedicated cardiac electrophysiology laboratory. Most centers (73) had 1 room (77%), 28 had 2 (27.4%), and 1 continues to be the only center with 3 rooms (1%). On average, the laboratory was available on 3.4 ± 1.7 (median, 4) days a week.
Cardiac devices were implanted in all centers, in addition to electrophysiological catheter ablation procedures (table 1).
At least 1 fixed C-arm fluoroscopy system was available in 71 centers (71%) and at least 1 portable C-arm fluoroscopy system in 40 (40%). Most centers (86%) had at least 1 nonfluoroscopic navigation system, 25% of the centers had 2, and 12% had 3. In addition, 29% of the centers had an X-ray system with integrated fluoroscopy (rotational angiography). Intracardiac echocardiography was available in 42 centers (41.8%). The most commonly available ablation technique after radiofrequency was cryoablation, with little change vs the previous year (77% vs 78% in 2018). Other energy sources, such as laser, were rare.
Staff numbers in the electrophysiology laboratories fell slightly last year (table 2), returning to an average of 3.2 staff physicians, with a full-time average of only 2.1. There was at least 1 full-time physician in 77.5% of centers and 2 or more in 61.8%. Furthermore, 39 centers (38%) had fellows (residents), typically 1 (range, 1-10).
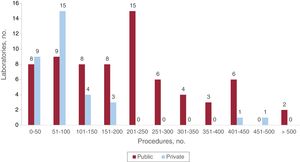
Overall resultsThe changes over time in registry participation are shown in figure 1. There was a notable increase (12% vs 2018) in the number of ablations (18 549), and the mean number of procedures per center was 181.9 ± 137.0 (higher than in 2018: 165.5 ± 127.9), with a median of 144.5 (range, 4-570). Seventeen centers (15 public) reported more than 300 ablations and 10 (8 public) reported more than 400 (figure 3).
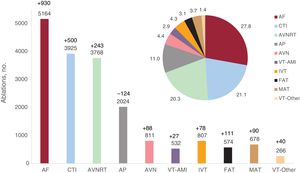
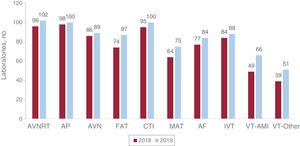
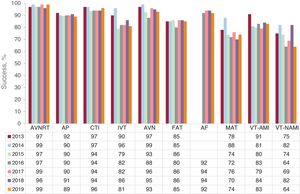
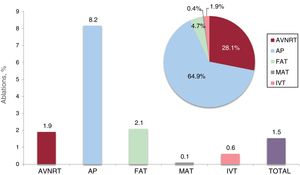
Regarding the different ablation targets (figure 4), AF was consolidated as the most frequently targeted substrate (5164; 27.8%), with more than 1200 procedures more than the next most common target, the CTI (21.1%). This moved AVNRT to third place (20.3%), with accessory pathways once again in fourth place (11%). Compared with 2018, the number of ablations of all substrates increased, except accessory pathways (figure 4). The changes in the relative frequencies of the different ablation targets since 2009 are shown in figure 5. The number of substrates treated by each laboratory increased in 2019 (figure 6). All centers (102) performed AVNRT ablation in 2019, 101 (99%) performed accessory pathway ablation, and 100 (98%) performed CTI ablation. The substrate targeted by the highest number of new centers was FAT (74 centers in 2018 and 87 in 2019). Finally, there was once again an increase in the number of centers treating AF (84%), which was stable (at about 75%) in the previous 3 years. The overall success rate was 91%, identical to that of 2018, although there were slight falls for several ablation targets, as can be seen in figure 7 (AF success data have only been collected since 2016, when the data collection form was updated).
Absolute frequency (bars) and relative frequency (pie chart) of the different ablation targets treated by catheter ablation in Spain in 2019 (18 549 procedures). The change in the number of cases vs the previous registry is also shown for each ablation target. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia/atypical atrial flutter; VT-AMI, ventricular tachycardia associated with acute myocardial infarction; VT-Other, other substrates.
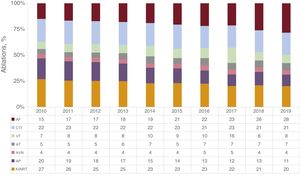
Changes in the relative frequency of the different ablation targets treated in the last 10 years. AF, atrial fibrillation; AP, accessory pathway; AT, atrial tachycardia (focal and atypical flutter); AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; VT, ventricular tachycardia.
Number of electrophysiology laboratories participating in the registry and treating each of the different ablation targets. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia; VT-AMI, ventricular tachycardia associated with acute myocardial infarction; VT-Other, other substrates.
