A substantial proportion of patients experiencing ST-segment elevation myocardial infarction (STEMI) have a late presentation. There is a lack of temporal trends drawn from large real-word scenarios in these patients.
MethodsAll STEMI patients included in the AMIS Plus registry from January 1997 to December 2017 were screened and patient-related delay was assessed. STEMI patients were classified as early or latecomers according to patient-related delay (≤ or> 12hours, respectively).
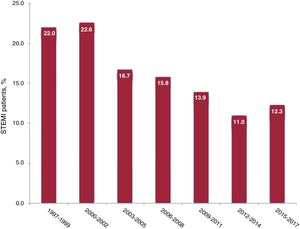
ResultsA total of 27 231 STEMI patients were available for the analysis. During the study period, the prevalence of late presentation decreased from 22% to 12.3% (P <.001). In latecomer STEMI patients, there was a gradual uptake of evidence-based pharmacological treatments (rate of P2Y12 inhibitors at discharge, from 6% to 90.6%, P <.001) and a marked increase in the use of percutaneous coronary intervention (PCI), particularly in 12- to 48-hour latecomers (from 11.9%-87.9%; P <.001). In-hospital mortality was reduced from 12.4% to 4.5% (P <.001). On multivariate analysis, PCI had a strong independent protective effect on in-hospital mortality in 12- to 48-hour latecomers (OR, 0.29; 95%CI, 0.15-0.55).
ConclusionsDuring the 20-year study period, there was a progressive reduction in the prevalence of late presentation, a gradual uptake of main evidence-based pharmacological treatments, and a marked increase in PCI rate in latecomer STEMI patients. In-hospital mortality was reduced to a third (to an absolute rate of 4.5%); in 12- to 48-hour latecomers, this reduction seemed to be mainly associated with the increasing implementation of PCI.
Keywords
A relevant proportion of ST-segment elevation myocardial infarction (STEMI) patients have a late presentation after symptom onset (ie, patient-related delay> 12hours).1 This subgroup of STEMI patients still represents an elusive and challenging population. Indeed, late presentation is associated with adverse clinical outcomes2,3 and, therefore, public health systems have invested a considerable number of resources in reducing patient-related delay.4,5 Previous studies have demonstrated a progressive time-dependent decrease in clinical benefit for reperfusion therapy.6 Latecomers are no more eligible for fibrinolysis.7 Percutaneous coronary intervention (PCI) to achieve reperfusion of the infarct-related artery still seems to be associated with an improvement in prognosis when performed within 12 to 48hours after symptom onset8–11; however, the benefit of late PCI remains controversial, particularly in patients presenting between 24 and 48hours, in whom there are very few available data.12 The present study aimed to evaluate temporal trends deriving from a large real-word scenario in latecomer STEMI patients.
METHODSThe AMIS Plus registry is an ongoing nationwide prospective cohort of patients admitted with a diagnosis of acute coronary syndrome to hospitals in Switzerland. Details of this registry have been provided elsewhere.13,14 Since 1997, of a total of 106 centers treating acute coronary syndromes in Switzerland, 83 centers have been voluntarily providing, temporarily or continuously, blinded data for patients hospitalized for acute coronary syndrome through standardized internet-based or paper-based questionnaires. Among these 83 centers, 24 (29% of the total registry collective) represent tertiary centers with 24-hour primary PCI facilities (meaning access to PCI is provided all hours of the day, every day of the year), accounting for 86% of all 24-hour primary PCI hospitals in Switzerland; globally, 24-hour primary PCI centers represent 26% of the total number of hospitals involved in the treatment of acute coronary syndrome in Switzerland. A list of all participating hospitals can be found on the AMIS Plus web site.15 All data are checked for completeness, plausibility and consistency by the AMIS Plus Data Center. Since 2010, external monitoring has been regularly performed in randomly selected hospitals using randomly selected cases. The present study represents a retrospective post-hoc analysis of data included in the AMIS Plus registry. This registry has been approved by the supra-regional Ethics Committee for Clinical Studies, the Swiss Board for Data Security, and the Cantonal Ethics Commissions and complies with the Declaration of Helsinki.
