To the Editor,
Spontaneous ductus arteriosus aneurysm (DAA) is a sack-like or spindle shaped dilatation due to an intrinsic anomaly of intraductal tissue related to elastin. It is usually diagnosed within the first 2 months of life,1 but can be detected at any age, occasionally after surgical closure of a patent ductus.2 This is a rare potentially severe heart condition; however, prenatal screening has shown a greater prevalence than expected and a more benign natural evolution during infancy.2
We present the case of a child with a large DAA diagnosed at birth by echocardiography and computed tomography angiography (CT-angio). A see and wait attitude was adopted with series of echocardiograms and complete resolution was seen.
Infant of 49 days of age, born at term, weighed 4.330 kg at birth, with a normal perinatal period, without maternal diabetes, brought for observation and treatment to our service with a diagnosis of DAA. At birth, an echocardiographic study showed a round image on the left of the pulmonary trunk was seen with marked autocontrast in its interior, indicating a ducal aneurysm, subsequently confirmed by CT-angio: partially thrombosed aneurysmatic formation of 20 mm in diameter with a narrow opening (6 mm) on the anterior face of the descendent aorta and with no communication with the pulmonary artery.
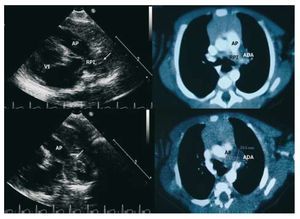
No symptoms were found on physical exam on admission, no murmurs were auscultated, peripheral pulses were preserved and there was no Marfanoid habitus. On x-ray it was possible to see a convex image between the first and second left costal arches. A transthoracic echocardiogram confirmed a large DAA adjacent to the left pulmonary branch, with thrombotic material in its interior and with no evidence of a shunt, which correlated with the CT-angio findings (Figure).
Figure 1. Left: ultrasound images of the "ductal" projection that show the pulmonary branch, and on the left, a rounded thrombus-like mass (aneurysm of the ductus arteriosus, white arrow). Right: angiography images seen by computed tomography in which it is possible to see thrombotic occlusion of the pulmonary end of the ductus. PA indicates pulmonary artery; LPB, left pulmonary branch; LV, left ventricle.
Given the lack of symptoms and the evidence of thrombosis within the aneurysm a conservative strategy was maintained. Echocardiographic control at 3 months was completely normal, with no image of an aneurysm of the permeable ductus.
Spontaneous or congenital DAA is usually not detected and, in many cases, is an incidental finding. In adult patients the pulmonary end is frequently found closed and this is confused with a thoracic aorta aneurysm, which means that its incidence could be underestimated.2 Predisposing risk factors are considered to be maternal diabetes mellitus, high weight at birth and connective tissue disease.3 Current incidence is estimated at 1.5%-8.8%.3,4 Diagnosis can be reliably performed with echocardiography, CT-angio and magnetic resonance.2
Management of spontaneous DAA must be careful without ignoring the possibility of potential complications. Spontaneous rupture with fatal consequences has been described in patients with Marfan syndrome. Furthermore, there have been reports of thrombi extension to the pulmonary arteries or aorta and even thromboembolism, including association with bacterial infections. Large ones may compress or cause erosion of neighbouring structures, vascular, airways or the recurrent laryngeal nerve. The true incidence rate of these complications is unknown, although it is known to be high in older children and adults.2
In some revisions surgical treatment is indicated in patients of more than 2 months of age2 if they have connective tissue disease, infectious syndrome or if there is a aortopulmonary shunt with clinical repercussion.3 It is advisable to closely monitor the patient with these characteristics up to 2-3 months of age to confirm spontaneous remission.2,5 Previously aneurysms of more than 10 mm were operated, although there is no evidence that size is related to a greater complication rate.4 In our case, the DAA was large, but the absence of symptoms and aortopulmonary communication, as also the age of the patient, led us to adopt an attitude of "wait and see." Echocardiographic control at 3 months showed total resolution of the condition with no events; however we continue with regular check-ups to rule out connective tissue diseases of late appearance.