Keywords
INTRODUCTION
Therapeutic Inertia (TI), defined as physicians' failure to begin or intensify indicated treatment,1-3 is common in the treatment of chronic diseases, such as diabetes, hypercholesterolemia, and hypertension, especially during asymptomatic phases.4-6 Among the causes of TI described are physician overestimation of the degree of adherence to clinical practice guidelines (CPG), a false impression of good control of the disease, perception of the patient's poor adherence, and lack of training and organization.1 Other physician-dependent factors, such as age, sex, years of training or training, and research activities during recent years, seem to play an important role in the existence of TI.7 It has also been described as associated with a patient's clinical situation at the time of consultation (laboratory or clinical parameters or treatment received), and to factors such as age, race, sex, or patient comorbidity.3,8-13 However, the results of these studies are not always conclusive. Concretely, studies of lipid management TI have described associations with sex14,15 and age.9,16
There is a clearly established association between a decrease of low density lipoprotein cholesterol (LDL-C) and risk of coronary death.17 According to the latest report of the National Cholesterol Education Program,18 a therapeutic target of LDL-C <100 mg/dL is recommended in patients with ischemic cardiopathy and <70 mg/dL if they are diabetic.
There is evidence of low compliance with the GPC recommendations for lipid management, both in primary and secondary prevention.13,19-22 For example, in the United States less than 33% of patients admitted for myocardial infarction were receiving lipid reducing treatment on discharge,19 and with an LDL-C >160 mg/dL, the probability that the physicians would adjust the statin dose was less than 30%.20 In the United Kingdom, a population study found that 35% of men and 20% of women receiving lipid-reduction treatment achieve the recommended therapeutic targets.21
In Spain, only 13% of patients with dyslipidemia achieved the therapeutic target of LDL-C during initial treatment with lipid-reducing drugs, another 13% achieved the target after changes in treatment, and 74% did not achieve the target after 3 years of follow-up. Paradoxically, the patients in which the therapeutic target was least achieved were those that obtained greatest benefit from lipid-reducing treatment.23
Therapeutic inertia in the management of lipids in chronic ischemic cardiopathy has not been studied. This study has the aim of increasing knowledge of TI in outpatient management of dyslipidemia in patients with chronic ischemic cardiopathy in Spain, in addition to establishing determinant or associated factors. This knowledge is basic to understand this phenomenon better and, therefore, to design strategies to decrease TI.
METHODS
Design
Epidemiological, observational, retrospective and multicentric national study, performed by reviewing clinical records and providing questionnaires to physicians.
Instrument
Based on the factors associated with TI described in previous studies,1-20 the authors designed a questionnaire to collect the data corresponding to 3 information obstacles (physicians, patients and visits).
Patient Inclusion Criteria
a) 18 years of age or over; b) diagnosis of dyslipidemia with drug treatment during the previous 24 months; c) diagnosis of ischemic cardiopathy; d) outpatient follow-up by a cardiologist during the previous 24 months; e) minimum of 3 visits during that period, with a record of the patient's lipid profile; and f) LDL-C >100 mg/dL in at least 1 of the visits.
Predetermination of Sample Size
To detect differences of 4% (eg, 50%-54%) in visit estimations, in a situation of maximum lack of determination (p=q=0.5), with a precision (alpha) of .05 and a statistical power (1-beta) of .8, the number of visits required is 4770. Considering 3 visits per patient (data from 1590 patients are necessary), and 10 patients per physician, 159 physicians must participate.
Sampling
The sample was taken from the clinical registers of a non randomized sample of cardiology consultations throughout Spain. Of the 155 participating cardiologists, 76.7% practiced in the hierarchical external or ambulatory offices of tertiary hospitals, 14.7% in consulting offices in regional hospitals, and the rest were not hierarchical).. Each physician carried out a retrospective review of the clinical records of the first 10 patients with a diagnosis of ischemic cardiopathy and dyslipidemia that met the inclusion criteria in November 2008 and answered the questionnaire.
Definition of Valid Visit
We considered that valid visits were those that included LDL-C measurement and complete treatment data (drug, dose, and adverse effects).
