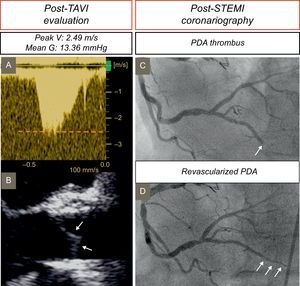
An 87-year-old man with symptomatic severe aortic valve stenosis and a previous percutaneous coronary intervention in the right coronary artery underwent transcatheter aortic valve implantation (TAVI) with a balloon-expandable prosthesis (Edwards Sapien XT). No complications were detected during the procedure guided by transesophageal echocardiography (TEE) (). Posterior transthoracic echocardiography (TTE) demonstrated a normal mean transvalvular gradient (Figure 1A-1B). The patient was discharged with antithrombotic treatment consisting of aspirin 100mg/d indefinitely and clopidogrel 75mg/d for 3 months. One year later, the patient was admitted with inferior ST-segment elevation myocardial infarction and underwent coronary angiography, which showed an abrupt obstruction in the distal part of the posterior descending segment of the right coronary artery, with the typical angiographic appearance of coronary embolism (Figure 1C). Percutaneous coronary intervention was performed with a low profile balloon inflated at very low atmospheres due to the small diameter of the vessel segment where the embolus had stopped (Figure 1D). No evidence of atrial fibrillation during follow-up or hospitalization was observed. Nevertheless, an aortic systolic murmur was detected on exploratory evaluation, with no anemia on laboratory tests or clinical signs of infection. Postprocedural TTE showed an increase in transvalvular aortic gradients compared with a previous study (Figure 2A). The TEE showed an increase in the thickness of the 3 leaflets with restricted motion compared with the previous echocardiographic study, and an aortic valve area of 1.1cm2 assessed by planimetry (Figure 2B-2D, and ). With a suspected diagnosis of subclinical leaflet prosthetic thrombosis, anticoagulation consisting of acenocoumarol was initiated. Three months later, a follow-up TTE and TEE showed normal transvalvular aortic gradients (Figure 2E) with thinning of the 3 valvular leaflets (Figure 2F-2H, and ).
TTE continuous wave Doppler and 2-dimensional TEE evaluation post-TAVI. A: Postimplantation follow-up TTE shows normal peak velocity and mean transvalvular gradient. B: TEE in the midesophageal long-axis view depicts thin aortic leaflets (arrows). C, D: Coronary angiography images showing a typical embolism lesion with abrupt closure in the posterior descending artery (C arrow), with posterior recanalization after percutaneous transluminal coronary angioplasty (D arrows). Mean G, mean gradient; PDA, posterior descending artery; Peak V, peak velocity; STEMI, ST-segment elevation myocardial infarction; TAVI, transcatheter aortic valve implantation; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography.
TTE continuous wave Doppler, TEE in 2-dimensional midesophageal long-axis and TEE in 2-dimensional short-axis views with explanatory colored illustrations. A: One year after TAVI, there is an increase in peak velocity and mean gradient. B: Aortic leaflets are significantly thickened (white arrows). Thrombosis of the 3 leaflets (yellow arrows) in TAVI in diastole (C) and systole (D) with restricted valve opening demonstrated by TEE images. E: After 3 months of anticoagulation therapy, peak velocity and mean gradient have become normal. F: Aortic leaflets again exhibit thinning (white arrows). Thinning of aortic leaflets (yellow arrows) after anticoagulation medication in diastole (G) and systole (H) observed by TEE. Mean G, mean gradient; OACs, oral anticoagulants; Peak V, peak velocity; STEMI, ST-segment elevation myocardial infarction; TAVI, transcatheter aortic valve implantation; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography.
Subclinical leaflet thrombosis in TAVI has been reported in 3% to 4% of patients with balloon-expandable prostheses beyond the first month postprocedure,1,2 and also in other types of TAVI and surgical biological prosthetic valves.3 The diagnosis is based on leaflet thickening and restricted motion detected by echocardiography or multidetector computed tomography.1–3 Nevertheless, in vitro models have shown mean transvalvular gradients to be increased only when at least 2 leaflets are affected, as in our patient.3 These patients are not under anticoagulation therapy or receive antiplatelet medication alone, and anticoagulation therapy is the first option.3 Although these findings have been described as “subclinical” leaflet thrombosis, patients with this complication have recently been reported to have a higher incidence of stroke and transient ischemic attacks.3,4 Coronary thrombosis has been reported during TAVI.5 However, there have been no previous reports of coronary embolism in the chronic phase secondary to leaflet thrombosis in TAVI, as in our patient. These complications raise the need to review imaging follow-up protocols and antiplatelet/anticoagulation therapy in TAVI patients during the first year after implantation.