There are few data on the safety of length of stay in uncomplicated ST-segment elevation myocardial infarction. We studied trends in hospital stay and the safety of short (≤ 3 days) vs long hospital stay in Spain.
MethodsUsing data from the Minimum Basic Data Set, we identified patients with uncomplicated ST-segment elevation myocardial infarction who underwent primary percutaneous coronary intervention and who were discharged alive between 2003 and 2015. The mean length of stay was adjusted by multilevel Poisson regression with mixed effects. The effect of short length of stay on 30-day readmission for cardiac diseases was evaluated in episodes from 2012 to 2014 by propensity score matching and multilevel logistic regression. We also compared risk-standardized readmissions for cardiac diseases and mortality rates.
ResultsThe adjusted length of stay decreased significantly (incidence rate ratio <1; P <.001) for each year after 2003. Short length of stay was not an independent predictor of 30-day readmission (OR, 1.10; 95%CI, 0.92-1.32) or mortality (OR, 1.94; 95%CI, 0.93-14.03). After propensity score matching, no significant differences were observed between short and long hospital stay (OR, 1.26; 95%CI, 0.98-1.62; and OR, 1.50; 95%CI, 0.48-5.13), respectively. These results were confirmed by comparisons between risk-standardized readmissions for cardiac disease and mortality rates, except for the 30-day mortality rate, which was significantly higher, although probably without clinical significance, in short hospital stays (0.103% vs 0.109%; P <.001).
ConclusionsIn Spain, hospital stay ≤ 3 days significantly increased from 2003 to 2015 and seems a safe option in patients with uncomplicated ST-segment elevation myocardial infarction.
Keywords
Primary percutaneous coronary intervention (pPCI) is the ideal reperfusion strategy for ST-segment elevation myocardial infarction (STEMI).1 The pPCI rate has been boosted through the implementation of health care networks, reducing complications and shortening hospital stay.1–4 The current clinical practice guidelines of the European Society of Cardiology consider a short length of hospital stay (48-72hours) to be a valid option for uncomplicated STEMI.1 However, this recommendation is mainly based on older studies with small sample sizes,3,5–10 which undermines reliable analyses of the safety effects of a short length of stay.
In Spain, the recent length of stay trends in STEMI patients treated with pPCI are unknown and no information is available on differences among hospitals and there are no data supporting the recommendation for a short length of stay.1
Thus, the aim of the present study was to evaluate the temporal trends in length of stay in patients admitted to Spanish National Health System (SNS) hospitals with uncomplicated STEMI treated with PCI and its possible association with adjusted rates of 30-day risk of death and readmission for cardiovascular diseases in these patients. The results will help to determine whether the recommendation of a short length of stay for these uncomplicated events is safe in the Spanish SNS and identify possible improvements to the health care process for STEMI in Spain.
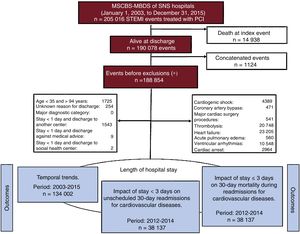
METHODSStudy design, data source, and patient populationThis retrospective observational study investigated patients admitted for STEMI to SNS hospitals and treated with PCI. The data source was the Minimum Basic Data Set (MBDS)11 of the Ministry of Health, Consumer Affairs, and Social Welfare. The usefulness of this database for the study of acute coronary syndrome in Spain was recently validated.12 The following events occurring between January 1, 2003, and December 31, 2005, were selected: patients with a principal diagnosis of STEMI who were treated with PCI and discharged alive (ICD-9-CM codes; ). Patients treated with thrombolysis or cardiac surgery were excluded to reduce analytical biases. Also excluded were patients with any of the following complications associated with the index event: heart failure, acute pulmonary edema, ventricular arrhythmias, cardiac arrest, and cardiogenic shock ().
