The American Society of Echocardiography (ASE) has recently published a document with recommendations for the reintroduction of activity in echocardiography laboratories during the coronavirus disease 2019 (COVID-19) pandemic.1 Regarding stress echocardiography, a key diagnostic tool in patients with coronary heart disease or suspected coronary heart disease, many studies have been delayed, giving priority to the pharmacological modality over the exercise modality, following previous ASE recommendations.2 Nonetheless, exercise stress echocardiography (ESE) provides us with very valuable information such as the patient's functional capacity and chronotropic response. The use of a surgical mask during ESE is currently recommended, since it has been shown to reduce the transmission of respiratory viruses.3 On the other hand, its use during exercise has demonstrated a negative impact on cardiopulmonary capacity, as well as increasing the feeling of discomfort, in healthy volunteers.4 This could lead us to inconclusive studies in our patients. The aim of our study was to assess whether the use of a surgical facemask during ESE negatively impacts on patients’ functional capacity and the percentage of conclusive studies.
We conducted a retrospective analysis including those patients who came to our center to perform an ESE from the resumption of our activity on 10/04/2020 to 30/07/2020. Studies in patients with active or highly suspected severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection were cancelled. We selected those patients in sinus rhythm whose indication was diagnosis or prognostic assessment of coronary heart disease. A symptom-limited standard Bruce protocol was performed. A surgical facemask was placed on all patients to carry out the test, completely covering the nose and mouth, and was not allowed to be removed at any moment. As a control group, we used patients who attended our center to perform an ESE with equal inclusion criteria during the same period in 2019. Of a total of 212 patients, 180 (84.91%) met the inclusion criteria. An experienced echocardiographer acquired rest, peak-exercise and postexercise images. Positive ESE was defined as newly developed wall motion abnormalities during exercise. We calculated predicted MET with the formulas of Gulati [women: 14.7-(0.13 x age)] and Morris [men: 18.0-(0.15 x age)]. A study is considered conclusive when the patient reaches 85% of the age-predicted maximum heart rate. To isolate the effect of facemask use on the variables of interest (MET achieved and percentage of conclusive studies), we performed both multivariate analyses adjusted for theoretical confounders (age, sex, body mass index, coronary heart disease, chronotropic treatment, chronic obstructive pulmonary disease, left ventricular ejection fraction ≤ 50%, and positive ESE result).
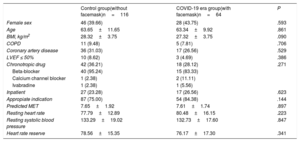
The total study sample consisted of 180 patients, 64 in the COVID-19 era (facemask group) and 116 in the pre-COVID-19 group (control group). Within the total sample, 74 (41.11%) were women, 53 (29.44%) had previous coronary artery disease, 13 (7.22%) had left ventricular systolic dysfunction, and the mean age was 63.54 years (standard deviation, 11.04). The baseline characteristics of the sample distributed by groups are summarized in table 1. We found no differences between the 2 groups in the analyzed variables, except for a nonsignificant trend toward a higher body mass index in the control group.
Baseline characteristics of the patients
| Control group(without facemask)n=116 | COVID-19 era group(with facemask)n=64 | P | |
|---|---|---|---|
| Female sex | 46 (39.66) | 28 (43.75) | .593 |
| Age | 63.65±11.65 | 63.34±9.92 | .861 |
| BMI, kg/m2 | 28.32±3.75 | 27.32±3.75 | .090 |
| COPD | 11 (9.48) | 5 (7.81) | .706 |
| Coronary artery disease | 36 (31.03) | 17 (26.56) | .529 |
| LVEF ≤ 50% | 10 (8.62) | 3 (4.69) | .386 |
| Chronotropic drug | 42 (36.21) | 18 (28.12) | .271 |
| Beta-blocker | 40 (95.24) | 15 (83.33) | |
| Calcium channel blocker | 1 (2.38) | 2 (11.11) | |
| Ivabradine | 1 (2.38) | 1 (5.56) | |
| Inpatient | 27 (23.28) | 17 (26.56) | .623 |
| Appropiate indication | 87 (75.00) | 54 (84.38) | .144 |
| Predicted MET | 7.65±1.92 | 7.61±1.74 | .897 |
| Resting heart rate | 77.79±12.89 | 80.48±16.15 | .223 |
| Resting systolic blood pressure | 133.29±19.02 | 132.73±17.60 | .847 |
| Heart rate reserve | 78.56±15.35 | 76.17±17.30 | .341 |
BMI, body mass index; COPD, chronic obstructive pulmonary disease; LVEF, left ventricular ejection fraction; MET, metabolic equivalents; Heart rate reserve, age predicted maximum heart rate - resting heart rate.