Changes in catheter ablation success rates since 2013 by the arrhythmia or arrhythmogenic substrate treated. AF, atrial fibrillation; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; AP, accessory pathway; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia/atypical atrial flutter; VT-AMI, ventricular tachycardia associated with acute myocardial infarction; VT-NAMI, ventricular tachycardia not associated with acute myocardial infarction.
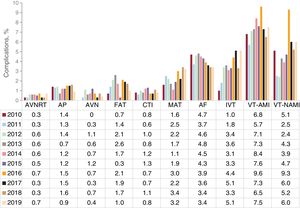
The changes in complications according to ablation target in the last 10 years are shown in figure 8. There were 348 complications (1.9%), a slight fall vs the previous 2 years. The most common complications continued to be vascular, followed by pericardial effusion/tamponade. Atrioventricular block (AVB) occurred in 25 patients.
Changes in the percentage of major complications related to catheter ablation since 2010 by the arrhythmia or arrhythmogenic substrate treated. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia; VT-AMI, ventricular tachycardia associated with acute myocardial infarction; VT-NAMI, ventricular tachycardia not associated with acute myocardial infarction.
Six periprocedural deaths were reported (0.03%); 3 of these deaths were related to VT ablations, whereas the other 3 were associated with left atrial procedures (2 in AF and 1 in MAT) and are described in the corresponding sections.
The following sections summarize the data analysis for the different ablation targets.
Atrioventricular nodal reentrant tachycardiaAVNRT was the only substrate treated in all participating centers. The slight increase in the absolute number of procedures (3768; 243 more than in the previous year) was not reflected in the relative percentage, which slightly decreased again (20% of all ablations). The mean number of procedures was 36.9 ± 24.5 (range, 2-130) and the success rate was 99%. In addition, 47% of centers reported a 100% success rate.
The 4-mm radiofrequency ablation catheter tip was once again the most commonly used catheter (94%). Although the application of other catheters and energy sources was low, cryoablation use increased this year, to second place (2.5%), largely due to a center that performed 73% of its procedures with this energy source. Other catheters were rare. Notably, the use is consistently increasing of navigation systems to avoid fluoroscopy (25% of procedures vs 10.9% in 2018) and 82.1% of these procedures were entirely performed without fluoroscopy.
In total, 26 severe complications were reported (0.7%): 12 AVBs (1 transient), 11 vascular complications, 1 heart failure event, and 1 embolic phenomenon.
Cavotricuspid isthmusCTI ablation, with 3925 procedures (21%), was once again the second most commonly targeted substrate after AF, ahead of AVNRT. It was treated in 100 centers, with a mean of 39.2 (range, 4-117) procedures per center and a mean success rate of 96%. Conventional irrigated tip catheters remained the most frequently used catheters (1842 procedures; 46.9%), although irrigated catheters with contact forcesensing technology have tripled since 2018 (932; 23.7%). The use of 8-mm catheters was stable (973; 24.8%). Navigation system use slightly increased, with 1272 procedures (32.4%), as did zero-fluoroscopy interventions, with 678 (17.2%). A total of 30 major nonfatal complications (0.8%) were reported: 23 vascular complications (0.6%), 3 pericardial effusions, 1 AVB, 1 embolism, and 1 myocardial infarction.
Accessory pathwaysAccessory pathways remain the fourth most targeted substrate. There was a slight decrease in the absolute number of procedures in 2019 (124 fewer): 2024 procedures for a total of 1904 accessory pathways, treated in 101 centers (3 more than in the previous year). An average of 20.1 ± 15.5 (range, 1-65) procedures was performed per center. A success rate of 89% was obtained, with 31 centers reporting 100% success.
The left ventricular free wall was once again the most frequent location (51.7%), with a 94% success rate, followed by inferoseptal (28.1%), with a 98% success rate. Para-Hisian/anteroseptal and right ventricular free wall had identical frequencies (10%) and similar success rates (84% and 85%, respectively).
Epicardial access was used for 31 accessory pathway procedures while the retroaortic approach was still the most commonly used approach for the ablation of left-sided pathways (66%).
The ablation rates of bidirectional conduction and exclusively antegrade conduction were similar (41.4% and 39.5%). Most of these ablations (54%) were performed with 4-mm ablation catheters. The use of irrigated catheters continued to increase (33.5%), although only 7.1% had contact forcesensing technology. Cryoablation was used in 4.9%, whereas the use of 8-mm catheters was limited (just 14 procedures).