To improve the consistency and quality of the data, a) events corresponding to patients admitted to one hospital and transferred to another for PCI were concatenated and the lengths of the stay in the referring hospital were attributed to the second hospital, and b) events corresponding to patients younger than 35 years and older than 94 years were excluded, as well as discharges against medical advice or due to transfer to a social health center or an unknown reason, patients with events not causing hospitalization who were discharged to home, patients transferred to another hospital who returned to the referring hospital, and events classified in Major Diagnostic Category 14 (pregnancy, childbirth, and the puerperium) of the All Patient Refined Diagnosis-Related Groups.13
The length of hospital stay, measured in days, was calculated as the difference between the discharge and admission dates and its changes over time were analyzed between 2003 and 2015. The impact of a short length of hospital stay (≤ 3 days) was evaluated for the 2012 to 2014 period because the MBDS enabled reliable identification of readmission events during this period. Outcome variables were unscheduled readmission 30 days after discharge from the index event for cardiovascular diseases (rheumatic heart disease, hypertensive heart disease, ischemic heart disease, pulmonary vascular diseases, other heart diseases, and aortic dissection and aneurysm, as well as other admissions to cardiology and cardiac surgery, regardless of the principal diagnosis) and the in-hospital mortality during these readmissions (because the MBDS does not include out-of-hospital information).
Statistical analysisMultilevel mixed-effects Poisson regression was applied to adjust the length of stay, given its skewed distribution.14 In addition to year of discharge and patient age and sex, the risk factors included in the models designed by the Centers for Medicare and Medicaid Services (CMS methodology) were used to adjust for the risk of mortality and readmission for AMI.15,16 We adapted the models to the structure of the MBDS, after grouping the secondary diagnoses according to the clinical condition categories proposed by Pope et al.,17 updated annually by the Agency for Healthcare Research and Quality.18 The expected length of stay was derived from the individual predictions obtained from the estimated model.
Taking into account the existence of characteristics specific to the patients and to the treating centers that are independent of the quality of the health care provided,19 the 30-day readmission and mortality rates were adjusted for risk according to the CMS methodology. The independent variables were those included in the models for readmission and mortality from AMI, respectively, and a dichotomous variable was included to identify whether the stay was short or long.
Multilevel logistic regression models20 were constructed that, in addition to clinical and demographic variables, included a specific random effect related to the hospital21,22; using backward elimination, significance levels of P <.05 and P ≥ .10 were applied for factor selection and elimination, respectively. The discrimination of the definitive models was assessed using the area under the receiver operating characteristic curve (AUC).
In all multilevel models, if the treating hospital could not be identified, the corresponding events were eliminated; in addition, the incidence rate ratios or odds ratios (ORs) were calculated, as appropriate, as well as their 95% confidence intervals (95%CIs).
The risk-standardized readmission and mortality ratios (RSRRs and RSMRs, respectively) were calculated as the ratios between the expected outcome (which individually considers the functioning of the hospital treating the patient) and the expected outcome (which considers standard functioning according to the average of all hospitals) multiplied by the crude readmission or mortality rate of the study population.18,23 If the RSRR (or RSMR) of a hospital is greater than the crude readmission rate (or crude mortality rate), the probability of readmission (or mortality) in that hospital is higher than the average of the hospitals studied.
To minimize selection bias, the impact of a short length of stay on readmission and mortality during these readmissions was assessed with propensity score matching (k-nearest neighbors matching option, psmatch2, Stata). To do this, we selected long-stay events that, based on the patients’ demographic characteristics and comorbidities, had a similar short-stay probability to that of each short stay event. The matching was performed using the risk adjustment models at a 1:1 ratio and with a maximum propensity score difference (caliper) of 0.05 standard deviations and without replacement. Also calculated were the probability of readmission or death, the effect of the differences between the 2 groups (average treatment effect on the treated [ATT]), and the ORs with their 95%CIs.
To discriminate between high- and low-volume hospitals (according to the number of events attended), a k-means clustering algorithm was used in two thirds of the dataset to obtain the maximum intracluster and minimum intercluster densities, which were validated with the remaining third of the dataset.
The RSRR and RSMR of 30-day readmissions were compared between the 2 length of stay groups classified according to their complexity using the RECALCAR24 typology () and the volume of events recorded.
As sensitivity analysis, the impact of transfers between hospitals was evaluated by excluding index events with discharge due to transfer.
