This report describes the result of the analysis of the implanted pacemakers reported to the Spanish Pacemaker Registry in 2018.
MethodsThe analysis is based on the information provided by the European Pacemaker Identification Card and supplier-reported data on the overall number of implanted pacemakers.
ResultsInformation was received from 90 hospitals, with a total of 12 148 cards, representing 31% of the estimated activity. Use of conventional and resynchronization pacemakers was 825 and 77 units per million people, respectively. The mean age of the patients receiving an implant was 78.3 years, and 54% of the devices were implanted in people aged> 80 years. A total of 77.1% were first implants and 21.6% corresponded to generator exchanges. Bicameral sequential pacing was the most frequent pacing mode but was less frequently used in patients aged> 80 years and in women. Single chamber VVI/R pacing was used in 28% of patients with sick sinus syndrome and in 24.7% of those with atrioventricular block, despite being in sinus rhythm.
ConclusionsThe total consumption of pacemaker generators in Spain increased by 1.2% compared with 2017, mainly due to an 8.7% increase in cardiac resynchronization therapy with pacemaker generators. Selection of pacing mode was directly influenced by age and sex.
Keywords
Formed in 1990, the Spanish National Pacemaker Data Bank collects information on cardiac pacing activity in Spain. This activity is summarized in the annual report published in Revista Española de Cardiología,1–17 which describes the current implantation practice and the patients’ demographic profiles, adherence to the recommendations of clinical practice guidelines, and trends in various aspects in recent years and compares the results with those of neighboring countries.
METHODSTo prepare the report of the Spanish Pacemaker Registry, we have thus far relied on the European Pacemaker Patient Identification Card (EPPIC), submitted to the National Pacemaker Data Bank by the implant centers. The EPPIC provides demographic and clinical data and information on the type of device implanted. The online CardioDispositivos18 platform, active since January 22 of this year, is designed to support the national pacemaker and implantable defibrillator registries. It was launched by the Spanish Agency of Medicines and Medical Devices in collaboration with the Spanish Society of Cardiology. The objective of this platform, whose use is mandatory for all professionals involved, is to improve the quality of implant-related data and to develop a more effective surveillance system for these medical devices. From now on, submission of the relevant data to the platform will be the way to obtain an EPPIC.
Because not all of the EPPICs are usually submitted, to obtain the total numbers of implanted devices (pacemaker generators and cardiac resynchronization therapy [CRT] devices, both with defibrillation [CRT-D] and without [CRT-P]), we rely on the information provided by the device suppliers. This information is additionally checked against the data published by the European Confederation of Medical Suppliers Association (Eucomed).19
The demographic data required for the calculation of implantation rates are obtained from the updated report of the Spanish National Statistics Institute as of July 1, 2018.20
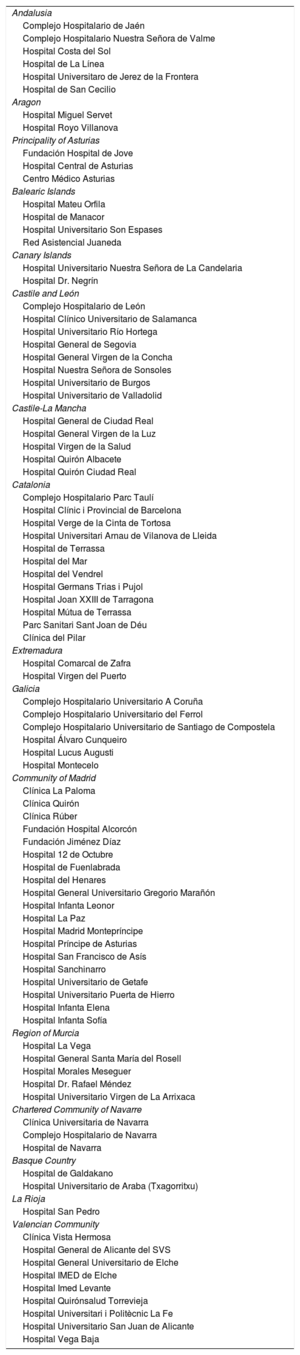
RESULTSSample QualityDuring 2018, 12 148 EPPICs from 90 implant centers were submitted to the National Pacemaker Data Bank (table 1), corresponding to 12 122 generator implantation and 26 lead replacement procedures. This represents 31% of the total activity, according to the data provided by the device suppliers.