There was major growth in the use of navigation systems in 2019, with an increase from 21.5% in 2018 to 44.5% in 2019. However, in contrast to the situation for AVNRT treatment, zero-fluoroscopy treatment of patients did not exceed 23% (10.2% of all accessory pathway ablations).
Complications markedly fell in 2019 (to half that of 2018). In total, 18 major complications were reported (0.9%): 8 vascular, 5 AVBs (1 transient), 2 pericardial effusions, 1 acute myocardial infarction, 1 embolism, and 1 transient bradycardia and hypotension.
Atrioventricular node ablationThe number of procedures targeting this substrate remained stable, with 811 ablations (4%) performed in 89 centers and a 93% success rate. Three minor complications were reported (0.3%), all vascular. Most of the procedures were performed with conventional 4-mm catheters (465; 57.3%), with the following distribution of the remainder: 209 conventional irrigated catheters (25.7%), 165 8-mm catheters (20.3%), and 17 irrigated contact forcesensing catheters (2.1%).
Focal atrial tachycardiaIn total, 574 procedures (3%) were performed in 87 centers, with a success rate of 85%, similar to that of 2018. This ablation target was located in the right atrium in 370 procedures (with a 90.5% success rate) and in the left atrium in 204 (a 74.1% success rate). Six complications were reported (1%), including 2 vascular complications (0.3%), 2 pericardial effusions (0.3%), and 1 transient phrenic nerve palsy. The use of irrigated tip catheters fell to 197 procedures (34.3%) and there was a marked increase in the use of catheters with contact forcesensing technology (218; 37.9%). Navigation system use clearly increased to 367 procedures (63.9%); 78 of these (13.5% of the total) were entirely performed without fluoroscopy.
Macroreentrant atrial tachycardiaMAT (which includes atypical atrial flutter) is one of the least treated ablation targets, with a total of 678 procedures (4%) in 75 centers. Of the 475 cases reporting this etiology, most (244; 51.3%) occurred after a previous AF ablation, 96 (20.2%) in congenital heart disease, and 79 (16.6%) after atriotomy; the remainder had various causes. It has the lowest success rate of all procedures—74.4%—and navigation system use is slowly increasing and now represents 81.7% of procedures. Just 35 procedures (5.1%) were performed without fluoroscopy. Irrigated tip catheters with contact forcesensing technology (67.4%) were much more frequently used than conventional irrigated tip catheters (14.3%); the other types were rarely used. A total of 22 nonfatal complications (3.2%) were reported, including 10 femoral vascular complications, 6 pericardial effusions, and 2 AVBs.
Atrial fibrillationAF was consolidated as the most often treated ablation target, with 5164 procedures in 4771 patients (26% of all ablations). This ablation target was treated by 7 new centers, giving a total of 84. The average number of procedures per center exceeded 50 ablations for the first time (mean, 61.5; range, 1-230), with a success rate of 92.3%. Nineteen centers performed more than 100 procedures (22.6%), with 2 performing more than 200 per year. According to the available data (4604 ablations), the distribution by type was 2886 paroxysmal AF procedures (62.7%), 1486 persistent AF procedures (32.3%), and 232 long-standing persistent AF procedures (5%).
Electrical isolation of the pulmonary veins was once again the most common procedure (91%). In addition, there were 37 reductions of the antral electrogram, 50 complex unfractionated electrogram ablations, and 116 superior vena cava isolations. Left atrial lines were placed in 193 procedures. Other targets included 24 magnetic resonance-guided scar ablations in 2 centers and 22 rotor ablations in 2 others. Also reported were ablation of the ganglion plexus and of extrapulmonary foci and a left atrial posterior box isolation.
The most commonly used technique for AF ablation was still point-by-point radiofrequency ablation, with 2925 procedures (57%); there was no increase in cryoablation, but it was consolidated as an alternative (2144; 42%). The use of other techniques was rare, such as the multielectrode pulmonary vein ablation catheter (PVAC) and laser ablation.
Irrigated catheters with contact forcesensing technology predominate (84.8% of point-by-point ablations). The use of steerable sheaths moderately increased to 1510 procedures (29.2% of the total, limited to 40 centers). Intracardiac echocardiography was still rarely used (445 procedures; 8.6%) and applied in just 15 centers. Three-dimensional navigation was used for 2938 procedures, and 5 centers reported zero-fluoroscopy procedures (115).
The number of complications was stable (178; 3.4%). Two were fatal (an atrioesophageal fistula and an atrial appendage perforation). The distribution of the remainder was as follows: 63 vascular complications (1.2%), 44 pericardial effusions (0.8%), 34 phrenic nerve palsies (0.6%), 14 embolisms (0.2%), 6 infarctions (0.1%), 3 perforations (0.06%, 1 requiring surgery), and 14 miscellaneous complications (eg, pericarditis, transient neurological symptoms, pulmonary embolism).