Quantitative variables are presented as means±standard deviations and categorical variables as frequencies and percentages. Correlations among quantitative variables were analyzed with the Spearman rank coefficient (ρ). The t test was used to compare 2 categories, whereas analysis of variance (ANOVA) with the Bonferroni correction was used for 3 or more. Comparisons among discrete variables were made using the chi-square test or Fisher exact test. All comparisons were 2-sided and differences were considered significant at P <.05. All statistical analyses were performed with STATA 13 or SPSS 21.0.
RESULTSTemporal trends in length of hospital stayIn total, 205 016 hospitalization events with STEMI as the principal diagnosis and treatment with PCI were identified; of these, 190 078 patients were discharged alive. Once transfer events were concatenated across hospitals, 188 854 events remained. After exclusions, 134 002 events comprised the study population for the analysis of trends (figure 1).
Flowchart of patients’ events. MSCBS-MBDS, Minimum Basic Data Set provided by the Spanish Ministry of Health, Consumer Affairs, and Social Welfare; PCI, percutaneous coronary intervention; SNS, Spanish National Health System; STEMI, ST-segment elevation myocardial infarction. *Exclusions were not mutually exclusive.
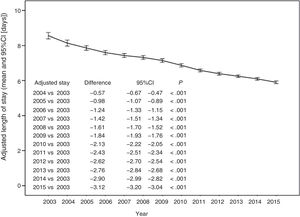
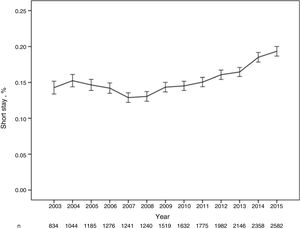
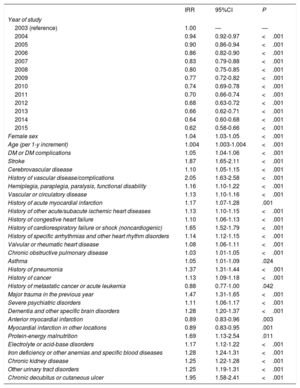
The crude mean length of hospital stay was 7.2±5.5 days and ranged between an annual maximum of 9.0±7.2 days in 2003 and a minimum of 6.1±4.7 days in 2015. The length decreased each year vs the previous year by 3.2%. The adjusted length of hospital stay was significantly reduced (incidence rate ratio <1; P <.001) each year of the period analyzed. With 2003 as reference (table 1), the expected mean lengths of stay showed significant annual differences (figure 2) and the percentage of short lengths of stays increased (from 14.3% in 2003 to 19.3% in 2015; P <.001) (figure 3).
Adjusted model for the length of hospital stay
| IRR | 95%CI | P | |
|---|---|---|---|
| Year of study | |||
| 2003 (reference) | 1.00 | — | — |
| 2004 | 0.94 | 0.92-0.97 | <.001 |
| 2005 | 0.90 | 0.86-0.94 | <.001 |
| 2006 | 0.86 | 0.82-0.90 | <.001 |
| 2007 | 0.83 | 0.79-0.88 | <.001 |
| 2008 | 0.80 | 0.75-0.85 | <.001 |
| 2009 | 0.77 | 0.72-0.82 | <.001 |
| 2010 | 0.74 | 0.69-0.78 | <.001 |
| 2011 | 0.70 | 0.66-0.74 | <.001 |
| 2012 | 0.68 | 0.63-0.72 | <.001 |
| 2013 | 0.66 | 0.62-0.71 | <.001 |
| 2014 | 0.64 | 0.60-0.68 | <.001 |
| 2015 | 0.62 | 0.58-0.66 | <.001 |
| Female sex | 1.04 | 1.03-1.05 | <.001 |
| Age (per 1-y increment) | 1.004 | 1.003-1.004 | <.001 |
| DM or DM complications | 1.05 | 1.04-1.06 | <.001 |
| Stroke | 1.87 | 1.65-2.11 | <.001 |
| Cerebrovascular disease | 1.10 | 1.05-1.15 | <.001 |
| History of vascular disease/complications | 2.05 | 1.63-2.58 | <.001 |
| Hemiplegia, paraplegia, paralysis, functional disability | 1.16 | 1.10-1.22 | <.001 |
| Vascular or circulatory disease | 1.13 | 1.10-1.16 | <.001 |
| History of acute myocardial infarction | 1.17 | 1.07-1.28 | .001 |