Patient selectionAll patients with a definitive diagnosis of STEMI included in the AMIS Plus registry from January 1997 to December 2017 were screened. For the present study, STEMI was defined by characteristic symptoms of acute myocardial ischemia, persistent ST-segment elevation on the initial electrocardiogram, and elevation of cardiac biomarkers. ST-segment elevation was defined as follows: at least 2 contiguous leads with ST-segment elevation of 2.5mm in men aged <40 years, 2mm in men aged ≥ 40 years, or 1.5mm in women in leads V2–V3 and/or 1mm in the other leads. Concerning biomarkers, diagnosis of STEMI required an increase in creatinine kinase-MB serum level at least twice above the upper limit of normal and/or an increase in troponin (I or T) serum level above the upper limit of normal; for each biomarker, we used individual hospital cutoffs for diagnosis of myocardial infarction. For each included patient, diagnosis conformed to the prevailing guidelines in use at the time of inclusion.
Patient-related delay (ie, time from symptom onset to first medical contact leading to hospitalization) was then assessed and STEMI patients were classified as early-comers (ie, patients with a symptom-to-door time ≤ 12hours) or latecomers (ie, patients with a symptom-to-door time> 12hours). Of note, both “timing of symptom onset” and “timing of first medical contact leading to hospitalization” were systematically included in the AMIS Plus questionnaire: patient-related delay was determined a posteriori based on these data. The subsequent analyses were essentially focused on latecomer STEMI patients. For this patient subgroup, baseline clinical features were assessed, including all classic cardiovascular risk factors, previous coronary history, and clinical status at admission (Killip class, blood pressure and heart rate at hospitalization, and resuscitation prior to hospital admission). To account for comorbidities, we calculated the Charlson comorbidity index.16 We collected data on immediate drug therapy (defined as therapy administered within the first 24hours of hospitalization), revascularization therapy during the index hospitalization (including door-to-balloon time in patients presenting between 12 and 48hours after symptom onset and undergoing PCI, which was defined as the time interval between first medical contact leading to hospitalization and crossing of the culprit lesion with a guidewire), and drug therapy at discharge to home.
All treatments were prescribed according to current practice and guideline recommendations at the time of the index presentation and treatment choice was left to the discretion of treating physicians. Concerning procedural data, only infarct location and the number of diseased vessels were available in a sufficient number of patients and were, therefore, included in the present analysis. Concerning outcomes, data on mortality, cardiogenic shock, reinfarction, significant bleeding events, and cerebrovascular events during the index hospitalization were collected. The methodology to assess outcomes was uniform during the study. In line with the Killip definition, cardiogenic shock was defined as hypotension with symptoms and/or signs of hypoperfusion. Reinfarction was defined as clinical signs or symptoms of ischemia with ECG changes indicative of new ischemia and a new rise in cardiac biomarkers following the initial infarction. Bleeding complications were recorded if deemed clinically relevant by the individual physician in charge of the patient. Stroke was defined as any event due to ischemic, thrombotic or hemorrhagic disturbance confirmed by a neurologist or an imaging modality.
EndpointsThe study endpoint was analysis of the temporal trend in in-hospital mortality in latecomer STEMI patients. In these patients, we also evaluated temporal trends in prevalence, in-hospital and discharge treatments, and other major in-hospital outcomes. Moreover, we aimed to identify independent predictors of in-hospital mortality in latecomer STEMI patients presenting between 12 and 48hours from symptom onset (hereafter identified as 12- to 48-hour latecomers).
Statistical analysesCategorical variables are presented as percentages. Continuous, normally distributed variables are expressed as the mean±1 standard deviation, while continuous, nonnormally distributed variables are expressed as the median [interquartile range]. Temporal trends were tested using the linear-by-linear test. To assess independent predictors of in-hospital mortality, multivariate analysis was performed with a logistic regression model. All variables included in the final logistic regression model were selected based on known clinical significance or on the results of preliminary age-adjusted logistic regression models. Globally, variables to be entered in the final model were carefully chosen, based on the number of mortality events, to ensure parsimony of the statistical model. To account for the potential confounding effect of changes over time (including variations in pharmacological treatments), we entered the variable “admission period” (as a 3-year period) in the final multivariate analysis. Model fit was assessed using the Hosmer-Lemeshow test. Odds ratios (OR) are reported with 95% confidence intervals (95%CI). A P value of less than .01 was considered significant. IBM SPSS Statistics (version 23, IBM Corp. Armonk, New York, United States) was used for statistical analyses.
RESULTSTrends in the prevalence of late presentationOverall, 27 653 STEMI patients were identified. A total of 422 patients were excluded because of missing data on patient-related delay and thus 27 231 patients were available for the final analysis. Of these, 22 928 patients were early-comers (84%) and 4303 were latecomers (16%). During the study period, the prevalence of late presentation significantly decreased from 22% to 12.3% (P <.001; figure 1).