Idiopathic ventricular tachycardiaIn total, 807 IVT ablation procedures (4%) were performed in 762 patients in 88 centers (4 more than in 2018). The mean number of procedures per center was 9.2 ± 8 (range, 1-46).
The following procedure locations were reported: 354 tachycardias of the right ventricular outflow tract, 155 of the left ventricular outflow tract, 71 aortic root tachycardias, 40 fascicular tachycardias, 36 epicardial tachycardias, 3 pulmonary artery tachycardias, and 63 tachycardias distributed in different locations, including 13 in the papillary muscles, 4 in the summit of the left ventricle, and 6 para-Hisian.
The overall success rate was 81.4%. The highest success rates were seen for the pulmonary artery (100%), aortic cusps (94%), and right ventricular outflow tract (91%). Left ventricular outflow tract and fascicular tachycardias had slightly lower success rates (83% and 82.5%, respectively), with even lower rates for the mixed group (76%). The worst results were seen for epicardial/coronary sinus procedures (53%).
Irrigated catheters with contact forcesensing technology predominated (62%), which, in conjunction with conventional irrigated catheters, were used in 85.4% of procedures. Almost all of the other procedures were performed with 4-mm catheters.
In 2019, the use of navigation systems reached 78%, with fluoroscopy-free procedures uncommon (7%).
Complications markedly increased (5%; 40 cases), mainly vascular complications and pericardial effusions: 13 vascular complications, 21 effusions/tamponades, 1 pericarditis, 4 AVBs, and 1 unspecified complication.
Ventricular tachycardia associated with myocardial infarctionThis substrate was targeted by the highest number of new centers (17 more than in 2018). However, the absolute number of procedures stabilized (532 ablations in 497 patients). A mean of 8.3 ± 7.4 (range, 1-43) procedures was performed per center.
The overall success rate has continued its progressive increase, reaching 85%, which is the highest rate in registry history. The approach in 70% of the procedures was ablation of the arrhythmogenic substrate.
An endocardial approach once again predominated (82.6%), both retroaortic and transseptal (302 vs 282 procedures). The use of the combined approach continues to increase, reaching a new peak this year (17.4%, much higher than the 11.2% of 2018). This tendency was not followed by the exclusively epicardial approach, which was stable but uncommon (2.4%).
The use of navigation systems predominates (91.2%, a large increase vs the 84% of 2018), although only 2 procedures were fluoroscopy-free. Steerable sheaths were common (44.2%) and practically all procedures were performed with irrigated tip catheters (96.7%), most with contact force sensing technology (76.5%)
There was a slight increase in complications (40; 7.5%): 20 vascular complications (3.8%), 1 AVB (0.2%), 8 pericardial effusions (1.5%), 7 heart failure events (1.3%), 1 AMI, 1 colonic perforation during the epicardial approach, 1 subsequent amputation of a lower limb due to critical ischemia, and 1 postprocedural arrhythmic storm. In addition, 1 death (0.2%) was reported, caused by cardiogenic shock several days after the intervention.
Ventricular tachycardia not associated with myocardial infarctionIn total, 266 ablation procedures were performed in 247 patients in 51 centers (12 hospitals more than in 2018). Regardless, it continues to be the least addressed ablation target in both absolute numbers (1.5% of procedures) and the number of centers (only half of registry laboratories), with an average of 5.2 ± 5.5 (range, 1-30) procedures.
With an 80% success rate, the following ablation targets were reported: 155 in nonischemic dilated cardiomyopathy (77% successful), 40 in arrhythmogenic cardiomyopathy (90% successful), 26 in congenital heart diseases (100% successful), 9 in hypertrophic cardiomyopathy (78% successful), 9 bundle branch ventricular tachycardias (89% successful), and 24 miscellaneous cases (92% successful), including 7 in valvular heart disease, 5 in myocarditis, 2 in Chagas disease, and 1 in incessant ventricular fibrillation.
The endocardial approach continues to predominate, with a slight preference for the retroaortic over the transseptal (36% vs 29%). However, exclusively epicardial approaches doubled vs 2018 (10.5%) and there was another increase in the combined approach (27.4%). The vast majority of catheters were irrigated tip catheters (95%), typically with contact forcesensing technology (73%).
As for other VTs, navigation systems are invaluable and their use has increased vs previous years (90.6% vs 81.4% in 2018). Fluoroscopy-free procedures continue to be rare (8 procedures).