Public and Private Hospitals Submitting Data to the Spanish Pacemaker Registry in 2018, Grouped by Autonomous Community
| Andalusia |
| Complejo Hospitalario de Jaén |
| Complejo Hospitalario Nuestra Señora de Valme |
| Hospital Costa del Sol |
| Hospital de La Línea |
| Hospital Universitaro de Jerez de la Frontera |
| Hospital de San Cecilio |
| Aragon |
| Hospital Miguel Servet |
| Hospital Royo Villanova |
| Principality of Asturias |
| Fundación Hospital de Jove |
| Hospital Central de Asturias |
| Centro Médico Asturias |
| Balearic Islands |
| Hospital Mateu Orfila |
| Hospital de Manacor |
| Hospital Universitario Son Espases |
| Red Asistencial Juaneda |
| Canary Islands |
| Hospital Universitario Nuestra Señora de La Candelaria |
| Hospital Dr. Negrín |
| Castile and León |
| Complejo Hospitalario de León |
| Hospital Clínico Universitario de Salamanca |
| Hospital Universitario Río Hortega |
| Hospital General de Segovia |
| Hospital General Virgen de la Concha |
| Hospital Nuestra Señora de Sonsoles |
| Hospital Universitario de Burgos |
| Hospital Universitario de Valladolid |
| Castile-La Mancha |
| Hospital General de Ciudad Real |
| Hospital General Virgen de la Luz |
| Hospital Virgen de la Salud |
| Hospital Quirón Albacete |
| Hospital Quirón Ciudad Real |
| Catalonia |
| Complejo Hospitalario Parc Taulí |
| Hospital Clínic i Provincial de Barcelona |
| Hospital Verge de la Cinta de Tortosa |
| Hospital Universitari Arnau de Vilanova de Lleida |
| Hospital de Terrassa |
| Hospital del Mar |
| Hospital del Vendrel |
| Hospital Germans Trias i Pujol |
| Hospital Joan XXIII de Tarragona |
| Hospital Mútua de Terrassa |
| Parc Sanitari Sant Joan de Déu |
| Clínica del Pilar |
| Extremadura |
| Hospital Comarcal de Zafra |
| Hospital Virgen del Puerto |
| Galicia |
| Complejo Hospitalario Universitario A Coruña |
| Complejo Hospitalario Universitario del Ferrol |
| Complejo Hospitalario Universitario de Santiago de Compostela |
| Hospital Álvaro Cunqueiro |
| Hospital Lucus Augusti |
| Hospital Montecelo |
| Community of Madrid |
| Clínica La Paloma |
| Clínica Quirón |
| Clínica Rúber |
| Fundación Hospital Alcorcón |
| Fundación Jiménez Díaz |
| Hospital 12 de Octubre |
| Hospital de Fuenlabrada |
| Hospital del Henares |
| Hospital General Universitario Gregorio Marañón |
| Hospital Infanta Leonor |
| Hospital La Paz |
| Hospital Madrid Montepríncipe |
| Hospital Príncipe de Asturias |
| Hospital San Francisco de Asís |
| Hospital Sanchinarro |
| Hospital Universitario de Getafe |
| Hospital Universitario Puerta de Hierro |
| Hospital Infanta Elena |
| Hospital Infanta Sofía |
| Region of Murcia |
| Hospital La Vega |
| Hospital General Santa María del Rosell |
| Hospital Morales Meseguer |
| Hospital Dr. Rafael Méndez |
| Hospital Universitario Virgen de La Arrixaca |
| Chartered Community of Navarre |
| Clínica Universitaria de Navarra |
| Complejo Hospitalario de Navarra |
| Hospital de Navarra |
| Basque Country |
| Hospital de Galdakano |
| Hospital Universitario de Araba (Txagorritxu) |
| La Rioja |
| Hospital San Pedro |
| Valencian Community |