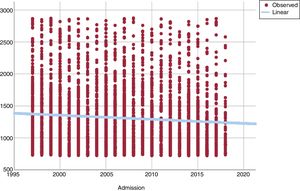
Patient-related delay did not significantly decrease over time within the overall latecomer population (data not shown, P=nonsignificant). However, when we focused only on 12- to 48-hour latecomers (3704 patients, 85% of the overall latecomer population), patient-related delay significantly decreased from 1260 [962-1635] minutes to 1103 [880-1897] minutes (P <.001; figure 2). Similarly, patient-related delay significantly decreased over time in the overall STEMI population from 210 [114-510] minutes to 158 [90-352] minutes (P <.001).
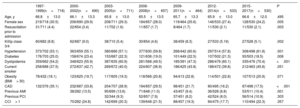
Trends in baseline clinical features in the overall latecomer populationDuring the 20-year study period, there was a significant decrease in the prevalence of female sex from 30.5% to 24.2% (P=.005). The proportion of patients with hypertension and dyslipidemia significantly increased. Conversely, we observed a significant decrease in the proportion of patients with diabetes and a previous history of coronary artery disease or acute myocardial infarction (AMI). There was also a significant reduction in the proportion of patients with resuscitation prior to admission or presenting in advanced Killip class (> 2). Trends in baseline clinical features are summarized in table 1.
Trends in baseline clinical features in latecomer STEMI patients between 1997 and 2017
| 1997-1999(n=718) | 2000-2002(n=690) | 2003-2005(n=711) | 2006-2008(n=657) | 2009-2011(n=464) | 2012-2014(n=533) | 2015-2017(n=530) | P | |
|---|---|---|---|---|---|---|---|---|
| Age, y | 66.8±13.0 | 66.1±13.3 | 65.8±13.0 | 65.5±13.5 | 65.7±13.3 | 65.9±13.0 | 66.6±12.0 | .495 |
| Female sex | 219/718 (30.5) | 206/690 (29.9) | 208/711 (29.3) | 184/657 (28.0) | 119/464 (25.6) | 146/533 (27.4) | 128/530 (24.2) | .005 |
| Resuscitation prior to admission | 31/711 (4.4) | 22/654 (3.4) | 11/702 (1.6) | 11/657 (1.7) | 8/464 (1.7) | 11/530 (2.1) | 11/530 (2.1) | .003 |
| Killip class 3/4 | 60/682 (8.8) | 62/687 (9.0) | 38/710 (5.4) | 30/654 (4.6) | 38/459 (8.3) | 27/533 (5.19) | 27/528 (5.1) | .002 |
| Hypertension | 373/702 (53.1) | 363/659 (55.1) | 380/666 (57.1) | 377/630 (59.8) | 268/442 (60.6) | 297/514 (57.8) | 308/498 (61.8) | .001 |
| Diabetes | 176/703 (25.0) | 158/674 (23.4) | 153/687 (22.3) | 121/636 (19.0) | 101/449 (22.5) | 107/502 (21.3) | 93/503 (18.5) | .006 |
| Dyslipidemia | 359/662 (54.2) | 348/623 (55.9) | 387/635 (60.9) | 281/568 (49.5) | 185/391 (47.3) | 286/476 (60.1) | 335/476 (70.4) | <.001 |
| Current smoker | 258/688 (37.5) | 272/637 (42.7) | 269/672 (40.0) | 224/607 (36.9) | 186/425 (43.8) | 188/472 (39.8) | 212/463 (45.8) | .051 |
| Obesity (BMI> 30) | 78/432 (18.1) | 123/625 (19.7) | 117/605 (19.3) | 118/566 (20.8) | 94/413 (22.8) | 114/501 (22.8) | 107/513 (20.9) | .071 |
| CAD | 132/376 (35.1) | 232/687 (33.8) | 204/707 (28.9) | 194/657 (29.5) | 98/451 (21.7) | 80/495 (16.2) | 87/498 (17.5) | <.001 |
| Previous AMI | 38/282 (13.5) | 95/699 (13.6) | 71/648 (11.0) | 43/457 (9.4) | 36/528 (6.8) | 53/511 (10.4) | .001 | |
| Previous PCI | 32/344 (9.3) | 52/657 (7.9) | 37/451 (8.2) | 42/524 (8.0) | 56/514 (10.9) | .303 | ||
| CCI> 1 | 70/282 (24.8) | 142/699 (20.3) | 139/648 (21.5) | 88/457 (19.3) | 84/475 (17.7) | 110/494 (22.3) | .357 |
AMI, acute myocardial infarction; BMI, body mass index; CAD, coronary artery disease; CCI, Charlson comorbidity index; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
Unless otherwise indicated, values are expressed as proportion (%), or mean±standard deviation.