Data are expressed as No. (%) or mean±standard deviation.
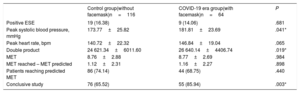
The data on hemodynamic parameters, workload and ESE results are shown in table 2. The main reason for stopping the test in both groups was muscle fatigue (75.00% facemask, 62.93% control, P=.09). The workload reached was very similar in both groups (8.77 MET facemask, 8.76 MET control, P=.984). Compared with patients with the control group, patients in the facemask group had significantly higher peak systolic blood pressure (181.81mmHg vs 173.77mmHg; P=.041) and double product (26 640 vs 24 621; P=.019). We obtained a higher percentage of conclusive studies in the facemask group (85.94% vs 65.52%; P=.003). In the multivariate analysis, the use of the mask maintained a significant positive association with the percentage of conclusive studies (odds ratio, 3.95, 95% confidence interval, 1.52-10.25, P=.005), and was not associated with the MET achieved (beta –0.25, 95% confidence interval, –0.84 to 0.35, P=.411).
Data on hemodynamic, workload and test results
| Control group(without facemask)n=116 | COVID-19 era group(with facemask)n=64 | P | |
|---|---|---|---|
| Positive ESE | 19 (16.38) | 9 (14.06) | .681 |
| Peak systolic blood pressure, mmHg | 173.77±25.82 | 181.81±23.69 | .041* |
| Peak heart rate, bpm | 140.72±22.32 | 146.84±19.04 | .065 |
| Double product | 24 621.34±6011.60 | 26 640.14±4406.74 | .019* |
| MET | 8.76±2.88 | 8.77±2.69 | .984 |
| MET reached – MET predicted | 1.12±2.31 | 1.16±2.27 | .898 |
| Patients reaching predicted MET | 86 (74.14) | 44 (68.75) | .440 |
| Conclusive study | 76 (65.52) | 55 (85.94) | .003* |
ESE, exercise stress echocardiogram; MET, metabolic equivalents; Double product, peak systolic blood pressure x peak heart rate.
Data are expressed as No. (%) or mean±standard deviation.
Previous studies have shown that heart rate during exercise is increased by the use of surgical facemasks in healthy participants.5 This may partly explain the higher percentage of conclusive studies obtained. The main weakness of our study is the impossibility of using the same patients without a facemask as their own control group, given the risk of aerosolization during ESE in the current pandemic situation. Given the retrospective nature of the analysis, it has not been possible to incorporate other variables related to chronotropic response, such as the level of sedentariness. However, this bias was mitigated by the use of body mass index as a surrogate variable. Finally, we cannot exclude a possible causal role of physical deconditioning, caused by confinement, on the maximum heart rate achieved.
In conclusion, our study demonstrates that ESE with a surgical facemask is a feasible procedure. The use of a facemask does not negatively affect the functional capacity of our patients, nor the percentage of conclusive studies. This enables us to benefit from the information provided by the exercise stress modality, while reducing the risk of infection in healthcare personnel. Given the current pandemic situation, and in view of the results of our study, we strongly recommend the systematic incorporation of the surgical facemask in ESE protocols.