| Clínica Vista Hermosa |
| Hospital General de Alicante del SVS |
| Hospital General Universitario de Elche |
| Hospital IMED de Elche |
| Hospital Imed Levante |
| Hospital Quirónsalud Torrevieja |
| Hospital Universitari i Politècnic La Fe |
| Hospital Universitario San Juan de Alicante |
| Hospital Vega Baja |
At the same time, given that the EPPICs were not fully completed in a non-negligible number of cases, various data were missing on each parameter analyzed: lead position (0.3%), age (19%), lead polarity (20%), sex (25.8%), type of lead fixation (28.4%), electrocardiogram (ECG) (46.2%), preimplant symptoms (49.9%), etiology (61.6%), reason for generator explantation (82.4%), and reason for lead explantation (92.9%). Nonetheless, we consider the sample to be representative of the cardiac pacing activity of our country. The results in the report refer to calculations based on the available data, excluding missing information.
Numbers of Pacemaker Generators ImplantedAccording to the data provided by the suppliers, 38 548 conventional pacemaker devices and 1320 CRT-P devices were implanted in Spain in 2018, giving a total of 39 868 devices. According to Eucomed, 39 329 devices were implanted in total.19
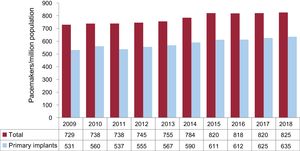
On July 1, 2018, the Spanish population was 46 733 038 inhabitants (22 914 086 men and 23 818 952 women). Thus, considering the total number of conventional pacemakers implanted, the implantation rate was 825 units/million population, slightly higher than that reported by Eucomed (818 units/million) (figure 1).
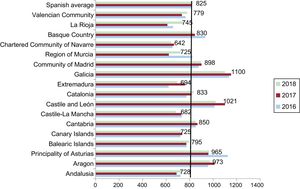
Regarding autonomous communities, Castile and León and Galicia top the list with more than 1000 units/million population, followed by Aragon and the Principality of Asturias with 973 and 965 units/million, respectively. Castile-La Mancha and the Chartered Community of Navarre have the lowest implantation rates, less than 700 units/million (figure 2).
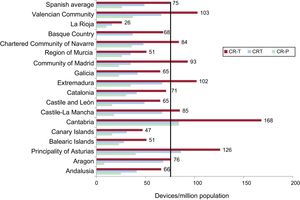
Cardiac Resynchronization DevicesAccording to the data from the Spanish Pacemaker Registry, 1320 CRT-P and 2294 CRT-D devices were implanted in Spain in 2018, giving 3614 CRT-Ts. This indicates a rate of 77 units/million population. The CRT-P rate was 28 units/million, equal to that reported by Eucomed, which represents an 8.7% increase vs the previous year (106 units more).
Cantabria clearly had the highest number of CRT-T implants with 168 units/million population, followed by the Principality of Asturias, the Valencian Community, and Extremadura with 126, 103, and 102 units/million, respectively (figure 3). Cantabria also topped the list in CRT-P implants (84 units/million), whereas La Rioja and Aragon were the communities with the fewest implants (10 and 16 units/million, respectively).
Cardiac resynchronization therapy devices per million population in 2018, national average and by autonomous community. CRT-D, cardiac resynchronization therapy with defibrillation; CRT-P, cardiac resynchronization therapy without defibrillation; CRT-T, total cardiac resynchronization therapy.