There were 15 complications (5.6%): 4 vascular (1.5%), 3 effusions/tamponades (1.1%), 2 AVBs (0.7%), 1 embolic phenomenon (0.3%), 1 AMI (0.3%), 3 heart failure events (1.1%), and 1 myocardial laceration. In addition, there was 1 death due to cardiogenic shock, which occurred several hours after incessant ventricular fibrillation ablation, and 1 death in a patient with previous cardiogenic shock receiving mechanical circulatory support and with arrhythmic storm.
Zero-fluoroscopy ablationNonfluoroscopic navigation was used in 8336 procedures (44.9%). Such systems were most commonly used for VTs (90.9%) and MATs (81.7%). For the last few years, the registry has collected data on zero-fluoroscopy procedures. As in previous years, the number of zero-fluoroscopy procedures in 2019 doubled that of 2018, reaching 1967 procedures (11% of the total). For the first time, the ablation target most commonly treated without fluoroscopy was AVNRT (768 procedures, 20.4% of all AVNRT ablations), followed by CTI (678 procedures, 17.3% of all CTI procedures).
Ablations in pediatric patientsThe number of centers and procedures in pediatric patients fell in 2019. In total, 286 ablation procedures (1.5%) were performed in 39 centers (7 fewer than in 2018).
The most frequently treated substrate was once again the accessory pathways (figure 9) (58% of all pediatric ablations and 8.2% of all accessory pathway ablations) but in a lower proportion than in 2018 (70.5% and 11.6%, respectively).
Pediatric ablation procedures. The bar chart shows the proportion of pediatric procedures for each ablation target and the total number of procedures in the registry while the pie chart shows the proportion of each substrate ablated with respect to the total number of pediatric procedures. AP, accessory pathway; AVNRT, atrioventricular nodal reentrant tachycardia; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia.
The other reported ablations in pediatric patients were 72 AVNRTs, 1 MAT, 12 FATs, and 5 IVTs. Overall, they represented 8.2% of accessory pathways, 1.9% of AVNRTs, 0.1% of atypical flutters, 2.1% of FATs, and 0.6% of IVTs. No CTI ablations were reported in 2019.
DISCUSSIONThe Spanish Catheter Ablation Registry, for the 19th consecutive year, continues to systematically record the ablation procedures performed in Spain. Its uninterrupted and comprehensive character, elevated participation, and the consistency of its data make it the only such registry of its kind worldwide. Barely no other similar experiences have been published, because the few national electrophysiology societies to publish data have described only activity (Portuguese20 and Italian21 registries), without detailing success rates or complications, or were limited to specific arrhythmias, such as the German registry.22,23 The Swedish Catheter Ablation Registry24 has recently provided complete and comprehensive information on most procedures from a 10-year period (2006-2015), although some substrates were missing, such as macroreentrant tachycardias, and the different VT forms were not differentiated, as in ours. Finally, the Japanese registry is planning to include patients in a similar registry to ours, although it is still in the pipeline.25
Our registry is a privileged platform to learn about the current use of catheter ablation therapy for cardiac arrhythmias. This information is essential to modify the improvement criteria for each center, among other objectives. The number of participating centers and procedures (18 549) reached a new high in 2019. It is likely that these numbers will not be surpassed until 2021 due to the marked fall in activity related to the coronavirus disease 2019 (COVID-19) pandemic, caused by SARS-CoV-2, which limited activity to urgent procedures for more than 2 months.26
The increase in procedures per center has been more uniform than in other years, in terms of both the mean and the median.
The growth in AF ablation increased its distance from the other ablation targets and highlights the lack of an increase in pulmonary vein cryoablation, the first in recent years; this technique fell to 42% of procedures from 44% in 2018. These results have probably been influenced by the predominant use of irrigated tip catheters with contact forcesensing technology as the catheter of choice for pulmonary vein ablation (84.8% of point-by-point ablations). In fact, catheters with contact forcesensing information have become the most frequently used catheters not only in AF, but also in the other complex substrates (MAT and all VTs).
All ablation targets showed an increased number of procedures in 2019, although not so markedly. The only exception was the accessory pathways, with a fall in the number of procedures to 114.
The success, complication, and mortality rates have barely changed from previous registries. AF continues to be the substrate with the highest number of complications, although the most severe complications are seen with VA-AMI (7.5%) and VT-NAMI (5.6%). This situation is also a reflection of the more severe conditions of the patients when these ablation procedures are indicated and the greater complexity of the procedures.
There were 6 periprocedural deaths (the same number as in the previous year), related to complex substrates, AF, MAT, and VT, and, in the case of these targets, to very high-risk patients, although we should remember that all procedures can become complicated and should not be underestimated.
