The results of the 2021 Spanish catheter ablation registry are presented.
MethodsData collection was carried out retrospectively by filling in and sending a specific form by the participating centers.
ResultsData from 93 centers (65 public, 28 private) were analyzed. A total of 17941 ablation procedures were reported with a mean of 193 ± 133 cases per centre. Recovery of activity from SARS-CoV-2 pandemic lockdown has led to a notable increase in the number of procedures (+2772 procedures, +18%) despite a small decrease in participating centers (4 centers less than in 2020). Atrial fibrillation ablation continues to be the leading procedure, with 5848 procedures (32,6%). Together with ablation of the cavotricuspid isthmus (3766; 21%) and atrioventricular nodal reentrant tachycardia (3132; 17,5%) they constitute the 3 most frequently approached substrates. The total success rate reported (94%) is similar to previous years with a similar rate of complications (2%) and mortality (0.07). A total of 401 procedures were performed in pediatric patients (3,8%).
ConclusionsThe Spanish catheter ablation registry systematically and continuously collects the national activity, which has recovered significantly from the SARS-CoV-2 pandemic impact in 2020. Success rate for 2021 remains high, with a low complication rate.
Keywords
For 2 decades and without interruption, the Spanish catheter ablation registry, an official report of the Heart Rhythm Association of the Spanish Society of Cardiology, has described the changes over time in the interventional management of arrhythmias in Spain.1–20 Its objective is to provide reliable and comparable data on the activity and resources of Spanish arrhythmia units.
METHODSData were retrospectively collected using a standardized form sent to all electrophysiology laboratories at the start of 2022. Data submission is voluntary and anonymous, even to the registry coordinators, because the secretary of the Spanish Society of Cardiology removes center identifiers.
The registry provides data on the technical and human resources of the participating arrhythmia units and the types of procedures and ablation targets, as well as their outcomes and complications. In line with the categorization established in previous years, the arrhythmias and arrhythmogenic substrates were analyzed in the following categories: atrioventricular nodal re-entrant tachycardia (AVNRT), accessory pathways (APs), atrioventricular node (AVN), focal atrial tachycardia (FAT), cavotricuspid isthmus (CTI), macrore-entrant atrial tachycardia (MAT), atrial fibrillation (AF), idiopathic ventricular tachycardia (IVT), ventricular tachycardia (VT) associated with myocardial infarction (VT-AMI), and VT not associated with myocardial infarction (VT-NAMI). For the first time, data were collected on cardioneuroablation.
The following variables common to all substrates were analyzed: numbers of patients and procedures (specifying the number of pediatric patients, defined as those younger than <15 years), acute success (at the end of the procedure), type of ablation catheter used, and numbers and types of complications, including periprocedural death. Also analyzed were a number of ablation target-specific variables, such as type, location, and underlying heart disease. The use of electroanatomic mapping systems was also recorded for all procedures, as well as those performed without the need for fluoroscopy. As in previous years, the success rate refers to acute success (at the end of the procedure) and the complications recorded are those occurring during the hospital stay. As in 2020, given the SARS-CoV-2 pandemic, additional information has been requested in an attempt to quantify the impact of the pandemic on the clinical practice in Spanish laboratories.
RESULTSTechnical and human resourcesTable 1 and table 2 show the technical and human resources in the participating laboratories, as well as their different activities. A total of 65 centers (69.9%) were equipped with at least 1 dedicated cardiac electrophysiology laboratory. Centers with more than 1 laboratory continued to be a minority: 18 centers (19.3%) had 2. The vast majority of centers also reported device implantation activity (pacemakers, defibrillators, resynchronization devices, and subcutaneous Holter). At least 1 fixed C-arm fluoroscopy system was available in 71 centers (76.3%) and 23 centers had rotational angiography. Most centers were equipped with a nonfluoroscopic navigation system. The most widespread was the Ensite system (73.1%), followed by Carto (61.2%) and Rhythmia (26.8%), and 75.2% performed cryoablation. The dedicated personnel in the electrophysiology laboratories was stable, with a mean of 3.3 physicians (just 2.4 full-time) and an average of 0.5 fellows per year.
Technical resources and additional activity of participating laboratories (n=93).
| General characteristics | |
| Teaching hospital | 73 (78.5) |
| Tertiary | 70 (75.2) |
| Type of funding | |
| Public | 64 (68.8) |
| Private | 26 (28) |
| Treating department: Cardiology | 91 (97.9) |
| Cardiac surgery available | 63 (67.7) |
| Anesthetist available | 81 (87.1) |
| Technical resources | |
| Availability of laboratory | |
| Exclusive use | 65 (69.9) |
| More than 1 electrophysiology laboratory | 18 (19.3) |
| Fluoroscopy system | |
| Fixed C-arm | 71 (76.3) |
| Portable C-arm | 28 (30.1) |
| Rotational angiography | 23 (24.7) |
| Nonfluoroscopic navigation systems | |
| Carto | 57 (61.2) |
| Ensite | 68 (73.1) |
| Rhythmia | 25 (26.8) |
| Remote navigation | |
| Magnetic | 1 (1) |
| Robotic | 1 (1) |
| Additional resources | |
| Intracardiac echocardiography | 43 (46.2) |
| Cryoablation | 70 (75.2) |
| Laser ablation | 1 (1) |
| Activity | |
| Device implantation | |
| Pacemakers | 86 (92.5) |
| ICDs | 84 (90.3) |
| Resynchronization devices | 83 (89.2) |
| Subcutaneous Holter | 87 (93.5) |
| Electrical cardioversion | 82 (88.2) |
| Renal denervation | 5 (5.3) |
| Atrial appendage closure | 20 (21.5) |
ICD, implantable cardioverter-defibrillator.