The average age of patients with pacemakers was 78.3 years. Age was slightly higher for women than men (79.1 vs 77.8 years) and for replacements vs primary implants (80 vs 78 years). The age range 80 to 89 years old had the highest number of implants (45.1%), followed by 70 to 79 (29.9%), 60 to 69 (10.6%), 90 to 99 (8.9%), and 50 to 59 (3.1%). The percentage of implants was low (2.4%) in those younger than 50 years old and just 0.3% of implanted patients were 100 years or older.
Pacemaker use continues to be higher in men than in women (59.7% vs 40.3%), both in primary implants (60.4% vs 39.6%) and in replacements (57% vs 43%).
Symptoms and EtiologyThe predominant reason for pacemaker implantation was syncope (39%), followed by dizziness (25.9%), heart failure (15.9%), bradycardia (10.9%), and, less frequently, prophylactic reasons (4.7%), tachycardia (1.1%), chest pain (0.8%), aborted sudden cardiac death (0.3%), and brain dysfunction (0.3%); 1.1% corresponded to unspecified causes.
The most frequent cause continues to be unknown etiology or conduction system fibrosis, at 83%, and, at much lower frequency, iatrogenic due to surgical complication, ablation, or medication (4.9%), ischemic heart disease (3.6%), postinfarction (0.6%), cardiomyopathies (1.5%), valvular heart disease (2.5%), carotid sinus syndrome (0.4%), vasovagal syncope (0.1%), transplant (0.2%), and, at less than 0.1%, myocarditis and endocarditis.
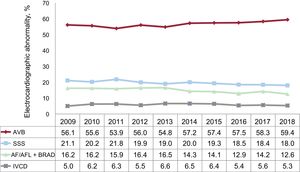
Preimplantation ElectrocardiogramAtrioventricular block (AVB) was the most common electrocardiographic abnormality (59.4%) (figure 4). Third-degree AVB predominated (36.6% of implantations), followed by second-degree AVB (15.6%) and, to a much lower extent, first-degree AVB (1.8%). Atrial fibrillation (AF) with complete heart block accounted for 5.3% of preimplantation ECGs. Sick sinus syndrome (SSS) was the second most common abnormality, present in 30.6% of implantations, and included bradycardia-tachycardia syndrome (6.5%), SSS with bradycardia (5.3%), unspecified SSS (3.8%), and, less commonly, sinus arrhythmia (1.7%) and sinoatrial block (0.5%). Slow AF accounted for 12.6% of abnormal ECG findings. Bundle branch block was found in a smaller percentage, just 5.3%.
Regarding differences according to sex, AVB (excluding blocked AF) was more common in men (55.5% vs 52.8%), whereas SSS (excluding slow AF) was more frequent in women (23.6% vs 15.3%). Bundle branch block as the preimplantation ECG abnormality was more common in men (5.6% vs 3.9%). Blocked or slow AF constituted 19.3% of the indications for men and 15.8% of those for women.
Primary Implants and ReplacementsOf generators implanted, 77.1% were primary implants, 21.6% were generator replacements, 1.1% were replacements of generator and leads, and 0.2% were lead replacements alone.
The most frequent cause of generator explantation was end-of-life battery depletion (87.8%). Other less common causes were elective replacement (6.4%), mechanical infection/erosion (1.7%), premature depletion (1%), advisories (0.6%), hemodynamic optimization due to pacemaker syndrome (0.9%), extracardiac pacing (0.2%), myopotential inhibition (0.2%), and unspecified causes (1.2%).
The most frequent reason for lead replacement was infection/ulceration (72.7% of cases), followed by displacement (18.2%) and, to a lesser extent, insulation failure (9.1%).
Electrode TypeActive fixation leads (88.2%) were much more common than passive fixation leads, in both the atrium (86.6%) and ventricle (89.2%) and in patients ≤ 80 years old and> 80 years old (89.3% and 87.3%, respectively). The vast majority of implanted leads were bipolar (99.8%), in both the atrium (99.9%) and ventricle (99.9%) or in the coronary sinus (98.9%). Magnetic resonance imaging-compatible leads represented 22.9% of the total leads implanted, 21.6% of the atrial leads and 23.7% of the ventricular leads.
