Most studies assessing the risk of sudden death in patients with tetralogy of Fallot report a 2% to 3% risk per decade with increased late mortality after surgical correction1 and correlation with arrhythmic events. We present the case of a 13-year-old boy with repaired tetralogy of Fallot, who presented with an episode of ventricular tachycardia (VT) triggered by chest trauma.
The patient had a history of tetralogy of Fallot and underwent surgery in 2004, with complete correction by ventriculotomy, transannular pericardial patch, and closure of the ventricular septal defect. He had been asymptomatic until he was punched in the precordial region during a quarrel with some friends. He presented at the walk-in clinic at his health center with palpitations and a feeling of dizziness. A rhythm strip showed regular wide QRS complex tachycardia, indicating sustained monomorphic VT (Fig. 1A). Due to clinical deterioration, the patient was treated with synchronized cardioversion, sinus rhythm was achieved, and the patient was transferred to our hospital.
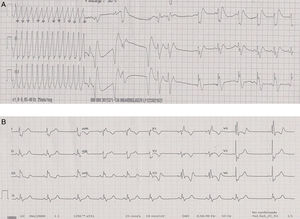
A: Rhythm strip at admission, with regular wide QRS complex tachycardia at 300 beats per minute with an inferior axis, consistent with sustained monomorphic ventricular tachycardia, which reverted to sinus rhythm after synchronized cardioversion. B: Baseline electrocardiogram in sinus rhythm with right bundle branch block of the bundle of His. QRS width, 154ms.
On admission, the patient was asymptomatic and in sinus rhythm (Fig. 1B). Laboratory tests showed no abnormal findings. An echocardiogram showed no significant changes compared with previous studies, a nondilated left ventricle with an ejection fraction of 68%, no contractile asymmetries, a mildly dilated right ventricle (RV) with preserved contractility, and severe pulmonary regurgitation.
During admission, the patient was started on low-dose beta-blocker therapy and he had no further arrhythmias. The study was completed with cardiovascular magnetic resonance, showing dilated RV (RV end-diastolic volume, 210 mL [143 mL/m2], RV end-systolic volume, 108 mL [74 mL/m2]), RV ejection fraction 48%, severe grade pulmonary regurgitation (regurgitant fraction, 43%), and no focal areas of late enhancement in either ventricle.
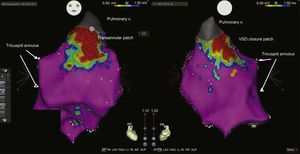
The beta-blocker therapy was discontinued and an electrophysiological study was performed. An anatomical reconstruction and RV voltage map were performed using the CARTO navigation system. The images showed an extensive scarring area from the anterior outflow tract to the pulmonary valve (location of the ventriculotomy and infundibular resection) and a posterior septal scar zone from the ventricular septal defect closure patch (Fig. 2). Programmed ventricular pacing was performed at baseline and during isoproterenol perfusion until the effective refractory period was reached, without induction of ventricular arrhythmias. Finally, after evaluating the different options, a dual-chamber cardioverter-defibrillator was implanted as secondary prevention.
Voltage map of the right ventricle in an anterior (AP) and posterior (PA) image. Scarring area from the pulmonary valve to the anterior outflow tract (ventriculotomy scar and infundibular resection) and another posterior septal scar zone from the VSD closure patch. The yellow dots show the bundle of His. VSD, ventricular septal defect; V, valve.
A complication after a tetralogy of Fallot surgical repair is the onset of VTs (generally macro-reentrant VT2,3) related to different factors, such as increased RV afterload due to residual outflow tract stenosis, RV volume overload due to pulmonary regurgitation secondary to RV outflow tract enlargement surgery, ventriculotomy incision, ventricular septal defect closure patch, and extracorporeal circulation.2,3 Furthermore, cases of cardiac arrhythmias have been described following precordial trauma, sometimes with a fatal outcome.4 To date, however, no case of ventricular tachycardia has been reported in a patient with tetralogy of Fallot in the context of chest trauma.
The hypothesis to explain the trigger mechanism of the sustained monomorphic VT episode in our patient is based on the combination of several of these factors (ventriculotomy incision, severe pulmonary regurgitation and RV dilatation) that gave rise to the arrhythmic substrate that triggered the VT from a punch in the chest. However, the catecholaminergic component should not be ruled out in the context of the emotional stress of the quarrel.
The role of electrophysiological studies has been long debated in the arrhythmia risk stratification of patients with repaired tetralogy of Fallot. According to current clinical practice guidelines, patients with sustained VT should undergo an electrophysiological study. Placement of an implantable cardioverter-defibrillator is recommended, as well as catheter ablation or surgical resection as alternative or adjuvant therapy to an implantable cardioverter-defibrillator in selected patients.5
.