The lack of compulsory continuing training in basic life support (BLS) and the absence of its routine monitoring, as well as the serious nature of a cardiopulmonary arrest (CPA) and the clinical magnitude of this problem would suggest that spot-testing of BLS competencies could be very useful to improve clinical care and health care professionals’ training.
To determine the current level of BLS competencies of the health care professionals in the cardiology department of a tertiary hospital, we performed, without warning, an assessment of their knowledge and skills in this area.
The study population comprised 140 nursing professionals and 15 resident physicians, all from a cardiology department that is structured into specialized units (1 coronary care unit, 1 step-down unit, 1 electrophysiology unit, 2 interventional units, and 2 general cardiology units). The study was authorized by the hospital ethics committee. Participants who did not give signed, informed consent were excluded.
The main variables studied were theoretical knowledge of BLS (assessed using a standardized test with questions scored from 0 to 10) and practical skills as reported by a smart mannequin (Resusci Anne QCPR, Laerdal, Norway),1 to calculate, out of a possible score of 100, the overall quality of the cardiopulmonary resuscitation (CPR) according to the European Resuscitation Council 2015 guidelines.1
Data were collected over a 24-hour period to include all shifts and units. Without previous warning, the participants were directed to a room to work through a simulated case, performing 2minutes of CPR. They undertook not to tell their colleagues about this simulation. Prior to this they completed a questionnaire with their demographic, professional, and employment details.
We obtained a sample of 101 health care professionals (table 1), composed of 90 nurses and 11 residents.
Sociodemographic data and scores for theoretical knowledge and practical skills
| Nurses (n=90) | Residents (n=11) | |||
|---|---|---|---|---|
| Sociodemographic profile | Knowledge | Skills | Sociodemographic profile | |
| Age | ||||
| <40 y | 46 (58.2) | 7.65±1.8 | 37.1±25.3 | 27.7±1 |
| >40 y | 33 (41.8) | 5.09±2.7 | 19.1±24.3 | |
| P | <.001 | .002 | ||
| Profession | ||||
| Nurse | 58 (64.4) | 7.47±1.8 | 35.74±25.96 | 73.3% of residents |
| Auxiliary nurse | 32 (35.6) | 5.19±2.94 | 21.87±25.45 | |
| P | <.001 | <.001 | ||
| Sex | ||||
| Male | 12 (13.3) | 6.8±2.53 | 36.92±22.68 | 4 (36.4) |
| Female | 78 (86.7) | 6.54±2.63 | 29.24±26.6 | 7 (63.6) |
| P | .74 | .34 | ||
| Years worked at the hospital | ||||
| <5 | 33 (36.7) | 7.64±2.36 | 39.58±23.92 | 0 to 5 |
| 6-10 | 9 (10) | 6.86±2.26 | 40±30.14 | |
| 11-15 | 16 (17.8) | 6.75±2.17 | 23.56±26.67 | |
| 16-20 | 12 (13.3) | 5.3±2.98 | 28±27.83 | |
| > 20 | 20 (22.2) | 5.41±2.32 | 17.65±23.28 | |
| P | .014 | .031 | ||
| Employment contract | ||||
| Temporary | 37 (41.1) | 7.53±2.41 | 38.11±28.1 | Resident |
| Substitute | 33 (36.7) | 6.28±2.45 | 30.52±25.36 | |
| Permanent | 20 (22.2) | 5.22±2.75 | 16.22±18.63 | |
| P | .007 | .014 | ||
| Unit | ||||
| Coronary care | 55 (61.1) | 7.24±2.2 | 40.44±27.8 | All |
| Ward | 35 (38.9) | 5.6±2.77 | 19.7±20.61 | |
| P | .005 | <.001 | ||
| Last BLS course | ||||
| <6 mo | 14 (15.6) | 6.86±3 | 32.71±26.9 | 2 (18.2) |
| 6 m-1 y | 18 (20) | 7.29±2.3 | 35.24±31 | 3 (27.3) |
| 1-2 y | 27 (30) | 6.38±2.8 | 32.9±28.6 | 5 (45.4) |
| > 2 y | 31 (34.4) | 6.29±2.2 | 23.68±18.7 | 1 (9.1) |
| P | .683 | .391 | ||
| Last CPA attended | ||||
| <6 mo | 36 (40) | 7.11±2.2 | 40.89±29 | 11 (100) |
| 6 m-1 y | 24 (26.7) | 6.33±3 | 26.9±24.9 | 0 |
| 1-2 y | 8 (8.9) | 7±1.7 | 20±16.6 | 0 |
| > 2 y | 13 (14.4) | 5.67±1.9 | 20.83±17 | 0 |
| Never | 9 (10) | 4±5.7 | 0.5±0.7 | 0 |
| P | .294 | .025 | ||
BLS, basic life support; CPA, cardiopulmonary arrest.