| History of other acute/subacute ischemic heart diseases | 1.13 | 1.10-1.15 | <.001 |
| History of congestive heart failure | 1.10 | 1.06-1.13 | <.001 |
| History of cardiorespiratory failure or shock (noncardiogenic) | 1.65 | 1.52-1.79 | <.001 |
| History of specific arrhythmias and other heart rhythm disorders | 1.14 | 1.12-1.15 | <.001 |
| Valvular or rheumatic heart disease | 1.08 | 1.06-1.11 | <.001 |
| Chronic obstructive pulmonary disease | 1.03 | 1.01-1.05 | <.001 |
| Asthma | 1.05 | 1.01-1.09 | .024 |
| History of pneumonia | 1.37 | 1.31-1.44 | <.001 |
| History of cancer | 1.13 | 1.09-1.18 | <.001 |
| History of metastatic cancer or acute leukemia | 0.88 | 0.77-1.00 | .042 |
| Major trauma in the previous year | 1.47 | 1.31-1.65 | <.001 |
| Severe psychiatric disorders | 1.11 | 1.06-1.17 | <.001 |
| Dementia and other specific brain disorders | 1.28 | 1.20-1.37 | <.001 |
| Anterior myocardial infarction | 0.89 | 0.83-0.96 | .003 |
| Myocardial infarction in other locations | 0.89 | 0.83-0.95 | .001 |
| Protein-energy malnutrition | 1.69 | 1.13-2.54 | .011 |
| Electrolyte or acid-base disorders | 1.17 | 1.12-1.22 | <.001 |
| Iron deficiency or other anemias and specific blood diseases | 1.28 | 1.24-1.31 | <.001 |
| Chronic kidney disease | 1.25 | 1.22-1.28 | <.001 |
| Other urinary tract disorders | 1.25 | 1.19-1.31 | <.001 |
| Chronic decubitus or cutaneous ulcer | 1.95 | 1.58-2.41 | <.001 |
95%CI, 95% confidence interval; DM, diabetes mellitus; IRR, incidence rate ratio.
N=132 715; 1287 (0.96%) lost events.
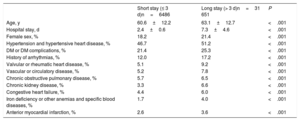
Between January 1, 2012, and December 31, 2014, 38 137 index events (28.5%) were identified from all patients with STEMI index events treated with PCI recorded in the MBDS. Of these, 6486 (17%) were short. Short lengths of stay were more likely in women, younger people, and patients with fewer comorbidities (table 2).
Profile of the patients with index events recorded from 2012 to 2014
| Short stay (≤ 3 d)n=6486 | Long stay (> 3 d)n=31 651 | P | |
|---|---|---|---|
| Age, y | 60.6±12.2 | 63.1±12.7 | <.001 |
| Hospital stay, d | 2.4±0.6 | 7.3±4.6 | <.001 |
| Female sex, % | 18.2 | 21.4 | <.001 |
| Hypertension and hypertensive heart disease, % | 46.7 | 51.2 | <.001 |
| DM or DM complications, % | 21.4 | 25.3 | <.001 |
| History of arrhythmias, % | 12.0 | 17.2 | <.001 |
| Valvular or rheumatic heart disease, % | 5.1 | 9.2 | <.001 |
| Vascular or circulatory disease, % | 5.2 | 7.8 | <.001 |
| Chronic obstructive pulmonary disease, % | 5.7 | 6.5 | <.001 |
| Chronic kidney disease, % | 3.3 | 6.6 | <.001 |
| Congestive heart failure, % | 4.4 | 6.0 | <.001 |
| Iron deficiency or other anemias and specific blood diseases, % | 1.7 | 4.0 | <.001 |
| Anterior myocardial infarction, % | 2.6 | 3.6 | <.001 |
DM, diabetes mellitus.
Total number of patients=38 137.
The most frequent causes of readmission are shown in . The crude rate of 30-day readmission was 2.59% (2.69% for short hospital stays vs 2.61%) and the crude rate of mortality during these readmissions was 0.11% (0.15% vs 0.10%).