Concerning immediate pharmacological treatments, there was a significant increase in the use of P2Y12 inhibitors (17.7%-91.5%, P <.001), statins, and renin-angiotensin-aldosterone system blockers during the study period. Conversely, in-hospital use of beta-blockers and glycoprotein IIb-IIIa inhibitors significantly decreased. In 12- to 48-hour latecomers, the PCI rate markedly increased from 11.9% to 87.9% (P <.001). In this patient subgroup, door-to-balloon time significantly decreased from 110 [31-327] minutes to 58 [27-116] minutes (P <.001). Referral for coronary artery bypass grafting in the whole latecomer cohort did not significantly change over time. Data on temporal trends in in-hospital treatments are shown in table 2.
Trends in in-hospital treatments in latecomer STEMI patients between 1997 and 2017
| 1997-1999(n=718) | 2000-2002(n=690) | 2003-2005(n=711) | 2006-2008(n=657) | 2009-2011(n=464) | 2012-2014(n=533) | 2015-2017(n=530) | P | |
|---|---|---|---|---|---|---|---|---|
| Aspirin | 692/716 (96.6) | 645/688 (93.8) | 677/711 (95.2) | 635/654 (97.1) | 451/464 (97.2) | 521/531 (98.1) | 510/529 (96.4) | .016 |
| P2Y12 inhibitor | 124/702 (17.7) | 227/685 (33.1) | 458/707 (64.8) | 538/651 (82.6) | 423/464 (91.2) | 508/533 (95.3) | 485/530 (91.5) | <.001 |
| GP IIb/IIIa inhibitors | 248/686 (36.2) | 244/708 (34.5) | 207/644 (32.1) | 94/451 (20.8) | 79/528 (15.0) | 74/526 (14.1) | <.001 | |
| Beta-blocker | 452/710 (63.7) | 512/688 (74.4) | 532/708 (75.1) | 423/647 (65.4) | 245/457 (53.6) | 275/475 (57.9) | 270/511 (52.8) | <.001 |
| ACE-I/ARB | 317/708 (44.8) | 288/653 (44.1) | 338/706 (47.9) | 397/652 (60.9) | 276/456 (60.5) | 280/479 (58.5) | 310/513 (60.4) | <.001 |
| Statin | 205/356 (57.6) | 527/708 (74.4) | 516/650 (79.4) | 364/457 (79.6) | 393/478 (82.2) | 400/513 (78.0) | <.001 | |
| PCI | 87/718 (12.1) | 334/690 (48.4) | 542/711 (76.2) | 531/657 (80.8) | 386/464 (83.2) | 477/533 (89.5) | 459/530 (86.6) | <.001 |
| PCI in 12-48 h patients | 72/605 (11.9) | 286/575 (49.7) | 497/637 (78.0) | 461/553 (83.4) | 336/376 (89.4) | 128/474 (90.3) | 398/453 (87.9) | <.001 |
| Door-to-balloon time in 12-48 h patients [minutes, IQR] | 110 [31,327] | 78 [20,185] | 72 [24,180] | 60 [22,140] | 58 [27,116] | <.001 | ||
| CABG | 29/627 (4.6) | 26/643 (4.0) | 11/619 (1.8) | 10/427 (2.3) | 10/505 (2.0) | 21/504 (4.2) | .22 |
ACE-I, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor antagonist; CABG, coronary artery bypass graft; GP IIb/IIa, glycoprotein IIb/IIIa inhibitors; IQR, interquartile range; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
Unless otherwise indicated, values are expressed as proportion (%).
At discharge to home, there was a significant increase in the prescription of aspirin (80.9%-96%), P2Y12 inhibitors (6%-90.7%), statins (55.1%-93.5%), and renin-angiotensin-aldosterone system blockers (60.8%-84.2%) (P <.001 for all variables). Trends in discharge treatments are summarized in table 3.