Navigation systems continue their unstoppable rise in both complex targets and in more simple substrates, such as AVNRT. In AF, their rate of use is almost identical to the 99% of ablations performed with radiofrequency and exceeds the 90% of VT ablations in patients with heart disease. These navigation systems permit further progress toward the “zero-fluoroscopy” objective, which is particularly relevant given their confirmed safety and efficacy.27 The number of fluoroscopy-free procedures performed in 2019 doubled that of 2018. This approach was used in 11% of all procedures reported to the current registry. AVNRT is a representative example of this trend, because this ablation target was managed without fluoroscopy in three-quarters of the procedures performed with a navigation system.
Finally, the number of pediatric ablation procedures fell slightly, as well as the number of centers performing these interventions (7 fewer than in 2018). This suggests that the likely most suitable situation,28 the concentration of these procedures in selected centers,29 may have already begun. We highlighted the value of this strategy in the previous registry report.18
CONCLUSIONSThe Spanish Catheter Ablation Registry continues to be the only such registry of its kind, due to its regularity, exhaustive nature, and the quality and relevance of its data. The number of overall procedures, except those in accessory pathways, and AF ablation procedures in particular reached a historic peak in 2019, with a continued highly elevated success rate and low rates of complications. Once again, the number of participating centers increased vs the previous year, which strengthens our conviction that the registry continues to reflect current Spanish ablation activity.
CONFLICTS OF INTERESTNone.
The coordinators of the registry would once again like to thank all of the participants in the Spanish Catheter Ablation Registry for voluntarily and selflessly completing the lengthy data collection forms. We again thank Cristina Plaza for her excellent and indispensable work, which goes above and beyond administration.
Jesús Almendral-Garrote, Pau Alonso-Fernández, Concepción Alonso-Martín, Nelson María Alvarenga-Recalde, Luis Álvarez-Acosta, Miguel Álvarez-López, Ignasi Anguera-Camos, María Fe Arcocha-Torres, Miguel Ángel Arias-Palomares, Antonio Asso-Abadía, Alberto Barrera-Cordero, Juan Benezet-Mazuecos, Andrés I. Bodegas-Cañas, Josep Brugada-Terradellas, Claudia Cabadés-Rumbeu, María del Pilar Cabanas-Grandío, Lucas R. Cano-Calabria, Silvia del Castillo-Arrojo, Víctor Castro-Urda, Rocío Cózar-León, Ernesto Díaz-Infante, Juan Manuel Durán-Guerrero, Juliana Elices-Teja, Elena Esteban-Paul, María del Carmen Expósito-Pineda, Juan Manuel Fernández-Gómez, Julio Jesús Ferrer-Hita, María Luisa Fidalgo-Andrés, Adolfo Fontenla-Cerezuela, Arcadio García-Alberola, J. Ignacio García-Bolao, Enrique García-Cuenca, Francisco Javier García-Fernández, Ignacio Gil-Ortega, Federico Gómez-Pulido, Juan José González Ferrer, Eduard Guasch i Casany, José M. Guerra-Ramos, Santiago Heras-Herreros, Julio Hernández-Afonso, Benito Herreros-Guilarte, Víctor Manuel Hidalgo-Olivares, Alicia Ibáñez-Criado, José Luis Ibáñez-Criado, Sonia Ibars-Campaña, Miguel Eduardo Jáuregui-Abularach, F. Javier Jiménez-Candil, Javier Jiménez-Díaz, Jesús I. Jiménez-López, Carla Lázaro-Rivera, José Miguel Lozano-Herrera, Alfonso Macías-Gallego, Santiago Magnani-Ragamato, Javier Martínez-Basterra, Ángel Martínez-Brotons, José Luis Martínez-Sande, Gabriel Martín-Sánchez, Roberto Matías-Francés, María Matiello, Francisco Mazuelos, Elena Mejía, José Luis Merino-Llorens, Josep Lluis Mont-Girbau, José Moreno-Arribas, Javier Moreno-Planas, Pablo Moriña-Vázquez Ángel Moya-i-Mitjans, Josep Navarro-Manchón, Joaquín Osca-Asensi, Agustín Pastor-Fuentes, Ricardo Pavón-Jiménez, Rafael Peinado-Peinado, Alonso Pedrote, Luisa Pérez-Álvarez, Nicasio Pérez-Castellano, Andreu Porta-Sánchez, Jordi Punti-Sala, Aurelio Quesada-Dorador, Nuria Rivas-Gándara, Felipe José Rodríguez-Entem, Enrique Rodríguez-Font, Juan Carlos Rodríguez-Pérez, Rafael Romero-Garrido, José Manuel Rubín-López, José Manuel Rubio-Campal, Jerónimo Rubio-Sanz, José Ramón Ruiz Arroyo, Pablo M. Ruiz-Hernández, Ricardo Salgado-Aranda, Georgia Sarquella-Brugada, Axel Sarrias-Mercé, Jose María Segura-Saint-Gerons, Federico Segura-Villalobos, and Irene Valverde-André.