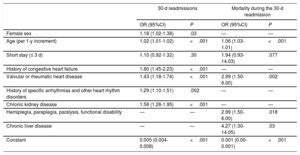
The adjusted risk models of 30-day readmissions and mortality during these admissions are shown in table 3. A short hospital stay was not an independent predictor in either of the models: OR=1.10 (95%CI, 0.92-1.32; P=.30) and OR=1.94 (95%CI, 0.93-14.03; P=.077), respectively.
Independent predictors of 30-day readmission after discharge and mortality during the readmission
| 30-d readmissions | Mortality during the 30-d readmission | |||
|---|---|---|---|---|
| OR (95%CI) | P | OR (95%CI) | P | |
| Female sex | 1.18 (1.02-1.38) | .03 | — | — |
| Age (per 1-y increment) | 1.02 (1.01-1.02) | <.001 | 1.06 (1.03-1.01) | <.001 |
| Short stay (≤ 3 d) | 1.10 (0.92-1.32) | .30 | 1.94 (0.93-14.03) | .077 |
| History of congestive heart failure | 1.80 (1.45-2.23) | <.001 | — | — |
| Valvular or rheumatic heart disease | 1.43 (1.18-1.74) | <.001 | 2.99 (1.50-6.00) | .002 |
| History of specific arrhythmias and other heart rhythm disorders | 1.29 (1.10-1.51) | .002 | — | — |
| Chronic kidney disease | 1.58 (1.28-1.95) | <.001 | — | — |
| Hemiplegia, paraplegia, paralysis, functional disability | — | — | 2.99 (1.50-6.00) | .018 |
| Chronic liver disease | — | — | 4.27 (1.30-14.05) | .03 |
| Constant | 0.005 (0.004-0.008) | <.001 | 0.001 (0.00-0.001) | <.001 |
95%CI, 95% confidence interval; OR, odds ratio.
Discrimination for 30-day readmission was low (AUC=0.65) but was appreciably higher (AUC=0.84) for mortality during these readmissions (). The intraclass correlation coefficients of both models were 0.02 and 0.11, respectively, and their median ORs were 1.3 and 1.8, indicating considerable variability among hospitals.
To analyze the effects of a short hospital stay, propensity score matching was used to obtain 2 cohorts of 12 966 events for readmissions and of 12 972 events for mortality (99.99% and 100% of the events with short hospital stays). The characteristics of these groups are shown in table 4. After matching, there were no significant differences between the 2 groups in 30-day readmissions (ATT=0.024 vs 0.019; P=.204; OR=1.26; 95%CI, 0.98-1.62) or 30-day mortality (ATT=0.001 vs 0.001; P=.52; OR=1.5; 95%CI, 0.48-5.13).
Clinical and demographic characteristics of the patients in the short and long hospital stay groups before and after propensity score matching
| Before matching | After matching | |||||
|---|---|---|---|---|---|---|
| Short stay (≤ 3 d) | Long stay (> 3 d) | P | Short stay (≤ 3 d) | Long stay (> 3 d) | P | |
| Unscheduled 30-d readmissions for cardiovascular disease | ||||||
| Number of valid cases | 6486 | 31 615 | 6483 | 6483 | ||
| Mean age, y | 60.6 | 63.0 | <.001 | 60.6 | 60.7 | .796 |
| Female sex, % | 18.2 | 21.7 | <.001 | 18.2 | 18.4 | .89 |
| Electrolyte imbalance, % | 0.9 | 1.6 | <.001 | 0.9 | 0.8 | .45 |
| History of congestive heart failure, % | 4.4 | 6.0 | <.001 | 4.4 | 4.2 | .70 |
| Acute coronary syndrome, % | 4.9 | 6.9 | <.001 | 4.9 | 4.9 | .90 |
| Valvular or rheumatic heart disease, % | 6.1 | 9.2 | <.001 | 6.1 | 5.0 | .84 |
| History of specific arrhythmias and other heart rhythm disorders, % | 12.0 | 17.2 | <.001 | 12.0 | 12.1 | .87 |
| Renal failure, % | 3.3 | 6.6 | <.001 | 3.3 | 3.3 | .84 |
| Mortality during the 30-d readmission | ||||||
| Number of valid cases | 31 651 | 6486 | 6486 | 6486 | ||
| Mean age, y | 60.6 | 63.0 | <.001 | 60.6 | 60.7 | .86 |
| History of coronary revascularization surgery, % | 0.8 | 0.8 | .81 | 0.8 | 0.9 | .92 |
| Valvular or rheumatic heart disease, % | 5.1 | 9.0 | <.001 | 5.1 | 5.1 | .94 |
| Hemiplegia, paraplegia, paralysis, functional disability | 0.9 | 1.3 | .006 | 0.9 | 0.8 | .64 |
| Chronic liver disease, % | 0.3 | 0.3 | .56 | 0.3 | 0.3 | .37 |
n, number of valid cases.