Temporal trends in discharge pharmacological treatments in latecomer STEMI patients between 1997 and 2017
| 1997-1999(n=629) | 2000-2002(n=627) | 2003-2005(n=670) | 2006-2008(n=624) | 2009-2011(n=437) | 2012-2014(n=516) | 2015-2017(n=506) | P | |
|---|---|---|---|---|---|---|---|---|
| Aspirin | 500/618 (80.9) | 561/623 (90.0) | 619/668 (92.7) | 605/622 (97.3) | 426/436 (97.7) | 500/516 (96.9) | 486/506 (96.0) | <.001 |
| P2Y12 inhibitor | 37/616 (6.0) | 298/622 (47.9) | 507/667 (76.0) | 518/619 (83.7) | 399/436 (91.5) | 482/516 (93.4) | 459/506 (90.7) | <.001 |
| Beta-blocker | 411/616 (66.7) | 509/624 (81.6) | 575/665 (86.5) | 510/620 (82.3) | 321/432 (74.3) | 383/515 (74.4) | 354/506 (70.0) | .15 |
| ACE-I/ARB | 374/615 (60.8) | 404/622 (65.0) | 495/667 (74.2) | 518/621 (83.4) | 364/434 (83.9) | 416/516 (80.6) | 426/506 (84.2) | <.001 |
| Statin | 337/612 (55.1) | 471/621 (75.8) | 590/668 (88.3) | 577/621 (92.9) | 405/434 (93.3) | 481/516 (93.2) | 473/506 (93.5) | <.001 |
ACE-I, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor antagonist; STEMI, ST-segment elevation myocardial infarction.
Values are expressed as proportion (%).
During the 20-year study period, in-hospital mortality decreased markedly from 12.4% to 4.5% (P <.001). The prevalence of both cardiogenic shock (14.6%-4.3%) and reinfarction (5.4%-0.2%) developing during the index hospitalization significantly decreased (P <.001 for both variables). Conversely, the prevalence of cerebrovascular events remained fairly stable and there was a strong trend toward a significant increase in the prevalence of bleeding complications (2.1%-5.1%, P=.025). Length of hospitalization in acute care facilities significantly decreased from 10 [6-14] days to 4 [1-7] days (P <.001). Trends in major in-hospital outcomes are shown in detail in table 4.
Temporal trends in in-hospital outcomes in latecomer STEMI patients between 1997 and 2017
| 1997–1999(n=718) | 2000–2002(n=690) | 2003–2005(n=711) | 2006–2008(n=657) | 2009–2011(n=464) | 2012–2014(n=533) | 2015–2017(n=530) | P | |
|---|---|---|---|---|---|---|---|---|
| Length of stay, d | 10 [6-14] | 8 [4-13] | 6 [2-10] | 6 [2-10] | 5 [2-8] | 4 [2-7] | 4 [1-7] | <.001 |
| Cardiogenic shock | 104/710 (14.6) | 80/680 (11.8) | 44/699 (6.3) | 34/657 (5.2) | 19/464 (4.1) | 11/480 (2.3) | 22/514 (4.3) | <.001 |
| Re-infarction | 38/706 (5.4) | 22/681 (3.2) | 15/699 (2.1) | 4/657 (0.6) | 10/464 (2.2) | 3/533 (0.6) | 1/530 (0.2) | <.001 |
| Bleeding event | 7/336 (2.1) | 19/657 (2.9) | 21/464 (4.5) | 17/533 (3.2) | 27/530 (5.1) | .025 | ||
| Cerebrovascular event | 5/708 (0.7) | 11/652 (1.7) | 1/696 (0.1) | 4/657 (0.6) | 2/464 (0.4) | 5/533 (0.9) | 9/530 (1.7) | .42 |
| Mortality | 89/718 (12.4) | 63/690 (9.1) | 41/711 (5.8) | 33/657 (5.0) | 27/464 (5.8) | 17/533 (4.5) | 24/530 (4.5) | <.001 |
STEMI, ST-segment elevation myocardial infarction.
Unless otherwise indicated, values are expressed as proportion (%) or median [interquartile range].