Leadless PacemakersThe number of Medtronic Micra model leadless pacemaker implantations increased to 375 units during 2018, representing an increase of 13% vs the previous year.17 Catalonia and Galicia continue to be the autonomous communities with the highest number of such implantations (85 and 77 units, respectively). Together with the Valencian Community, the Community of Madrid, and the Basque Country, they encompass 80% of the total leadless pacemaker implantations in Spain. Taking these figures into account, leadless pacing continues to account for only 2.4% of all VVI/R devices implanted during 2018.
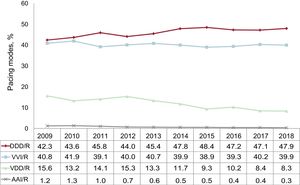
Pacing ModesThe temporal trends in the use of the different pacing modes in recent years are shown in figure 5. Dual-chamber pacing, using either 1 or 2 leads, continues to be the predominant pacing mode. The use of single-lead sequential pacing (VDD/R) was also maintained, at 8.3%, mainly due to a slight rise in replacements (17.2%) because primary implants have decreased to 4.8%. Dual-lead dual-chamber pacing (DDD/R) continues to be the most used mode, with a slight increase vs the previous year to 49.7% of all generators implanted, 55.7% of primary implants and 44.6% of replacements (figure 5). In total, 98% of the dual-chamber devices were implanted with biosensors allowing modification of the pacing frequency.
Single-chamber atrial pacing (AAI/R) continues to decline (0.3%) (figure 5). The number of primary implants in AAI/R mode was stable at 0.2%, as was the number of generator replacements (0.7% of all replacements). Single-chamber ventricular pacing (VVI/R) remained at 40% (37.8% of primary implants and 35.7% of replacements).
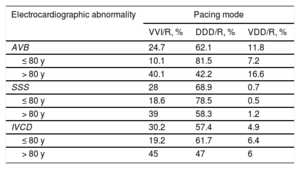
Pacing Mode SelectionAtrioventricular BlockIn this section, patients with AVB and permanent atrial tachyarrhythmia (EPPIC code 8) were excluded to properly assess the degree of adaptation to the most recommended pacing modes.21 Factors possibly influencing this selection were analyzed, such as patients’ age and sex and the degree of blockage.
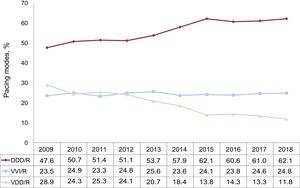
Atrial synchronous pacing (DDD/R and VDD/R modes) predominated (73.9%), with a proportion comparable to that of previous years. The use of DDD/R mode (62.1%) remained stable, whereas VDD/R mode (11.8%) continues to decline. The use of VVI/R mode was stable at 24.7% (figure 6).
The influence of age on the choice of pacing mode was analyzed, as in previous years (table 2). In patients aged ≤ 80 years, pacing maintaining atrioventricular (AV) synchrony clearly predominated (88.6%) and DDD/R mode was the most widely used (81.5%). In this group of patients, the use of the DDD/R mode continues to rise and the use of the VDD/R mode is decreasing (7.2%). Meanwhile, in individuals older than 80 years of age, the use of pacing modes that preserve AV synchrony was much lower (58.7%) and single-chamber ventricular pacing reached 40.1%, a percentage identical to that recorded last year. As in previous years, this age group also showed greater use of the VDD/R mode (16.6%), with a corresponding decrease in the DDD/R mode (42.2%).