| Andalusia | |
| Cádiz | Hospital Universitario Puerta del Mar (Lucas R. Cano-Calabria) |
| Granada | Hospital Universitario Virgen de las Nieves (Miguel Álvarez-López); Hospital HLA Inmaculada (Miguel Álvarez-López); Hospital Clínico Universitario San Cecilio (José Miguel Lozano-Herrera) |
| Huelva | Hospital Juan Ramón Jiménez (Pablo Moriña Vázquez); Hospital Quirón Huelva (Pablo Moriña Vázquez) |
| Córdoba | Hospital Universitario Reina Sofía (Jose María Segura-Saint-Gerons/Francisco Mazuelos) |
| Málaga | Hospital Clínico Universitario Virgen de la Victoria, Hospital Vithas Xanit Internacional, Hospital Vithas Parque San Antonio, Hospital Quirónsalud Málaga, Hospital Quirónsalud Marbella (Alberto Barrera-Cordero) |
| Sevilla | Hospital Universitario Virgen Macarena (Rocío Cózar-León); Hospital Vithas Nisa Sevilla (Ernesto Díaz-Infante); Hospital Universitario Virgen del Rocío (Alonso Pedrote); Hospital Universitario Virgen de Valme (Ricardo Pavón-Jiménez); Hospital Quirónsalud Infanta Luisa, Hospital Quirónsalud Sagrado Corazón (Juan Manuel Fernández-Gómez); Hospital HLA Santa Isabel (Rafael Romero-Garrido) |
| Aragon | |
| Zaragoza | Hospital Universitario Miguel Servet, Hospital Quirónsalud Zaragoza (Antonio Asso-Abadía); Hospital Clínico Universitario Lozano Blesa (José Ramón Ruiz Arroyo) |
| Principality of Asturias | Hospital Universitario de Cabueñes (Irene Valverde-André); Hospital Universitario Central de Asturias (José Manuel Rubín-López) |
| Balearic Islands | Hospital Universitario Son Llátzer (Santiago Magnani-Ragamato); Hospital Universitario Son Espases (María del Carmen Expósito-Pineda); Clínica Rotger, Hospital Quirónsalud Palmaplanas (Nelson María Alvarenga-Recalde) |
| Canary Islands | |
| Las Palmas | Hospital Vithas Santa Catalina (Juan Carlos Rodríguez-Pérez); Hospital Perpetuo Socorro (Pablo M. Ruiz-Hernández); Hospital Universitario Insular de Gran Canaria (Federico Segura-Villalobos) |
| Santa Cruz de Tenerife | Hospital Universitario Nuestra Señora de la Candelaria (Luis Álvarez-Acosta); Hospital San Juan de Dios (Julio Hernández-Afonso); Complejo Hospitalario Universitario de Canarias (Julio Jesús Ferrer-Hita) |
| Cantabria | Hospital Universitario Marqués de Valdecilla (Felipe José Rodríguez Entem) |
| Castile-La Mancha | |
| Toledo | Hospital Virgen de la Salud (Miguel Ángel Arias-Palomares); Hospital General Nuestra Señora del Prado (Alfonso Macías-Gallego) |
| Ciudad Real | Hospital General Universitario de Ciudad Real (Javier Jiménez-Díaz) |
| Albacete | Complejo Hospitalario Universitario de Albacete (Víctor Manuel Hidalgo-Olivares) |
| Castile and León | |
| Burgos | Hospital Universitario de Burgos (Javier García Fernández) |
| León | Complejo Asistencial Universitario de León (María Luisa Fidalgo-Andrés) |
| Salamanca | Complejo Asistencial Universitario de Salamanca (F. Javier Jiménez-Candil) |
| Valladolid | Hospital Clínico Universitario de Valladolid (Jerónimo Rubio-Sanz); Hospital del Río Hortega (Benito Herreros-Guilarte) |
| Catalonia | |
| Barcelona | Hospital Universitario de Bellvitge (Ignasi Anguera-Camos); Hospital Clínic (Josep Lluis Mont-Girbau, Eduard Guasch-i-Casany); Hospital Universitario Germans Trias i Pujol (Axel Sarrias-Mercé); Hospital Universitario Vall d’Hebron (Nuria Rivas-Gándara); Clínica Corachán (José M. Guerra-Ramos); Clínica Sagrada Família, Hospital Universitario Dexeus (Ángel Moya-i-Mitjans); Hospital Universitario Mútua de Terrassa (Sonia Ibars-Campaña); Hospital Sant Joan de Déu (Georgia Sarquella-Brugada); Hospital del Mar (Jesús I. Jiménez-López); Hospital Universitario Parc Taulí (Jordi Punti-Sala); Hospital de la Santa Creu i Sant Pau (Concepción Alonso-Martín); Clínica Teknon (Enrique Rodríguez Font); Hospital General de Cataluña (María Matiello) |