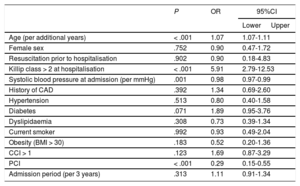
Anterior infarct location and multivessel disease had no impact on in-hospital mortality as assessed in preliminary age-adjusted models and were, therefore, not included in the final logistic regression model (OR, 0.95; 95%CI, 0.65-1.41 and OR, 1.59; 95%IC, 0.90-2.79, respectively; P=nonsignificant for both variables). Similarly, heart rate at hospitalization showed no significant correlation with in-hospital mortality in a preliminary age-adjusted model that also included systolic blood pressure and Killip class at hospitalization and was, therefore, excluded from the final analysis (OR, 1.00; 95%CI, 0.99-1.01; P=.772). In our final logistic regression model, there was a slight but significant direct correlation between age and in-hospital mortality (OR, 1.07; 95%CI, 1.07-1.11; P <.001). Advanced Killip class (> 2) at hospitalization was the strongest independent predictor of in-hospital mortality (OR, 5.91; 95%CI, 2.79-12.53; P <.001). PCI had an impressive independent protective effect on in-hospital mortality with an OR of 0.29 (95%CI, 0.15-0.55; P <.001). Of note, PCI had no protective effect on mortality in patients presenting more than 48hours after symptom onset (OR, 0.41; 95%CI, 0.08-2.04; P=.123). Data from the multivariate analysis are summarized in table 5.
Predictors of in-hospital mortality in 12-48 hours latecomers
| P | OR | 95%CI | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Age (per additional years) | < .001 | 1.07 | 1.07-1.11 | |
| Female sex | .752 | 0.90 | 0.47-1.72 | |
| Resuscitation prior to hospitalisation | .902 | 0.90 | 0.18-4.83 | |
| Killip class > 2 at hospitalisation | < .001 | 5.91 | 2.79-12.53 | |
| Systolic blood pressure at admission (per mmHg) | .001 | 0.98 | 0.97-0.99 | |
| History of CAD | .392 | 1.34 | 0.69-2.60 | |
| Hypertension | .513 | 0.80 | 0.40-1.58 | |
| Diabetes | .071 | 1.89 | 0.95-3.76 | |
| Dyslipidaemia | .308 | 0.73 | 0.39-1.34 | |
| Current smoker | .992 | 0.93 | 0.49-2.04 | |
| Obesity (BMI > 30) | .183 | 0.52 | 0.20-1.36 | |
| CCI > 1 | .123 | 1.69 | 0.87-3.29 | |
| PCI | < .001 | 0.29 | 0.15-0.55 | |
| Admission period (per 3 years) | .313 | 1.11 | 0.91-1.34 | |
95%CI, 95% confidence interval; BMI, body mass index; CAD, coronary artery disease; CCI, Charlson comorbidity index; OR, odds ratio; PCI, percutaneous coronary intervention.
Of interest, neither a door-to-balloon time below 60minutes nor a door-to-balloon time below 90minutes had a significant impact on in-hospital mortality as assessed in 2 distinct age-adjusted models (OR, 0.71; 95%CI, 0.40-1.26; P=.247 and OR, 0.72; 95%CI, 0.42-1.24; P=.236, respectively); cutoffs for the analysis were chosen based on the latest recommendations on STEMI by the European Society of Cardiology.12 Moreover, when we assessed the impact of PCI on in-hospital mortality in an age-adjusted model including total ischemic time (defined as the sum of patient-related delay and door-to-balloon time), PCI was still protective, even if it showed only a strong trend in terms of statistical significance (OR, 0.36; 95%CI, 0.14-0.93; P=.035).
DISCUSSIONThe present study provides the first long-term picture of major temporal trends in late presentation in STEMI. During the 20-year study period, there was a progressive reduction in the prevalence of late presentation. Moreover, we observed a gradual uptake of evidence-based pharmacological treatments in the overall latecomer population and a marked increase in the PCI rate, particularly in 12- to 48-hour latecomers. During the same period, the in-hospital mortality rate markedly declined in the overall latecomer population (from 12.4% to 4.5%). In 12- to 48-hour latecomers, this reduction in mortality seemed to be mainly associated with the increasing implementation of PCI.
The beneficial effect of revascularization is time-dependent6; therefore, public health systems have invested financial and human resources in reducing system- and patient-related delay.4,5 However, to the best of our knowledge, no previously published studies have investigated trends in the prevalence of late presentation in a real-word scenario. A recent study by Al’Aref et al.17 reported a progressive decrease in reperfusion time in STEMI from 2004 to 2012 (a reduction in both symptom-to-door and door-to-balloon times), but the analysis excluded latecomers. In our study, the prevalence of late presentation significantly decreased from 22% to 12.3%. These data likely reflect enhanced awareness in the general population, which currently seeks medical attention earlier when experiencing symptoms potentially suggestive of AMI. However, the prevalence of late presentation remained high at the end of the study period, thus suggesting that additional efforts are still needed to further reduce patient-related delay in STEMI.