Distribution of Pacing Modes by Electrocardiographic Abnormality and Age Group in 2018
| Electrocardiographic abnormality | Pacing mode | ||
|---|---|---|---|
| VVI/R, % | DDD/R, % | VDD/R, % | |
| AVB | 24.7 | 62.1 | 11.8 |
| ≤ 80 y | 10.1 | 81.5 | 7.2 |
| > 80 y | 40.1 | 42.2 | 16.6 |
| SSS | 28 | 68.9 | 0.7 |
| ≤ 80 y | 18.6 | 78.5 | 0.5 |
| > 80 y | 39 | 58.3 | 1.2 |
| IVCD | 30.2 | 57.4 | 4.9 |
| ≤ 80 y | 19.2 | 61.7 | 6.4 |
| > 80 y | 45 | 47 | 6 |
AVB, atrioventricular block; DDD/R, sequential pacing with 2 leads; IVCD, intraventricular conduction defect; SSS, sick sinus syndrome; VDD/R, single-lead sequential pacing; VVI/R, single-chamber ventricular pacing.
Atrial-based pacing continues to be used more in patients with first- and second-degree AVB (78.1%) than in those with third-degree AVB (70.7%). However, these differences were minimal in those younger than 80 years of age (91.4% for first- and second-degree AVB vs 87.7% for third-degree AVB), whereas they were somewhat more pronounced in the population older than 80 years of age (64.6% and 52.8%, respectively).
Sex continues to be a major determinant of the pacing mode. DDD/R pacing was more frequently used in men than in women (66.1% vs 54.7%), whereas VDD/R pacing was used slightly more commonly in women (14.8% vs 11.2%). The same differences were observed according to age range. In women ≤ 80 years of age, the percentage use of the DDD/R mode continued to be lower than in men (79.6% vs 82%), as was the case in previous years, due to greater use of both the VDD/R (8% vs 7.4%) and VVI/R (11.6% vs 8.5%) modes. Notably, in women older than 80 years of age, the use of the VVI/R mode exceeded that of the DDD/R (42.2% vs 36.9%).
Single-chamber ventricular pacing continues to be used in 24.7% of patients with an electrocardiographic diagnosis of AVB with preserved sinus rhythm. This figure is practically identical to those recorded in previous years and was even higher in older patients (40.1% in those older than 80 years) and higher for third-degree AVB and in women of both age bands.
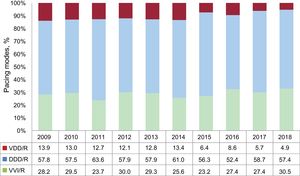
Intraventricular Conduction DefectsBicameral pacing in DDD/R mode accounted for 57.4% of implants and continues to be the most common pacing mode, with figures similar to those of previous years.17 VVI/R mode slightly increased to 30.2%, whereas VDD/R mode slightly decreased to 4.9%. The use of CRT-P devices in patients with an intraventricular conduction defect (IVCD) in sinus rhythm (6.4%) continues to decrease, whereas biventricular pacing in patients with permanent AF remained stable at 0.9%. In general, pacing that maintains AV synchrony continues to predominate, representing 62.3% of all implants (figure 7).
Age continues to be a determinant of the pacing mode in patients with an IVCD (table 2). In patients older than 80 years, the VVI/R mode is much more frequent, at 45%. Use of the DDD/R mode has slightly fallen in this age group, down to 47%, but is once again the most common pacing mode in patients older than 80 years with an IVCD. In contrast, the VVI/R mode was used in only 19.2% of patients aged ≤ 80 years and the DDD/R mode was the most widely used (61.7%). The VDD mode is similarly used in both age groups (6% in those older than 80 years old and 6.4% in those 80 years old or younger).
The use of CRT-P devices to treat ventricular dysfunction slightly decreased (by 7.3%). This drop occurred due to lower use of these devices in younger patients (12.1%), whereas the figure among those older than 80 years remained stable at 1.3%.
Sick Sinus SyndromeAs in previous years, patients with SSS were divided into 2 large groups to assess the adequacy of the pacing modes to the current recommendations in the clinical practice guidelines21: patients who theoretically are in permanent AF or atrial flutter and have bradycardia (EPPIC code E6) and patients who at least theoretically are in sinus rhythm.