| Tarragona | Hospital Universitario Joan XXIII (Gabriel Martín Sánchez) |
| Lleida | Hospital Universitario Arnau de Vilanova (Miguel Eduardo Jáuregui-Abularach) |
| Girona | Clínica Girona (Josep Brugada-Terradellas) |
| Valencian Community | |
| Alicante | Hospital Universitario San Juan de Alicante (José Moreno-Arribas); Hospital General Universitario de Alicante (José Luis Ibáñez-Criado); Cardioritmo Levante (Alicia Ibáñez-Criado) |
| Castellón | Hospital General Universitario de Castellón (Josep Navarro Manchón) |
| Valencia | Hospital General Universitario de Valencia (Aurelio Quesada-Dorador); Hospital Universitario y Politécnico de La Fe (Joaquín Osca-Asensi); Hospital Clínico Universitario de Valencia (Ángel Martínez-Brotons); Hospital de Manises (Pau Alonso-Fernández); Hospital Universitario de la Ribera (Santiago Heras-Herreros); Hospital Universitario Dr. Peset (Claudia Cabadés-Rumbeu) |
| Extremadura | |
| Badajoz | Hospital Universitario de Badajoz (Juan Manuel Durán-Guerrero) |
| Galicia | |
| A Coruña | Hospital Universitario de A Coruña (Luisa Pérez-Álvarez); Complexo Hospitalario Universitario Clínico de Santiago de Compostela (José Luis Martínez-Sande) |
| Pontevedra | Hospital Álvaro Cunqueiro (María del Pilar Cabanas-Grandío) |
| Lugo | Hospital Universitario Lucus Augusti (Juliana Elices-Teja) |
| Community of Madrid | Hospital Universitario Ramón y Cajal (Javier Moreno-Planas), Hospital Universitario La Moraleja (Roberto Matías-Francés); Hospital Universitario 12 de Octubre (Adolfo Fontenla-Cerezuela); Hospital Universitario de Getafe (Agustín Pastor-Fuentes); HM Hospitales (Jesús Almendral-Garrote); Hospital Universitario Puerta de Hierro (Víctor Castro-Urda); Hospital Universitario La Paz (Rafael Peinado-Peinado); Hospital Universitario Quirónsalud Madrid y Complejo Hospitalario Ruber Juan Bravo (Andreu Porta-Sánchez, José Luis Merino-Llorens); Hospital Universitario La Paz-Unidad de Electrofisiología Robotizada, Hospital Nisa Pardo de Aravaca (José Luis Merino-Llorens); Hospital Clínico San Carlos (Nicasio Pérez Castellano); Hospital Universitario Fundación Alcorcón (Elena Esteban-Paul); Hospital Universitario Fundación Jiménez Díaz (José Manuel Rubio-Campal); Hospital Universitario Severo Ochoa (Ricardo Salgado-Aranda); Hospital La Luz-Quirón (Juan Benezet Mazuecos); Hospital Universitario Rey Juan Carlos (Federico Gómez-Pulido/Elena Mejía); Hospital Universitario de Torrejón (Carla Lázaro-Rivera); Hospital Universitario de Fuenlabrada (Silvia del Castillo-Arrojo). Hospital Universitario Príncipe de Asturias (Juan José González Ferrer) |
| Region of Murcia | Hospital Universitario Virgen de la Arrixaca (Arcadio García-Alberola); Hospital General Universitario Santa Lucía (Ignacio Gil-Ortega) |
| Chartered Community of Navarre | Complejo Hospitalario de Navarra (Javier Martínez-Basterra); Clínica Universidad de Navarra (J. Ignacio García-Bolao) |
| Basque Country | |
| Vizcaya | Hospital de Cruces (Andrés I. Bodegas-Cañas); Hospital de Basurto (María Fe Arcocha-Torres) |
| Álava | Hospital Universitario Araba (Enrique García-Cuenca) |
| LaRioja | Hospital Viamed Los Manzanos (Francisco Javier García-Fernández) |