Interpretation of trends in baselines clinical features is complicated and not always unequivocal. However, some points are worth consideration. During the 20-year period, the overall latecomer population showed a progressive decrease in the prevalence of female sex, diabetes, and previous history of coronary artery disease/AMI, all previously shown to be independent predictors of late presentation.18 This is likely to be linked to an increased awareness of symptoms suggesting an AMI (especially atypical ones) in these patient subsets. Trends in the prevalence of hypertension and dyslipidemia are difficult to interpret; the increase in the prevalence of these well-known cardiovascular risk factors likely reflects their increase in the AMI population and, more broadly, in the general population.19 In our study, we observed a reduction in the proportion of patients presenting in advanced Killip class and/or with resuscitation prior to hospital admission. This observation is apparently in contrast with the results of a recently published study by Hunziker et al.,20 showing an increase in the prevalence of cardiogenic shock at hospital admission between 2006 and 2017 in the AMIS Plus population, mainly ascribed to an improvement in the prehospital care of critically-ill patients. However, data observed in the present study are likely explained by a more rapid activation of the emergency network by patients experiencing more severe clinical pictures, once again reflecting increased awareness in the general population.
Concerning trends in pharmacological treatments, there was a significant and gradual uptake of all main evidence-based treatments during the study period.12 Of note, both immediate and discharge prescription of P2Y12 inhibitors markedly increased over the 20-year period, reaching a level above 90%. Therefore, the global picture emerging from our study is positive and is in line with available evidence in the overall STEMI population.21 The rate of revascularization by PCI during the index hospitalization also markedly increased, reaching an absolute rate of 87.9% in 12- to 48-hour latecomers. A previous study by Radovanovic et al.,22 based on data from the AMIS Plus registry, reported a similar trend in the overall STEMI population, with a progressive increase in the PCI rate, reaching an absolute rate of 91.8%. In 12- to 48-hour latecomers, most PCI procedures (around 90%) were performed urgently/emergently after hospital admission; door-to-balloon time significantly decreased over time, in line with previous observations in early-comers.17
The most interesting and striking data emerging from our analysis concern trends in major in-hospital outcomes in latecomer STEMI patients. During the study period, overall mortality notably decreased to one third (to an absolute rate of 4.5%). In addition, the prevalence of cardiogenic shock and reinfarction developing during the index hospitalization markedly decreased. Overall length of stay in acute care facilities was significantly reduced to a median of 4 days, with intuitive important financial consequences. Our study provides the first documentation of a reduction of in-hospital mortality in this subgroup of patients. This datum is in line with the results of a recently published study by Radovanovic et al.,22 based on data from the AMIS Plus registry, reporting a marked reduction in the in-hospital mortality rate in the overall STEMI population, with a final age- and sex-adjusted value around 4%. A recent study by McNair et al.,23 comparing outcomes of STEMI patients presenting <12hours and ≥ 12hours after symptom onset and enrolled between January 2011 and December 2016, found an in-hospital mortality around 4% in latecomers, in line with our observations.
The results of our analyses strongly suggest that improvement in in-hospital outcomes in 12- to 48-hour latecomers could be mainly explained by the increasing implementation of revascularization by PCI. The protective effect of PCI in 12- to 48-hour latecomers was preserved despite adjustment for total ischemic time, thus further supporting the idea of a homogeneous beneficial effect of PCI in this subgroup of patients. However, in patients presenting more than 48hours after symptom onset, PCI had no protective effect on in-hospital mortality. Taken together, these data strengthen the hypothesis that PCI is beneficial in patients with a total ischemic time of 12 to 48hours but not in those with a total ischemic time of more than 48hours, in line with latest recommendations on STEMI by the European Society of Cardiology.12 Our results are of particular importance as they derive from a large real-word all-comer population, which also included patients presenting between 24 and 48hours after symptom onset, for whom very few data are available in the literature. Of interest, in 12- to 48-hour latecomers, door-to-balloon time had no impact on in-hospital mortality, thus suggesting that in-hospital delay could be somehow less important in latecomers than in early-comers.17 However, our data should only be taken as hypothesis-generating and dedicated prospective trials are needed to better clarify the optimal timing of PCI in latecomers.