Data are expressed as No. (%).
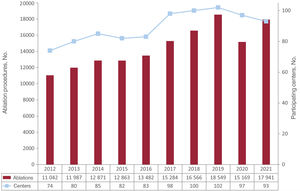
The total number of ablations performed increased in 2021, after the fall detected in 2020 (as a result of the impact of the SARS-CoV-2 pandemic). In contrast, there was another decrease in the number of participating centers (4 fewer than in 2020). In 2021, 17 941 ablation procedures were reported, with an average of 193 ± 133 procedures per center and a median of 171. The activity recovery after the SARS-CoV-2 pandemic-related shutdown led to a marked jump in procedures (+2772 procedures, +18%). Figure 1 shows the changes over time in the numbers of procedures and centers participating in the registry in the last 10 years.
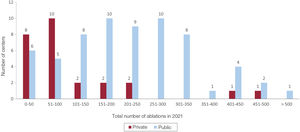
There was robust recovery in the number of centers performing more than 400 ablations (from 3 in 2020 to 9 in 2021), although there were 10 such centers in 2019. Figure 2 shows the number of procedures per center and the distribution of the centers by type of funding.
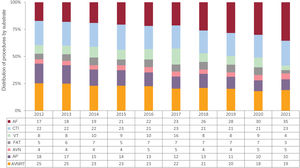
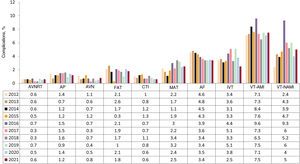
The data indicate an increase in the number of procedures of all ablation targets, and their relative distribution is similar to that of 2020. AF continued to be the most commonly treated ablation target, with almost one-third of procedures (5848 procedures; 32.6%). The second most frequently treated ablation target, CTI ablation, was stable (3766 procedures; 21%). AVNRT ablation was next (3132 procedures; 17.5%). Figure 3 shows the distribution of the number of procedures per ablation target in the last decade while table 3 details the relative proportion of ablation targets in 2021 and compared with 2020.
Distribution of the number of procedures by ablation target in the last decade. AF, atrial fibrillation; AP, accessory pathway; AT, atrial tachycardia; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; VT, ventricular tachycardia.
Overall and relative distributions of the number of procedures per ablation target reported in 2021 and compared with 2020.
| Procedures | 2020 | 2021 | Relative % in 2021 | % variation from 2020 |
|---|---|---|---|---|
| AF | 4513 | 5848 | 32.6 | +29.6 |
| CTI | 3188 | 3766 | 21 | +18.1 |
| AVNRT | 2808 | 3132 | 17.5 | +11.5 |
| AP | 1539 | 1645 | 9 | +6.9 |
| AVN | 750 | 905 | 5 | +20.7 |
| VT-AMI | 422 | 453 | 3 | +7.3 |
| IVT | 649 | 709 | 4 | +9.2 |
| FAT | 471 | 504 | 3 | +7.0 |
| MAT | 582 | 749 | 4 | +28.7 |
| VT-NAMI | 247 | 199 | 1 | −19.4 |
| Cardioneuroablation | 0 | 31 | 0 | 0 |
AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia; VT-AMI, ventricular tachycardia associated with acute myocardial infarction; VT-NAMI, ventricular tachycardia not associated with acute myocardial infarction.
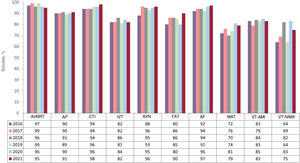
The success rate was similar to the average of recent years at 94% and the percentage of complications was stable at 2%. Figure 4 and figure 5 show the success rates and complications reported in recent years by ablation target.
Changes over time in success rate per ablation target. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia; VT-AMI, ventricular tachycardia associated with acute myocardial infarction; VT-NAMI, ventricular tachycardia not associated with acute myocardial infarction.
Changes over time in complication rate per ablation target. AF, atrial fibrillation; AP, accessory pathway; AVN, atrioventricular node; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia; VT-AMI, ventricular tachycardia associated with acute myocardial infarction; VT-NAMI, ventricular tachycardia not associated with acute myocardial infarction.
A total of 360 complications were reported. The most frequent continued to be vascular complications (n=110) and pericardial effusions/tamponades (n=98). There were 14 atrioventricular blocks (half in AVNRT and the rest during CTI or VT ablation). Regarding mortality, 14 periprocedural deaths were recorded (0.07%), which was similar to the number in previous years.
The following sections summarize the different ablation targets.