- 1.
Sick sinus syndrome in permanent atrial tachyarrhythmia. In total, 93.1% of the generators implanted in this context were VVI/R devices, with DDD/R generators representing 5.2%, a slight decrease vs the previous year; 0.5% were VDD/R devices, despite being hardly justifiable for SSS. In the case of the DDD/R mode, its use can be justified when sinus rhythm restoration is expected. The percentage of patients who received a CRT-P device decreased to 1%.
- 2.
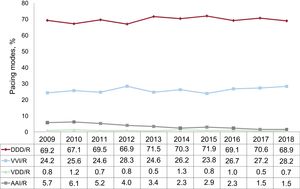
Sick sinus syndrome in sinus rhythm. As recommended by current clinical practice guidelines,20 the most commonly used pacing mode continues to be DDD/R, at 68.9%, followed by 28.2% for VVI/R, 1.5% for AAI/R, and 0.7% for VDD/R (figure 8). Pacing in AAI/R mode remains stable, but slightly increased in VDD mode. In any case, both are at very low percentages, which is in line with the recommendations of the latest clinical practice guidelines published in 2013.21
By separately analyzing the different electrocardiographic manifestations of SSS, excluding EPPIC subgroups E7 and E8 (interatrial block and chronotropic incompetence) due to their minimal representation over the years, the VVI/R pacing mode percentage can be seen to vary between 14.9% and 41.7%; once again, the highest percentage corresponded to bradycardia-tachycardia syndrome (EPPIC subgroup E5). Nevertheless, these numbers may have been inflated by the erroneous inclusion of patients with slow-fast permanent AF episodes in this group and not in the already discussed E6 group.
In patients ≤ 80 years, the most frequently used pacing modes allowed atrial detection and pacing, that is, AAI/R and DDD/R, at 1.2% and 78.5%, respectively, vs only 18.6% for VVI/R mode (table 2). However, in the population older than 80 years of age, the VVI/R mode was used much more frequently (39% vs 58.3% for DDD/R and 0.7% for AAI/R). These figures are similar to those obtained in recent years. There is still a small representation of VDD/R mode in both age groups (0.5% and 1.2%), which represents a slight increase vs previous years, particularly in the group older than 80 years.
Sex also influences the choice of pacing mode, with the VVI/R mode used in 37.2% of women and in 34.4% of men in the older population group (> 80 years). In contrast, in patients ≤ 80 years of age, the VVI/R mode was used much less frequently and was more common in women (17.0% for men vs 19% for women).
Remote MonitoringThis year, 5091 conventional pacemakers (13.2%), 455 CRT-P devices (34%), and 1684 CRT-D devices (73.4%) were included in a remote monitoring program.
DISCUSSIONOnce again, we must stress the need for an improvement in the quality of the sample used for this registry analysis, given the low number of submitted EPPICs due to the lower volume of centers (90 this year vs 106 in 2017). To improve the quality of the sample, it is vital to extend the use of the online platform, a process already underway, in order to increase the reliability of the analyses presented in the report.
In 2018, there was a slight increase in the total number of implanted pacemaker generators, 1.2% according to the Spanish Pacemaker Registry and 0.4% according to Eucomed, after 1 year without growth. This has largely been due to an 8.7% increase in the total number of CRT-P devices vs a 0.9% increase in conventional pacemakers. In 2018, the rate of conventional pacemakers also increased according to the Spanish Pacemaker Registry (825 vs 820 units/million population in 2017), although it is still below the European average (952 units/million). The figure nonetheless exceeds than that of countries such as Switzerland, Norway, the Netherlands, and the United Kingdom, whose per capita incomes are higher than that of Spain.19 The distinct implantation rates of the various countries are probably influenced by differences in health care management, resource distribution, type of funding, and demographic factors.