Study limitationsOur study has some limitations. First, the patients were treated at many different hospitals, including centers without PCI facilities, and the choice of interventions and medications was left to the discretion of the treating physicians, which could have caused an unknown bias. However, our data, drawn from a real-life scenario, help to provide a better understanding of the overall burden of late presentation. Moreover, in our study, patient-related delay was defined as “time from symptom onset to first medical contact leading to hospitalization”; this definition slightly differs from the that used in latest guidelines of the European Society of Cardiology on STEMI, which define patient-related delay as “time from symptom onset to first medical contact”.12 We acknowledge that this slightly different definition could have led to an overestimation of delay in the patient subgroup that first alerted the prehospital network. However, in Switzerland, there is an efficient prehospital emergency network, whose activation times are usually very short (fibrinolysis progressively disappeared from national algorithms for the treatment of STEMI). Moreover, the median time of presentation in our latecomer population was well above 12hours throughout the study period. Therefore, we believe that this slight difference in the definition of patient-related delay did not have a major impact on our results. Furthermore, it is not known whether patients were still experiencing symptoms and/or signs suggestive of ongoing ischemia at hospital admission. However, previously published trials showed that patients with ongoing signs of ischemia at hospital admission usually represent only a minority of latecomer STEMI patients, around 15%.8 Therefore, the observed improvements in prognosis more likely reflect a wider clinical benefit of PCI. In our study, we could not account for all clinical, anatomic, and procedural variables potentially influencing clinical outcomes. However, this analysis included most important variables affecting short-term prognosis in STEMI patients. Finally, the lack of data on long-term outcome represents an additional limitation of our study. In AMIS Plus registry follow-up data, obtained through a telephonic interview, are available only for a minority of patients and did not therefore allow meaningful analysis of temporal trends in 1-year mortality or of independent predictors of long-term outcome in our latecomer population.
CONCLUSIONSDuring the 20-year study period, the prevalence of late presentation significantly decreased, likely reflecting greater awareness of AMI presentation in the general population. In the overall latecomer population, there was a gradual uptake of evidence-based pharmacological treatments (both immediate in-hospital and discharge prescription), in line with guideline recommendations; moreover, the PCI rate during the index hospitalization significantly increased, particularly in 12- to 48-hour latecomers. We documented a marked reduction in the in-hospital mortality rate in the overall latecomer population (from 12.4% to 4.5%). In 12- to 48-hour latecomers, this reduction seemed to be mainly associated with the increasing implementation of PCI. Globally, the results of the present study provide further evidence in support of a positive impact of PCI in 12- to 48-hour latecomers and are of particular importance as they derive from a large real-word all-comer population, which also included patients presenting between 24 and 48hours after symptom onset, for whom very few data are available in the literature.
FUNDINGThe AMIS Plus registry is funded by unrestricted grants from the Swiss Heart Foundation and from Abbot AG, Amgen AG, AstraZeneca AG, Bayer (Schweiz) AG, B. Boston Scientific AG, Braun Medical AG, Biotronik AG, Cordis Cardinal Health, Daiichi-Sankyo, Medtronic, Mepha Pharma AG, Novartis Pharma Schweiz AG, SIS Medical AG, St Jude Medical, Terumo, Vascular Medical AG, all in Switzerland. The sponsors did not play any role in the design, data collection, analysis, or interpretation of the registry for the present study.
CONFLICTS OF INTERESTH. Rickli reports institutional research grants from Biotronik, Boston, Braun, Terumo and Medtronic, all outside the submitted work. The other authors report no potential conflicts of interest.
- -
A relevant proportion of patients experiencing STEMI show late presentation after symptom onset (ie, patient-related delay>12hours).
- -
This subgroup of STEMI patients still represents an elusive and challenging population and the benefit of late PCI remains controversial.
- -
There is a lack of temporal trends deriving from a large real-word scenario and focusing on latecomer STEMI patients.
- -
This study provides a comprehensive picture of temporal trends in late presentation over the last 20 years in Switzerland.
- -
During the study period, there was a progressive reduction in the prevalence of late presentation.
- -
In the overall latecomer population, there was a gradual uptake of evidence-based pharmacological treatments and a marked increase in the PCI rate, particularly in 12- to 48-hour latecomers.
- -
For the first time, we document a reduction of in-hospital mortality in the overall latecomer population (from 12.4% to 4.5%). In 12- to 48-hour latecomers, this reduction seemed to be mainly associated with the increasing implementation of PCI.