Atrioventricular nodal re-entrant tachycardiaAVNRT ablation continued to be the third most frequently treated ablation target, after AF and CTI. A total of 3132 procedures were performed, representing an 11.5% increase vs 2020, although the relative percentage vs all other ablation targets was stable at 17.5%.
Together with CTI ablation, AVNRT continued to be the ablation target treated in the highest number of centers (n=93). The reported success rate was 95% and the complications rate was 0.6%, including 9 atrioventricular blocks (2 transient), 4 vascular complications, 1 pneumothorax, and 1 PR interval prolongation. A 4-mm nonirrigated tip catheter was used in most procedures (88%), whereas the use of other types of catheters or energy sources was negligible (cryoablation, 2%; irrigated tip catheter, 1.7%). The use of nonfluoroscopic navigation systems continued to grow and reached 55.7% of procedures for this ablation target (31% in 2020); 44% of procedures using a navigation system were performed without fluoroscopy.
Accessory pathwaysAP ablation was once again the fourth most frequent ablation target, with 9% of all ablations performed and a 6.9% increase in the total number of procedures vs 2020 (1645 vs 1539 in 2020). AP ablation was reported by 90 of the 93 participating centers, with a success rate of 91% and complication rate of 1.6%; these complications included 9 vascular complications, 8 pericardial effusions, 1 bilateral pulmonary thromboembolism 1 week after the procedure, 1 self-limiting Wenckebach atrioventricular block, and 1 catheter entrapment in the mitral subvalvular apparatus requiring surgery.
In addition, 46.5% of the APs showed bidirectional conduction, 17.8% had exclusively anterograde conduction, and 38.2% had exclusively retrograde conduction. Left APs continued to be the most frequent location (44.3% of procedures), with a 93.5% ablation success rate, followed by inferoseptal (24.5%; 99.8% reported success rate), right free wall pathways (9.4%; 89.7% success rate), and Para-Hisian/anteroseptal pathways (8.3%; 86% success rate). Epicardial ablation was necessary in 25 procedures, whereas retroaortic access was used for ablation of the left pathways in 71% of procedures. The use of navigation systems has become predominant, with a highly marked increase vs 2020 (70.8% in 2021 vs 48.7% in 2020), and 29.2% were performed without fluoroscopy.
Focal atrial tachycardiaFAT was the eighth most commonly treated ablation target in 2021, with a total of 504 procedures in 483 patients (3% of all ablations in 2021) and of 5.5 procedures annually per center. In 456 procedures (90%), the ablation was considered a success. In 352 procedures, the origin of the FAT was the right atrium (70%), with effective ablation in 327 (93%). In the remaining 152 procedures, the origin was the left atrium, with procedural success in 123 (81%). The application of a 4-mm nonirrigated catheter continued its downward trend, reaching its current infrequent use (20% of procedures), and there were 10 focal cryoablations and 377 irrigated catheter procedures (75% of the total), 103 without contact forcesensing technology and 274 with the technology. The use of navigation systems continued its upward trend. They were used in 73% of all ablations of this substrate (n=368). In 127 cases, the procedure was performed without fluoroscopy, an increase from 21% in 2020 to 25%. In 2021, a total of 9 complications (1.8%) related to this procedure were reported; 4 were vascular and 4 were atrioventricular blocks and there was 1 pericardial effusion.
Cavotricuspid isthmusIn 2021, 3766 CTI ablations were performed in 3646 patients; this ablation target was thus the second most frequent target, after pulmonary vein ablation (21% of all procedures). An average of 41 procedures was performed per center. The acute success rate (CTI block) was 98%. In 2734 of the 3766 procedures (73%), an irrigated tip catheter was used, with contact forcesensing technology in 1283 procedures and without this technology in 1481. In 885 procedures, an 8-mm catheter was used (23.5%, an almost identical percentage to that of 2020). After a marked increase in 2020, mapping system use stabilized and represented slightly less than half of all procedures (46%). Zero-fluoroscopy ablations fell slightly from 25% in 2020 to 20% in 2021 (749 of the 3766 procedures). In line with previous years, a total of 22 complications were recorded (0.6%); once again, those related to the vascular access predominated (n=16), as well as 2 cases of pericardial effusion and 1 myocardial infarction. Notably, there were no cases of atrioventricular block related to CTI ablation and no deaths.
Macrore-entrant atrial tachycardiaIn 2021, the number of ablations of this substrate was considerably higher, with a total of 749 procedures in 633 patients, vs 582 in 2020. In 594 procedures (79%), the ablation was considered successful. This percentage is similar to that of 2020 and significantly lower than that of other ablation targets. A total of 244 procedures (33%) were performed after previous AF ablation, 111 (15%) in patients with congenital heart disease and 62 in patients with previous arteriotomy. Of the 749 ablations of this substrate, 212 (29%) were in the right atrium and 510 (68%) were in the left atrium.