Sociodemographic values are expressed as No. (%) and scores for knowledge and skills, as mean±standard deviation. Statistical analysis: Student t test or ANOVA.
The nurses had a mean age of 39.19±13.17 years and were mostly women (86.7%) with a temporary or substitute contract (77.8%), working in the coronary care or step-down unit (61.1%). In 64.4%, more than 1 year had passed since they last attended a BLS course and 90% had attended at least 1 CPA (66.7% within the last year). Most thought that they had sufficient training in CPR, were familiar with the hospital protocol, and thought that the hospital had the responsibility to train its employees.
The residents had a mean age of 27.7 years and were mostly women with 5-year training contracts. All had attended a CPA in the past 6 months and more than half had attended a BLS course more than 1 year prior.
The mean theoretical knowledge score for nursing staff was 6.57 (out of a maximum of 10 points). Those who had been working for less time at the hospital, who had nonpermanent contracts, and worked in the coronary care unit or step-down unit had higher scores, reaching statistical significance.
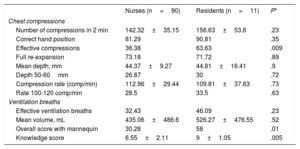
The total score for knowledge and skills in the residents group was significantly higher, particularly for chest compressions (table 2).
Comparison between nurses’ and residents’ knowledge and skills
| Nurses (n=90) | Residents (n=11) | P* | |
|---|---|---|---|
| Chest compressions | |||
| Number of compressions in 2 min | 142.32±35.15 | 156.63±53.6 | .23 |
| Correct hand position | 81.29 | 90.81 | .35 |
| Effective compressions | 36.38 | 63.63 | .009 |
| Full re-expansion | 73.18 | 71.72 | .89 |
| Mean depth, mm | 44.37±9.27 | 44.81±16.41 | .9 |
| Depth 50-60mm | 26.87 | 30 | .72 |
| Compression rate (comp/min) | 112.96±29.44 | 109.81±37.63 | .73 |
| Rate 100-120 comp/min | 28.5 | 33.5 | .63 |
| Ventilation breaths | |||
| Effective ventilation breaths | 32.43 | 46.09 | .23 |
| Mean volume, mL | 435.06±486.6 | 526.27±476.55 | .52 |
| Overall score with mannequin | 30.28 | 58 | .01 |
| Knowledge score | 6.55±2.11 | 9±1.05 | .005 |
Values are expressed as mean±standard deviation.
While the results for BLS theory in both groups were acceptable, the practical skills in the nurses group left room for improvement.
There was a correlation between knowledge scores and CPR skills and employment status: temporary and substitute staff scored higher than permanent staff. One possible reason for this could be a greater interest in continuing professional development courses to improve their curriculum vitae.
Significant differences were found according to the area in which the professional worked. Nurses who worked in the specialized units had better knowledge than those who worked in the general cardiology ward (7.24±2.2 vs 5.6±2.77; P=.005) and scored twice as high on practical skills (40.44±27.8 vs 19.7±20.61; P=.001). These results bear thinking about, since 50% of CPAs occur on general wards.2
There is little evidence on surprise assessment of BLS competencies. An Israeli study of an annual series of surprise simulations reported a progressive improvement in results. After the simulation, the participants received evaluation and feedback.3,4 Surprise testing without warning may give a more realistic view of health professionals’ competencies and can be a very useful tool to plan training.
When organizing training, effective4 and efficient5 methods should be used, and it may be helpful to carry out spot-testing, which gives a real perspective of the professionals’ level of training and can serve to refresh and maintain their skills.3
Our results show that the BLS competencies of the nurses in the cardiology department of this tertiary hospital were modest. The best results were associated with being a resident physician and, among nursing staff, age < 40 years, < 10 years’ professional practice, having a temporary contract, and working in a specialized unit.4
FUNDINGNone.
AUTHORS’ CONTRIBUTIONSJ. Castillo García: concept, methodology, formal analysis, investigation, results, data management, drafting the manuscript, review and editing of the manuscript, supervision, project management. M.I. Barrionuevo Sánchez: concept, methodology, drafting the manuscript, supervision, project management. J.C. Sánchez-Salado: concept, methodology, review and editing of the manuscript, supervision, project management. C-S. Molina Mazón and D. Arbonés Arqué: methodology, writing, review and editing. Albert Ariza-Solé: concept, methodology, drafting the manuscript and review and editing of the manuscript, supervision, project management.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.