Main Variable
Visits were taken as the unit of analysis, and therefore the main variable is the TI of a visit. There was considered to be TI if no change was made in medication when it should have been. It was defined that a change in medication was necessary when LDL-C >100 mg/dL or >70 mg/dL in diabetic patients.18 The TI was studied for those visits that met the following criteria: a) a change of medication was indicated; b) it was possible to change medication (a possibility that would not exist in patients treated with the most potent statin at its maximum dosage, which at the time of the study was atorvastatin 80 mg/day); and c) lipid-lowering treatment has not caused the patient any adverse effects. The severity of a visit's TI was classified as TI, high TI, or very high TI, according to LDL-C values and the patient's risk factors. Diabetes and smoking have been weighted to a greater degree, since they are the coronary risk factors with the highest adjusted relative risk for the Spanish population, in men and women, respectively24 (Table 1).
Variables
Physician-related: profile (sex, years of experience in their specialty); training (general training courses, and specific courses on dyslipidemia, number of congresses attended in the last 2 years, and annual hours; the physician's estimate of the type, of patients attending their consulting offices (mean number of patients/week, percentage of dyslipidemia among their patients); the physician's opinion on the existence, and reasons for, undertreatment of lipids in ischemic cardiopathy (overloaded care system, ignorance of guidelines, lack of confidence in trial results, fear of medication side effects, lack of protocols, organizational aspects); lipid management in collaboration with primary care services (setting a target level as a treatment objective and referring the patient to primary care to achieve it).
Patient-related: sociodemographic data (sex, age, education, weight, and height); disease data (date of diagnosis of ischemic cardiopathy, of dyslipidemia and of beginning of dyslipidemia drug treatment); cardiovascular risk factors (diabetes, arterial hypertension, stroke, smoking, lifestyle, exercise, and diet).
Visit-related: date; lipid profile (total cholesterol, HDL-C, LDL-C, triglycerides); lipid-lowering treatment at the time of the visit (active ingredients, dosage); side effects of the treatment; any change of medication at this visit, lipid-lowering treatment as a result of the consultation (active ingredients, dosage).
Statistical Analysis
Description of physician, patient, and visit variables. Recoding of variables: treatment with statins on each time of the visit (yes/no) and number of lipid-lowering drugs. Calculation and description of TI and its severity at the visit (N and %). Study of the univariate association between TI at time of visit and the independent variables described using a χ2 test and OR calculation without adjustment. Study of factors associated with the TI of the visit, using a multivariate logistical regression model. The hypothesis was tested using 2-tailed analysis, for a level of significance of α=.05.
RESULTS
Most participating physicians were men and had experience; the data on their characteristics and opinions are shown in Table 2.
In Tables 3 and 4 we summarize the characteristics of the population studied and their lipid profile. As expected, there is a predominance of men, of high mean age, obese or overweight, and former smokers, with a high prevalence of hypertension and diabetes. Risk factors were more frequent in women. Seven of 10 followed a lipid-lowering diet and less than one third carried out regular exercise. In 76.3% of visits, LDL-C was above the target value recommended in the guidelines.
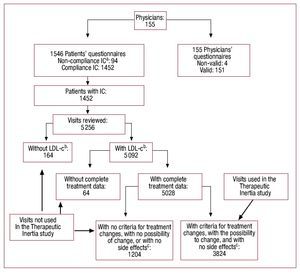
Figure 1 depicts the sampling of valid visits for the study. In 92.1% of visits with complete data, patients received statin treatment, with the following order of frequency: atorvastatin (58.6%), simvastatin (22.8%), pravastatin (9.8%), and lovastatin (1.9%). Globally, there were treatment changes in 46.7% of visits and lipid lowering treatment adverse effects were seen in 2.9%. In 8.3% of visits in which the therapeutic target for LDL-C was not achieved, the patient was receiving the maximum lipid-lowering dose (atorvastatin 80 mg/day). Lastly, the TI study of the visit was performed for 3,824 visits with medication change criteria. In 1636 (42.8%) of the visits there was TI, considered in 29.5% as high and in 28.9% as very high (Table 5).
Figure 1. Diagram of the method used for taking the final valid simple. aIC: Patient inclusion criteria. bLDL-C: Visit with low density lipoprotein cholesterol values available. cCriteria for treatment change: LDL-C >100 without Diabetes, or LDL-C >70 with Diabetes: With no [sic] Side effects: adverse effects resulting from current lipid lowering medication.