The use of nonirrigated catheters for this substrate was negligible, with absolute predominance of irrigated catheters with contact forcesensing technology (617 of all MAT ablations, 82%). The ablation was performed predominantly with a mapping system (628 procedures, 84%) and without fluoroscopy in 86 (11%). The procedure included administration of ethanol into the vein of Marshall in 16 procedures. A total of 19 complications were recorded (3%), which included 7 vascular complications, 8 pericardial effusions, and 1 embolism.
Atrioventricular node ablationIn total, 905 AVN ablations were performed in 854 patients, with an average of 10 ablations of this substrate per center. AVN was once again the fifth most commonly treated target, with 5% of all ablations in 2021. In addition, 96% of procedures were successful, a similar percentage to previous years. A 4-mm catheter continued to be the most frequently used catheter type (499 procedures, 55%), with irrigated catheters used in 304 procedures (without contact forcesensing technology in 250 of them). An 8-mm catheter was applied in 109 procedures (12%), with no decrease from previous years. A total of 7 complications were recorded (0.8%), including 3 vascular complications, 1 pericardial effusion, and 1 embolic event related to the procedure. A mapping system was used in 45 procedures (5%) and 65 (7%) were performed without fluoroscopy.
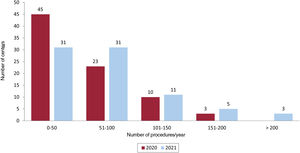
Atrial fibrillationAF ablation continued its growing predominance and was the most frequently treated ablation target in 2021. It represented 32.6% of all reported ablation procedures (5848 procedures in 5601 patients). According to the available data, 3516 of the 5848 procedures were performed in patients with paroxysmal AF, 1888 in patients with persistent AF, and 213 in patients with long-standing persistent AF. Once again, a not insignificant number of centers (n=13) performed no AF ablations, 31 centers performed fewer than 50, and 51 (54% of the total) performed most of the ablations of this substrate (more than 50 per center). In contrast, 8 centers performed more than 150 ablations. Figure 6 shows the number of centers by annual ablation volume (in blocks of 50 procedures).
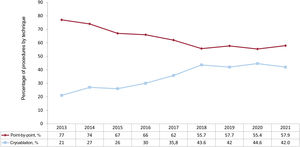
An irrigated catheter was used in 3286 procedures (56%), with contact forcesensing technology in 95% while cryoablation was used in 2399 (41%). Figure 7 shows the changes over time in point-by-point ablation and cryoablation of AF from 2013 to 2021. An additional 83 procedures were performed with laser. Steerable sheaths and intracardiac echocardiography continue to show continuous year-on-year growth and were used in 32% and 11% of procedures in 2021, respectively. In 2021, a seventh center performing fluoroscopy-free AF ablation was added, giving a total of 242 procedures (much higher than the 75 such procedures in 2020). The objective of the procedure was pulmonary vein isolation alone in 92% of cases. The ablation was considered a success in 97% of cases, with pulmonary vein isolation successful in 99% of such procedures. In addition to performing or confirming pulmonary vein isolation, additional ablation lines were placed in the left atrium in 355 procedures (6% of the total, with a successful result in 354, practically 100%), superior vena cava isolation in 116 procedures (97% success rate), ablation of complex/fragmented electrograms in 50 (80% success rate), and ethanol ablation of the vein of Marshall in 28. A mapping system was used in 3576 procedures (61%).
The percentage of complications related to the AF procedure was maintained at 3.4% (202 of 5848 procedures). The data revealed 55 pericardial effusions (0.9%), 47 vascular complications (0.8%), and 14 embolisms (0.2%), as well as 45 phrenic nerve palsies (0.8%). In addition, there was 1 death associated with an atrioesophageal fistula.
Idiopathic ventricular tachycardiaIVT ablation represented 4% of all procedures, the same number as in 2020. In absolute numbers, with a total of 709 procedures, there was an 8.5% increase vs 2020; however, this is still far from the 807 procedures recorded in 2019. The number of centers performing this ablation dropped considerably, from 88 in 2020 to 75 in 2021, with an average of 9.5 ± 8.3 (range, 1-55) procedures per center. The reported success rate was 81.8%.
Regarding the locations of the tachycardias, 333 involved VT of the right ventricular outflow tract, 123 involved VT of the left ventricular outflow tract, 63 involved VT of the aortic root, 41 were fascicular tachycardias, 30 were epicardial tachycardias, 9 had an origin in the pulmonary artery, and 48 were in other locations, such as the papillary muscles, moderator band, right ventricular free wall, and mitral annulus.
A navigation system was used in 82.5% of procedures and 16.6% were fluoroscopy-free. The use of ablation catheters with an irrigated tip and contact forcesensing technology predominated for this target (78%), whereas the use of irrigated catheters without this technology markedly dropped to 7.8%, vs 24.3% in 2020. Six alcohol ablation procedures were reported, of which 5 were performed in the same center. There were 18 complications (2.5%): 1 atrioventricular block, 4 vascular complications, 12 pericardial effusions, and 1 embolism. There was 1 death after the cardiac surgery due to tamponade and aortic dissection.