The number of CRT-T generators has increased by 3.1%, after a 4.7% decrease in 2017 vs the previous year.17 This increase has particularly been due to CRT-P devices, because the number of CRT-D units has remained practically constant. CRT-P devices constitute 36.5% of CRT-Ts, with a CRT-D/CRT-P ratio of 1.7:1. In recent years, there has been an increase in CRT-P devices vs CRT-Ds (2:1 ratio in 2016), probably due to an aging population, the growing evidence of the clinical benefit of the therapy in the elderly population, and modified clinical practice guidelines that recommend the implantation of CRT-P devices in patients indicated for bradycardia pacing, reduced ejection fraction, and a high expected pacing percentage. Despite this increase, Spain continues to be one of the lowest in Europe, only ahead of Greece and Poland, with 12 and 23 units/million, respectively. The low implantation rate in Spain vs the rest of Europe can probably be explained by issues related to health system organization, with an insufficient number of heart failure units that act as referral centers.22
As for implanted generators, slightly more than 75% corresponded to primary implants, and the most frequent cause of replacement was battery depletion. Notably, despite the standardization of preventive measures and the new tools available, such as antibiotic mesh, infection/ulceration remains the cause of 1.7% of generator explantations and 72.7% of lead extractions.23
The growing use of tetrapolar leads for left ventricular pacing is not recognized in the EPPICs and is undoubtedly of interest, given the benefit provided by these leads in terms of the possibility of programming multiple electrical configurations. In the European CRT survey (CRT-Survey II), carried out in 2015 and 2016 in Spain, 74% of the left ventricular leads used were quadripolar.24 The use of MRI-compatible leads continues to rise, reaching 22.9%, which is an 18% increase vs 2017. Nonetheless, their use continues to be insufficient, considering that 75% of patients with these devices will require this imaging modality during their lifetime.25
Leadless pacing showed a very slight rise (13% vs the previous year). Two new autonomous communities have begun to implant this type of device, leaving just 3 communities that have not yet implemented it (La Rioja, Extremadura, and Cantabria).
Pacing modes that maintain AV synchrony continue to predominate in patients with AVB (73.9%). Again, age significantly influences the pacing mode in this group of patients, and the DDD/R mode is mostly used in patients aged ≤ 80 years (81.5%). However, in those older than 80 years of age, the percentage is much lower (42.1%) and is already very close to the percentage of pacing use in VVI/R mode (40.1%).
In patients with SSS, the DDD/R mode remains the most used, at 73.9%. Nonetheless, the VVI/R mode is still used in 21% of patients who are not in permanent atrial tachyarrhythmia, although this figure is slightly lower than that recorded last year. AAI/R mode pacing remains stable at 1.5%, with increasingly lower numbers of primary implants, in accordance with the results of the DANPACE study, which showed AVB rates in patients with SSS of between 0.6% and 1.9%.26 Clinical practice guidelines recommend DDD/R mode in SSS because of its ability to reduce the incidence of AF and strokes, as well as pacemaker syndrome. In patients with permanent atrial tachyarrhythmia, the VVI/R mode still predominates (93.1%).
In 2018, 13.2% of conventional pacemakers were included in a remote monitoring program, which represents an increase of 7.2% vs the previous year. In CRT-P devices, 34.5% of the units include remote monitoring, which represents an increase of 56.3% vs 2017. This datum is important due to the benefits of these monitoring systems, such as the early detection of events, possibility of early therapeutic intervention, reduction in face-to-face visits, and economic savings for the health system.27 For CRT-D units, the figure for devices included in remote monitoring programs were similar to that of the previous year (73.1%).
CONCLUSIONSDuring 2018, the number of pacemaker implantations rose slightly (1.2%), mainly due to an increase in the number of CRT-P generators (8.7%). More than half of the devices were implanted in patients older than 80 years. Pacing modes that maintain AV synchrony remain predominant, although they are less common in older patients and women.
CONFLICTS OF INTERESTNone declared.