There were also no significant differences between the 2 groups in the RSRR (2.54% vs 2.55%; P=.020). Although the mean RSMR at 30 days was significantly higher in the short hospital stay group, the difference was probably not clinically significant (0.103% vs 0.109%; P <.001) ().
Impact of patient volume and type of hospitalFrom 2012 to 2014, hospitals with higher volume (> 415 events) had a larger proportion of short hospital stays (18.10% vs 17.10%; P=.02), but no significant differences were found in the mean lengths of stay, the 30-day RSRR, or the 30-day RSMR according to volume (all P > .05). Neither were there significant correlations of the RSMR or RSRR with the patient volume nor were their differences significant according to hospital type (all P> .05).
Sensitivity analysisIn the sensitivity analysis, events corresponding to 4192 patients (11%) from 2012 to 2014 were excluded due to their transfer to another hospital. As in the original models, neither a short hospital stay nor their respective ORs or ATTs obtained from matching were significant.
DISCUSSIONThe main finding of this study is that, with a very large population (that of the Spanish SNS) and an extended period of time (2003-2015), hospitalization of patients with uncomplicated STEMI for ≤ 3 days is practically safe. Our results substantiate the decision of the European clinical practice guidelines to upgrade the level of recommendation for this practice to IIa.1 Another notable finding is the progressive and significant decrease in the mean length of hospital stay in patients admitted for STEMI during the study period, which probably reflects clinical strategy improvements.
After matching, which enables a less biased analysis than RSRR and RSMR comparisons due to an appropriate balance between the short and long hospital stay groups, there were no significant differences.
The RSRR for cardiovascular diseases was also similar in the 2 groups and, although the 30-day RSMR in the short stay group was higher (0.109% vs 0.103%), the difference does not seem clinically relevant because it is equivalent to just 6 deaths/100 000 patients. This represents an excess mortality rate <1 death per year associated with a short hospital stay.
Studies largely performed in the United States have also found a significant decrease in length of hospital stay in recent years.3,4,25 However, in the Spanish SNS, the tendencies in the length of hospital stay for STEMI and its prognostic impact had not been characterized, and the availability of data on the impact of a short hospital stay could help to improve the health care process.
In the CathPCI registry,25 which included 33 920 patients with STEMI treated with pPCI, the proportion of hospital stays ≤ 3 days increased from 24% in 2004 to 30% in 2009, a percentage increase similar to that found in Spain in the 2003 to 2015 period (5%; from 14.30% in 2003 to 19.30% in 2015), although the percentage of stays ≤ 3 days was considerably lower. In a study with more than 50 000 patients, a significantly longer hospital stay was seen (at least 3-4 days) in European countries, including Spain.26 Potentially unnecessary days consumed per 100 patients enrolled ranged between 65 (New Zealand) and 839 (Germany) and the potential for a more efficient hospital stay for low-risk patients was suggested to be particularly marked in European countries. Independently of the causes of these differences, the safety of a short hospital stay for STEMI should underline the significance of an efficient hospital stay. In this regard, the information on the efficiency and safety of a shortened hospital stay for STEMI patients is mainly derived from observational studies,3,6,9,10,25 and few were recent and multicenter.9,25 A recent meta-analysis concluded that a hospital stay ≤ 3 days does not increase the risk of 30-day or 6-month readmission or death.27 However, because the analysis included studies from 1998 to 2016 and had a small sample size, heterogeneous definition of low-risk STEMI, and varying follow-up protocols after discharge, its conclusions are limited.