Ventricular tachycardia associated with myocardial infarctionVT-AMI ablation comprised 3% of all ablations performed, with 453 procedures in 403 patients. This represented a very slight increase vs 2020 (31 procedures more); the procedure was performed in 65 centers (mean, 7.1 ± 5.4 procedures per center; range, 1-26). The use of navigation systems fell to 85% vs 91.7% reported in 2020, and just 9 procedures (2%) were fluoroscopy-free. The success rate was 82.6% and the use of ablation catheters with an irrigated tip and contact forcesensing technology was standard, at 90.3% of procedures. Three cases of radioablation were reported, as well as 4 of cryoablation and 1 of alcohol ablation. The data showed an increase in the use of the transseptal approach, reaching 55.8% of procedures; it now exceeds the retroaortic approach, which was used in 41.3%. The combined endocardial/epicardial approach was adopted in 9.5% of procedures while exclusively epicardial access was used in 3.3%. The predominant strategy was ablation of the substrate (66.9% of procedures) while conventional activation mapping was applied in 24.3%. The complication rate was as high as 7.5%, similar to previous years, and comprised 11 vascular complications, 2 atrioventricular blocks, 5 pericardial effusions, 1 embolism, 1 myocardial infarction, and 8 heart failure decompensations. A total of 7 deaths associated with this procedure were reported (1.5% mortality).
Ventricular tachycardia not associated with myocardial infarctionVT-NAMI underwent a slight reduction vs the numbers reported in recent years. A total of 199 procedures were conducted in 184 patients (48 procedures fewer than in 2020) and the number of centers performing this type of ablation also decreased, from 51 in 2020 to 45. The mean number of procedures per center was 4.6 ± 4.4 (range, 1-22) and the success rate was 74.9%. A nonfluoroscopic navigation system was used in most procedures (96%). The substrates treated included nonischemic dilated cardiomyopathy, 112 (77.7% success rate); arrhythmogenic cardiomyopathy, 29 (86.2% success rate); hypertrophic cardiomyopathy, 9 (100% success rate); congenital heart diseases, 17 (88.2% success rate); bundle-branch tachycardia, 9 (88.9% success rate); and 26 miscellaneous conditions, which included Chagas disease, sarcoidosis, myocarditis, and valvular heart disease.
The use of ablation catheters with an irrigated tip and contact forcesensing technology was standard (91%), whereas the other ablation sources were rare, including 3 radioablations, 1 cryoablation, and 1 alcohol ablation. A transseptal approach was used in 35% of procedures and retroaortic in 31.7%. The combined endocardial-epicardial approach was used in 21.6% of procedures while exclusively epicardial was used in 9.5%.
The rate of reported complications was 5%, including 2 atrioventricular blocks, 2 vascular complications, 4 pericardial effusions, 1 thoracic artery bleeding, and 1 lead displacement of an implantable cardioverter-defibrillator. Two deaths occurred, 1 after cardiac tamponade and the other a result of thoracic bleeding in relation to epicardial access.
Mapping systems and zero-fluoroscopy ablationThe percentage of ablation procedures conducted with nonfluoroscopic navigation systems grew vs previous years, from 49% in 2020 to 52% in 2021 (9394 procedures). As a percentage, the ablation target with the greatest use of navigation systems was once again VT (85% of procedures), whereas the use of a navigation system was less common for less complex substrates (AVNRT, AP, CTI, and, in particular, AVN): from 5% for AVN ablation to 46% for AP ablation.
The number of fluoroscopy-free procedures grew to 2929, 16% of the total, slightly higher than the 14% recorded in 2020. The ablation targets most commonly treated without fluoroscopy were once again AVNRT (29%), CTI (28%), and FAT (25%).
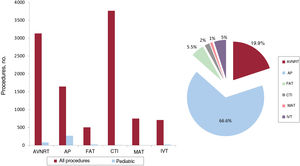
Ablations in pediatric patientsA total of 401 ablations were reported in pediatric patients, representing a 39% increase vs 2020 (158 more ablations performed in 2021). The relative weight of ablations in pediatric patients significantly increased from 1.6% in 2020 to 3.8% in 2021. However, the number of centers reporting ablations in pediatric patients fell from 37 in 2020 to 24. The most frequently treated ablation target in pediatric patients continued to be the APs (66.6% of procedures; 267 procedures), followed by AVNRT (19.9%, 80 procedures), FAT (5.5%, 22 procedures), and IVT (5%, 20 procedures). CTI (2%, 8 procedures) and MAT (1%, 2 procedures) were the least frequently treated ablation targets in this population group. Figure 8 shows the distribution of pediatric procedures by ablation target and their proportion in relation to the total number of procedures.
Distribution of pediatric procedures by ablation target and as a proportion of the total number of procedures. AP, accessory pathway; AVNRT, atrioventricular nodal reentrant tachycardia; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia.
The SARS-CoV-2 pandemic was much less impactful in 2021, and just 29 laboratories (31.2%) provided specific data on the effect of the pandemic on their clinical practice. In 2021, the electrophysiology laboratories were closed due to the pandemic for an average of 9.33 ± 22 days. A total of 70 electrophysiologists (21.17%) were infected with SARS-CoV-2 or were isolated and procedures were performed on 182 patients who tested positive for SARS-CoV-2.