In the univariate analysis, significant associations were found that disappeared when the multivariate model was adjusted. This was the case with the following variables: triglycerides (lower levels of triglycerides, higher TI); patient age (greater age, greater TI), patients 55 to 75 years of age in comparison to those <55 years of age had an OR=1.35 (95% CI, 1.14-1.66) and those >75 years of age an OR=1.66 (95% CI, 1.33-2.10). Following a lipid-lowering diet in comparison with not following a lipid-lowering diet had an OR=1.17(1.02-1.35); not receiving lipid-lowering treatment in comparison with receiving 2 or more drugs is a protective factor (OR=0.3; 95% CI, 0.2-0.5), whereas receiving only 1 drug is a risk factor (OR=1.3; 95% CI, 1.1-1.6); number of patients a week ≥50 in comparison with < 50 had an OR=0.79 (95% CI, 0.66-0.96); having received 3 or more courses on dyslipidemia in comparison with fewer than 3, had an OR=0.78 (95% CI, 0.66-0.92).
The OR of the raw data on the association between the other significantly associated variables in the univariate analysis can be seen in Table 6.
No significant association was found between TI and sex. However, when analyzing this factor based on TI severity, there is an association: the percentage of high and very high TI is significantly (P < .05) higher in women (high TI: 35% in women and 27% in men; and very high TI: 34% in women and 26% in men).
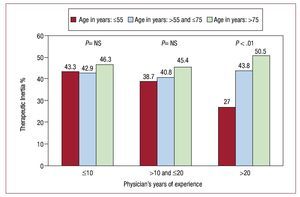
We found a significant association between TI and physician years of experience, and when stratifying by patient age: in young patients (<55), TI decreases as physician experience increases (Figure 2). In diabetics, TI is significantly higher in the LDL-C range of 70-100 mg/dL than in LDL-C >100 mg/dL patients (76.5% vs 34.6%).
Figure 2. Therapeutic inertia (TI) according to patients' age and physicians' years of experience. ns = not significant
On carrying out the logistical regression multivariate analysis and comparing it with the univariate analysis (Table 6), we saw that the greater association with TI corresponded to the visits with levels of total cholesterol ≤200 mg/dL (with medication change criteria). Diabetes, which was a significant risk factor for the univariate TI analysis (P < .001), is no longer a risk factor when adjusted for lipid profile variables (P= .07). High HDL-C levels and low total cholesterol values are shown to be risk factors for TI. A history of stroke, independent of diabetes, reduces TI. In the case of other variables that were significantly associated with TI in the univariate analysis, significance disappears when the multivariate model is adjusted. This is the case for: triglycerides, number of drugs, patient age, diet for dyslipidemia, number of patients/week, courses on dyslipidemia during the last 2 years, when the physician sets a value as a therapeutic target or considers there is undertreatment due to organizational aspects or fear of side effects.
With reference to aspects related to the cardiologist, a lower TI is related to years of experience, with an opinion that the lack of protocols is the cause of undertreatment, with a greater attendance at congresses, and with a greater number of patients with dyslipidemia during consultations. In contrast, when the hours per year of training are at the work center or when the physician considers that the percentage of patients who comply with treatment is greater, there is greater risk of TI (Table 6).
DISCUSSION
Our treatment indicators are better than those of the L-TAP study, which estimated that 82% of patients with dyslipidemia and ischemic cardiopathy did not have LDL-C values within the recommended therapeutic target values,13 but were worse than those seen in another more recent study, also on ischemic cardiopathy, which considered patients with LDL-C and HDL-C were over 50% and 80% respectively, outside the recommended target values.25 A novelty of our study is that it confirms a high proportion of undertreatment associated with TI in the management of dyslipidemia in the area of outpatient cardiology. These data are a cause for concern when many of the participating physicians (83%) recognize a priori that there is undertreatment of dyslipidemia and the majority attend specific training courses.
Another aspect to be highlighted, is the global association of TI and cardiovascular risk. In two thirds of visits TI can be considered high or very high. The GPC underline the need to tighten lipid control in patients at greater risk. However, in our study, diabetes adjusted to LDL-C values becomes a weak protective factor (P = .07), and the other traditional risk factors (hypertension, tobacco smoking, obesity, physical exercise) do not intervene in the decision to intensify treatment. In contrast, the finding that a history of stroke contributes to improve dyslipidemia treatment is extremely interesting: this was supported by the recently published results of the ASCOT study.26
Although when considered as a whole, no association has been seen between TI and sex when analyzing the type of TI, it has been found that high or very high TI is more frequent in women. This finding, confirms the fact that physicians underestimate or undertreat risk factors, which is in agreement with what has been described in relation to the differences seen between sexes in the management of risk factors and ischemic cardiopathy itself.27
In our opinion, the finding of selectively lower TI in young patients cared for by physicians with greater experience, is probably due to the fact that these physicians have a greater understanding of the chronic and recurrent nature of this disease. Length of time of lipid-lowering treatment is a factor that, in our study, is associated with TI, probably due to rejection of treatment changes on the part of the stable patient. However, it is also possible that there is "inertia" on the part of the physician to modify a treatment which proves to be effective over time.
