To the Editor,
Tako-Tsubo syndrome occurs predominantly in women over 60 years of age with a history of stress. The presentation resembles acute coronary syndrome, with electrocardiogram changes that normalize within 97-191 days.1 The echocardiogram shows decreased apical contractility with basal hyperkinesia and occasionally, intraventricular gradients,2 and the alterations return in 1-3 weeks. Enzyme elevation is minimal for the alterations described.3 Early catheterization reveals normal coronaries or insignificant lesions.4,5 We present a case of Tako-Tsubo syndrome with significant coronary lesions that do not explain the clinical symptoms. To our knowledge, no similar cases have been described.
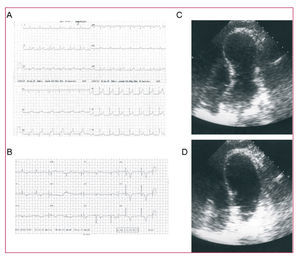
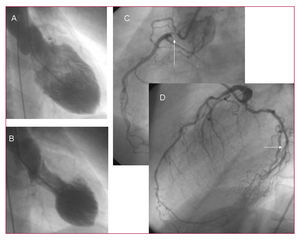
A 61-year-old woman, smoker, with hypertension, and depressive syndrome currently under treatment was seen in the emergency room for oppressive precordial pain radiating to the left arm that worsened upon inspiration, which she experienced after seeing a recently deceased family member on a video tape. The symptoms did not clearly vary with posture, and were accompanied by sweating and nausea. The clinical evolution was over a period of 3 hours. The electrocardiogram (ECG) showed concave ST segment elevation in leads V4-V6, with peaked T waves in all precordial series and short PR-interval in lead II. To investigate pericarditis and the changes in pain with respiration, the patient underwent echocardiography, which showed apical dyskinesia with good basal contractility and a subaortic gradient of 30 mm Hg (Figure 1). Laboratory analysis disclosed a troponin-T concentration of 0.71 and normal creatine kinase. On the basis of suspected Tako-Tsubo with extensive dyskinesia, together with a dubious ECG and the patient's clinical profile, coronary angiography was performed to avoid fibrinolysis. The findings included apical dyskinesia (Figure 2) and two-vessel disease (right coronary and circumflex) with left dominance and a highly developed left anterior descending (LAD) artery; the coronary lesions were not consistent with the contractility alterations.
Figure 1. Electrocardiogram (A: acute, B: discharge), and echocardiogram (C: systole, apical dyskinesia; D: diastole).
Figure 2. Ventriculography (A: diastole; B: systole) and coronary angiography (C: right coronary; D: left coronary).
The patient was admitted to intensive care and treatment was started with beta-blockers and antiplatelet agents, with satisfactory clinical progress. An ultrasound examination at 7 days showed recovery of apical function and resolution of the subaortic dynamic gradient, ECG changes indicating a trend toward generalized subepicardial ischemia.
Tako-Tsubo syndrome was originally described in 1990, although the first series of cases was published in 2001, in Japan.6 Other series from different countries, including Spain, were published later, indicating the global nature of the syndrome.
The etiopathogenesis of this syndrome is still not understood. The mechanisms most commonly cited include:
1. Direct myocardial injury induced by catecholamines.1
2. Dynamic, acute, severe, and transient obstruction of the outflow tract in patients with a predisposition (sigmoid septum and narrow tract), which would cause increased end-diastolic pressure.6
3. Localized or multivessel coronary spasm.
4. Microcirculation alterations.
5. Myocarditis.
6. Self-limiting, acute coronary syndrome in patients with LAD recurrent segment that irrigates an extensive apical-diaphragmatic region, but with a lesion in the middle portion not visualized on angiography, but seen on intravascular ultrasound as disrupted eccentric plaque.7
It is likely that patients with different pathophysiological substrates are included under similar clinical, electrical, and echocardiographic manifestations.
Interestingly, this patient presented significant angiographic lesions in the proximal right coronary and distal circumflex, both vessels with small diameters; nevertheless, the lesions did not explain the extensive contractile alterations observed. The patient was diagnosed with Tako-Tsubo-like syndrome and fibrinolysis was not performed; the contractile alterations were normal by the time of discharge.
On the basis of the findings in this case, we believe that the presence of significant coronary lesions should not rule out the possibility of Tako-Tsubo syndrome when the obstruction (if it occurs) fails to explain a contractility alteration as extensive as the one we describe. Evidently, in other circumstances, we should consider that the patient has had an acute infarction and proceed to emergency revascularization.