CardioneuroablationFor the first time, cardioneuroablation procedures have been described. A total of 10 centers conducted 31 procedures in 30 patients (1 center, 10 procedures), both as indicated for cardioinhibitory syncope and for sinus node dysfunction. An irrigated catheter with contact forcesensing technology was used in all procedures. Both atria were treated in 24 procedures (77.5%), only the left atrium in 6 (19.3%), and just the right in 1 (3.2%).
DISCUSSIONIn 2021, the growth resumed in the number of procedures, recovering the upward trend seen in the last decade. The consequences of the SARS-CoV-2 pandemic have been much fewer and most of the activity has been restored, without reaching the peak obtained in 2019.
Compared with 2020, the impact of the pandemic was much lower in 2021. Although few centers reported the effects of the pandemic on their activity, the submitted data show few days with laboratory closures, with little impact on personnel by SARS-CoV-2 in terms of isolation or infection.
The increase in the volume of cases observed in 2021 contrasts with the slight decrease in the number of centers providing activity data. This is the second consecutive year with a fall in the number of participating centers, which should act as a general wake-up call and compel us to strengthen participation in order to keep the registry going and ensure it continues to be an accurate reflection of the activity of Spanish centers.
Although there was an increase in practically all ablation targets, the greatest impact (particularly due to its volume) has been on AF, which already represents one-third of all procedures, although Spanish AF activity is still much lower than that of most of our neighboring countries.
One of the most notable findings is the increased number of AF procedures per center. Notably, almost two-thirds of centers already perform more than 50 AF procedures per year and about 20% perform more than 100 (with 3 centers reporting more than 200 procedures).
Regarding the technique of choice for AF ablation, the preference continues for the point-by-point technique. The rapid spread of cryoablation has failed to unseat radiofrequency, which continues to be used in 57.9% of procedures, even though the 2 techniques have similar efficacy.21,22
For the first time, data were collected on the incipient technique of cardioneuroablation. A total of 10 centers reported their initial experience with this technique, both as indicated for cardioinhibitory syncope and for functional sinus node dysfunction. Although we must await the results of studies with robust methodologies, the current data are promising.23
Finally, ablation procedures remain a safe technique with a low rate of complications. This rate has stayed stable over the years but has still not fallen, despite our awareness of the complications. In absolute terms, vascular complications are the most frequent. In this regard, their rate should be reduced as much as possible by the gradual incorporation of ultrasound-guided vascular access. Unfortunately, this is not yet reflected in the reported data. Notably, procedures considered simple (AVNRT, CTI, AVN, and FAT) were associated with a complication rate between 0.5% and 2%, not negligible rates, and this should remind us to adequately inform patients of all procedural risks.
CONCLUSIONSThe Spanish Catheter Ablation Registry has systematically and reliably collected data on the activity and resources of arrhythmia units in Spain for 2 decades. The drop in activity caused by the SARS-CoV-2 pandemic has been overcome and the arrhythmia units have reported strong growth in activity. The overall success rate remains high and the rate of complications is low, and AF was once again consolidated as the most frequently treated ablation target.
FUNDINGNo funding has been received.
AUTHORS’ CONTRIBUTIONSThe first author, I. Anguera, and the coauthors, Ó. Cano Pérez and V. Bazán, contributed equally to this work, which included the study design, data analysis, and manuscript drafting and revision.
CONFLICTS OF INTERESTNone of the authors have any conflicts of interest related to this manuscript.
The coordinators of the registry would once again like to thank all of the participants in the Spanish Catheter Ablation Registry (appendix 2), whose selfless help each year permits the publication of this document. We also thank Cristina Plaza for her invaluable contribution.