The reduced length of stay between 2003 and 2015 in our study could be due to more widespread use of PCI and to other therapeutic and STEMI treatment-related improvements and advances, as well as other factors, such as the more efficient clinical management of these patients. However, because the proportion of patients with a hospital stay> 3 days was very high (> 80%), a short hospital stay can be considered uncommon for low-risk patients in Spain. A short hospital stay is a valid alternative for low-risk patients with STEMI,9,10,25 who may represent up to 50% to 70% of all patients with STEMI.5,6,9,25,26 De Luca et al.6 observed that a longer length of stay in low-risk STEMI would only save, at 30 days after discharge, 1 life per 1097 patients, at an additional cost of almost €200 000. In a cost-effectiveness study, Newby et al.28 reported that only 0.006 years of life per patient was saved when patients were hospitalized for an additional (fourth) day. In this regard, we believe that an early monitoring program, particularly in cardiac rehabilitation units, could help to optimize the length of hospital stay. Regardless, the objective of this study was not to explore the estimated saving that a shortened hospital stay could represent, but to reflect the reality of the health care administered in terms of hospital stay and its effect on prognosis. A shorter hospital stay in low-risk patients can reduce complications and costs.29 However, a potential disadvantage could be related to modification of the patients’ perception of the severity of the disease, which could undermine efforts to improve secondary prevention.1
LimitationsAlthough this retrospective analysis is based on administrative data, the validity of administrative registries is comparable to that of medical registries12,22 and the reliability of these studies allows public comparison of hospitals in terms of outcomes.30
In addition, in contrast to the CMS methodology, only readmissions due to cardiovascular disease were analyzed (and mortality during these readmission) due to a lack of events with a principal diagnosis other than that of cardiovascular disease (not included in the MBDS provided by the Spanish Ministry of Health, Consumer Affairs, and Social Welfare). However, cardiac events are probably a better indicator of performance related to length of stay than all-cause readmissions.31 Moreover, the difference in the mortality of patients with STEMI from cardiovascular diseases observed in other studies32,33 vs our findings is likely due to the absence of patient selection in those studies. For example, from our population with STEMI, we excluded patients with heart failure, acute pulmonary edema, ventricular arrhythmias, cardiac arrest, and cardiogenic shock. In addition, readmissions were not considered a recurrent outcome variable. However, the risk of adverse events was low or very low in our population, and a low burden of recurrences would be expected.
Another limitation lies in the inability of ICD-9-CM coding to accurately determine whether primary PCI was performed. However, according to the Spanish Cardiac Catheterization and Coronary Intervention Registry,34 86% of PCIs in STEMI are primary procedures and 5% are rescue PCIs (after fibrinolysis, which were excluded from our study population). Thus, 91% of the PCIs would be primary in our study.
CONCLUSIONSHospital stay for uncomplicated STEMI treated with PCI significantly decreased in Spain between 2003 and 2015, although most patients are still hospitalized for 4 or more days. The discharge of these patients in ≤ 3 days can be considered safe in the SNS and its generalization, in line with the recommendations of the European clinical practice guidelines, would improve the efficient use of health care resources.
FUNDINGThis study has been funded by an unconditional grant from the Fundación Interhospitalaria de Investigación Cardiovascular, Spain (1-2018).
CONFLICTS OF INTERESTE. Abu-Assi is an Associate Editor of Revista Española de Cardiología. The other authors do not declare conflicts of interest.
- –
The increased rate of percutaneous coronary intervention in STEMI has helped to reduce complications and shorten length of hospital stay.
- –
Although the recommendation has recently been strengthened for discharge in less than 3 days in low-risk patients with STEMI, the scientific evidence is slight overall and entirely lacking in the Spanish SNS.
- –
In Spain, hospital stay in STEMI patients significantly shortened from 2003 to 2015. The percentage of short stays (≤ 3 days) significantly increased from 14.30% (2003) to 19.30% (2015).
- –
After propensity score matching, there were no differences in 30-day readmission or mortality during the readmission between a short and a long stay.
To the Institute for Health Information of the SNS. To the Spanish Ministry of Health, Consumer Affairs, and Social Welfare for partial rights to the MBDS database.
Supplementary data associated with this article can be found in the online version at https://doi.org/10.1016/j.rec.2019.09.016