Óscar Alcalde Rodríguez, Jesús Almendral-Garrote, Pau Alonso-Fernández, Concepción Alonso-Martín, Luis Álvarez-Acosta, Miguel Álvarez-López, Ignasi Anguera, Álvaro Arce-León, María Fe Arcocha-Torres, Miguel Ángel Arias-Palomares, Antonio Asso-Abadía, Pablo Bastos Amador, Alberto Barrera-Cordero, Javier A. Bellver Navarro, Juan Benezet-Mazuecos, Bruno Bochard-Villanueva, María del Pilar Cabanas-Grandío, Lucas R. Cano-Calabria, Antonio J. Cartón-Sánchez, Silvia del Castillo-Arrojo, Víctor Castro-Urda, Rocío Cózar-León, Paolo D. Dallaglio, Tomás Datino, Ernesto Díaz-Infante, Juan Manuel Durán-Guerrero, Amine El Amrani Rami, Juliana Elices-Teja, Elena Esteban Paul, María del Carmen Expósito-Pineda, Juan Manuel Fernández-Gómez, Julio Jesús Ferrer-Hita, María Luisa Fidalgo-Andrés, Adolfo Fontenla-Cerezuela, Arcadio García-Alberola, Enrique García-Cuenca, Francisco Javier García-Fernández, Miguel García-Pumarino García, Ignacio Gil-Ortega, Federico Gómez-Pulido, Eduard Guasch-i-Casany, José M. Guerra-Ramos, Julio Hernández Afonso, Benito Herreros-Guilarte, Víctor Manuel Hidalgo-Olivares, Alicia Ibáñez-Criado, José Luis Ibáñez-Criado, Sonia Ibars-Campaña, Álvaro Izquierdo Bajo, Javier Jiménez-Candil, Jesús I. Jiménez-López, José Miguel Lozano-Herrera, Ángel Martínez-Brotons, José Luis Martínez-Sande, Gabriel Martín-Sánchez, Roberto Matías-Francés, Elena Mejía-Martínez, Haridian Mendoza Lemes, Diego Menéndez-Ramírez, José Luis Merino-Llorens, Josep Lluis Mont-Girbau, José Moreno-Arribas, Javier Moreno-Planas, Pablo Moriña-Vázquez, Ángel Moya-i-Mitjans, Josep Navarro-Manchón, Joaquín Osca-Asensi, Agustín Pastor-Fuentes, Ricardo Pavón-Jiménez, Alonso Pedrote, Rafael Peinado-Peinado, Luisa Pérez-Álvarez, Andreu Porta-Sánchez, Javier Portales Fernández, Aurelio Quesada-Dorador, Pablo Ramos Ardanaz, Javier Ramos-Maqueda, Nuria Rivas-Gándara, Felipe José Rodríguez-Entem, Enrique Rodríguez-Font, Juan Carlos Rodríguez-Pérez, Rafael Romero-Garrido, José Manuel Rubín-López, José Manuel Rubio-Campal, Ricardo Salgado-Aranda, Pepa Sánchez Borque, María de Gracia Sandín-Fuentes, Georgia Sarquella-Brugada, Axel Sarrias-Mercé, Alba Santos-Ortega, José María Segura-Saint-Gerons, and Irene Valverde-André.
| Andalusia | |
| Cádiz | Hospital Universitario Puerta del Mar (Lucas Cano Calabria) |
| Granada | Hospital Clínico Universitario San Cecilio (José Miguel Lozano Herrera); Hospital Universitario Virgen de las Nieves (Miguel Álvarez López) |
| Huelva | Hospital Juan Ramón Jiménez (Pablo Moriña Vázquez); Hospital Quirón Huelva (Pablo Moriñas Vázquez) |
| Córdoba | Hospital Universitario Reina Sofía (José María Segura Saint-Gerons/Francisco Mazuelos Bellido) |
| Málaga | Hospital Clínico Universitario Virgen de la Victoria (Alberto Barrera Cordero); Hospital Quirónsalud Málaga (Alberto Barrera Cordero); Hospital Quirónsalud Marbella (Alberto Barrera Cordero); Hospital Vithas Málaga (Alberto Barrera Cordero); Hospital Vithas Xanit Internacional Benalmádena (Alberto Barrera Cordero) |
| Sevilla | Clínica HLA Santa Isabel (Álvaro Arce León); Hospital Quirónsalud Infanta Luisa (Rafael Romero Garrido); Hospital Vithas Sevilla (Ernesto Díaz Infante/Rocío Cózar León); Hospital Universitario Virgen de Valme (Ricardo Pavón Jiménez); Hospital Virgen del Rocío (Alonso Pedrote); Hospital Virgen Macarena (Pablo Bastos Amador/Álvaro Izquierdo Bajo); Quirónsalud Sagrado Corazón (Juan Manuel Fernández Gómez) |
| Aragon | Hospital Lozano Blesa (Javier Ramos Maqueda); Hospital Universitario Miguel Servet (Antonio Asso); Quirónsalud Zaragoza (Antonio Asso) |
| Principality of Asturias | Hospital Universitario de Cabueñes (Irene Valverde André); Hospital Universitario Central de Asturias (José Manuel Rubín López) |
| Balearic Islands | Hospital Universitario Son Espases (María del Carmen Expósito Pineda) |
| Canary Islands | |
| Las Palmas | Hospital Perpetuo Socorro (Pablo M. Ruiz Hernández); Hospital Universitario de Gran Canaria Doctor Negrín (Haridian Mendoza Lemes); Hospital Vithas Santa Catalina (Juan Carlos Rodríguez Pérez) |
| Santa Cruz de Tenerife | Complejo Hospitalario Universitario de Canarias (Julio Jesús Ferrer Hita); Hospital San Juan de Dios Tenerife (Julio Hernández Afonso); Hospital Universitario Virgen de la Candelaria (Luis Álvarez Acosta) |
| Cantabria | Hospital Universitario Marqués de Valdecilla (Felipe José Rodríguez Entem) |
| Castile-La Mancha | |
| Toledo | Hospital Universitario de Toledo (Miguel Ángel Arias Palomares) |
| Albacete | Complejo Hospitalario Universitario de Albacete (Víctor M. Hidalgo Olivares) |
| Castile and León | |
| Burgos | Hospital Universitario de Burgos (Francisco Javier García Fernández) |
| León | Hospital de León (María Luisa Fidalgo Andrés) |
| Salamanca | Hospital Universitario de Salamanca (Javier Jiménez Candil) |
| Valladolid | Hospital Clínico Universitario de Valladolid (María de Gracia Sandín Fuentes); Hospital Universitario Río Hortega (Benito Herreros Guilarte) |
| Catalonia | |
| Barcelona | Clínica Corachán (José Guerra Ramos); Clínica Sagrada Família (Ángel Moya i Mitjans); Clínica Teknon (Enrique Rodríguez Font); Hospital Clínic (Eduard Guasch/Lluís Mont); Hospital del Mar (Jesús Jiménez López); Hospital Mútua de Terrassa (Sonia Ibars); Hospital San Joan de Déu (Georgia Sarquella-Brugada); Hospital de la Santa Cruz y San Pablo (Concepción Alonso Martín); Hospital Universitario de Bellvitge (Ignasi Anguera/Paolo D. Dallaglio); Hospital Universitario Dexeus (Ángel Moya i Mitjans); Hospital Universitari Germans Trias i Pujol (Axel Sarrias); Hospital Universitario Vall d’Hebron (Nuria Rivas/Alba Santos) |
| Tarragona | Unidad Funcional Territorial de Electrofisiología Camp de Tarragona (Gabriel Martín Sánchez/Amin Elamrani Rami) |
| Lleida | Hospital Universitario Arnau de Vilanova (Diego Menéndez Ramírez) |
| Valencian Community | |
| Alicante | Cardioritmo Levante: Hospital HLA La Vega, Clínica HLA Vistahermosa, Hospitales IMED Elche y Benidorm (Alicia Ibáñez Criado); Hospital General Universitario de Alicante Doctor Balmis (José Luis Ibáñez Criado); Hospital San Juan de Alicante (José Moreno Arribas) |
| Castellón | Hospital Universitario General de Castellón (Javier A. Bellver Navarro) |
| Valencia | Hospital Clínico Universitario de Valencia (Ángel Martínez Brotons); Hospital de Manises (Pau Alonso Fernández); Hospital General Universitario de Valencia (Aurelio Quesada Dorador); Hospital Universitario de la Ribera (Bruno Bochard Villanueva); Hospital Universitario La Fe (Joaquín Osca Asensi) |
| Extremadura | |
| Badajoz | Complejo Hospitalario Universitario de Badajoz (juan Manuel Durán Guerrero) |
| Cáceres | Hospital de Cáceres (Javier Portales Fernández) |
| Galicia | |
| A Coruña | Complejo Hospitalario Universitario A Coruña (Luisa Pérez Álvarez); Hospital Clínico Universitario Santiago de Compostela (José Luis Martínez Sande) |
| Pontevedra | Hospital Álvaro Cunqueiro (Pilar Cabanas Grandío) |
| Lugo | Hospital Universitario Lucus Augusti (Juliana Elices Teja) |
| Community of Madrid | Fundación Jiménez Díaz (José Manuel Rubio Campal); HM Hospitales (Jesús Almendral Garrote); Hospital Clínico San Carlos (Ricardo Salgado Aranda); Hospital Puerta de Hierro-Majadahonda (Víctor Castro Urda); Hospital La Luz (Juan Benezet Mazuecos); Hospital Ramón y Cajal (Javier Moreno Planas); Hospital Sanitas la Moraleja (Roberto Matía Francés); Hospital Severo Ochoa (Ricardo Salgado Aranda); Hospital Ruber Juan Bravo (José Luis Merino); Hospital Universitario de Getafe (Agustín Pastor Fuentes); Hospital Universitario 12 de Octubre (Adolfo Fontenla Cerezuela); Hospital Universitario Fuenlabrada (Silvia del Castillo); Hospital Universitario La Paz, Sección de Arritmias y Electrofisiología (Rafael Peinado Peinado); Hospital Universitario (General e Infantil) La Paz, Unidad de Electrofisiología Robotizada (José Luis Merino/Antonio Cartón); Hospital Universitario Fundación Alcorcón (Elena Esteban Paúl); Hospital Universitario General de Villalba (José Manuel Rubio Campal); Hospital Universitario Rey Juan Carlos (Federico Gómez Pulido/Elena Mejía Martínez); Hospital Universitario QuirónSalud Madrid y Complejo Hospitalario Ruber Juan Bravo (Andreu Porta-Sánchez/Tomás Datino); Viamed Santa Elena (José Luis Merino) |
| Region of Murcia | Hospital Universitario Santa Lucía (Ignacio Gil Ortega); Hospital Universitario Virgen de la Arrixaca (Arcadio García Alberola) |
| Chartered Community of Navarre | Pamplona: Clínica Universidad de Navarra (Pablo Ramos Ardanaz); Hospital Universitario de Navarra (Óscar Alcalde Rodríguez) |
| La Rioja | Hospital San Pedro La Rioja (Pepa Sánchez Borque) |
| Basque Country | |
| Vizcaya | Hospital de Basurto (Maria Fe Arcocha Torres); Hospital de Cruces (Miguel García-Pumarino García) |
| Álava | Hospital Universitario de Álava (Enrique García Cuenca) |
The collaborators are listed in appendix 1 while the participating electrophysiology laboratories are shown in appendix 2.