According to our results the values of total cholesterol are considered more important than those of LDL-C when deciding not to change a treatment. Something similar occurs when HDL-C levels are above 40 mg/dL. These findings could be partly justified by a consideration that total cholesterol values have sufficient validity to establish treatment, and on the other hand, by the belief of a greater preventive capacity on the part of that HDL-C is more preventive than has been proven.
It is only logical to believe that hours of training correlate with knowledge and adherence to GPC. When analyzing the attendance at congresses or a greater number of hours per year of training at the work center, we saw that attending congresses reduced TI, while local training has an inverse effect to that expected. This finding could be explained by the fact that physicians with less TI who attend less training at their work center, are those with greater experience, and greater activity and care pressure, but with a greater attendance at congresses. In any case, the reason for this association is not clear.
Most of the physicians in this study recognize that dyslipidemia in patients with ischemic cardiopathy is undertreated, and it is their opinion that this undertreatment can be due to ignorance of the GPC, fear of medication side effects and, in great measure, care overload. However, we have assessed care pressure by means of the number of patients/ week and have not found an association with TI; therefore, it is possible that it is a perception on the part of the physician and not a real cause of undertreatment. It is also noteworthy that less than half of the physicians recognize that there is communication and coordination with primary care; in our opinion, this should lead us to reflect on the organizational model and shows a route of action to improve control of these patients and probably of all chronic cardiovascular conditions.
However, we are sure that there are still factors that have not been considered in this study and that are a cause of TI. Organizational aspects such as duration of visit, lack of motivation or rejection of therapeutic changes by the patients who are stable, among others, are involved in this complex and severe care problem. It would seem evident that the GPC alone do not modify clinical practice with sufficient speed to be appropriate and that strategies must be found to improve knowledge and facilitate care. We should take advantage of the support provided by new technologies as well as the multidisciplinary nature of care. We need support systems for the correct decisions (electronic and/ or paper), population health education, reminder systems, coordination with primary care, and inclusion of these patients as chronic patients in nursing and clinical pharmacology protocols.28-32
Limitations of the Study
The sample of physicians was not randomly taken, but to minimize bias we used several measures: distribution in all communities, letter of invitation from the scientific society, and choice of a retrospective design of consecutive patients (without possibility, therefore, of modifying their habitual practices or prescriptions). The data of our study do not disagree with those described in the literature with reference to lipid levels, treatment using different statins at a national level,33 and risk factors in the population with such as chronic ischemic cardiopathy25,34 (such as a low percentage of patients with ischemic cardiopathy had recommended lipid levels according to the guidelines). We believe this supports the representativity of the sample analyzed.
CONCLUSIONS
Our study confirms the high proportion of TI in the management of dyslipidemia in outpatient cardiology.
When managing lipids in patients with coronary cardiopathy, physicians ignore the existence of other cardiovascular risk factors. Even the presence of diabetes does not lead physicians to clearly and significantly change their therapeutic attitude.
The severity of TI in lipid management in patients with ischemic cardiopathy is greater in women, and overall risk factors are under-estimated.
Physicians continue to be guided by total cholesterol levels or assume that HDL-C level is a preventive measure, and do not follow GPC recommendations when they decide to change treatments.
Only those physicians with greater professional experience closely adhere to GPC, with their younger patients. Attendance at different training activities improves GPC adherence.
Cardiologists recognize the undertreatment of dyslipidemia, and also that there is little communication with primary care in the follow-up of these patients.
ABBREVIATION
COCS: Clinical and Outpatient Cardiology Section
CPG: clinical practice guideline
HDL-C: high-density lipoprotein cholesterol
LDL-C: low-density lipoprotein cholesterol
SD: standard deviation
TI: therapeutic inertia
SEE ARTICLE ON PAGES 1399-401
The INERCIA Study was an initiative of the Outpatient and Clinical Cardiology Department of the Spanish Society of Cardiology.
Financing: Pfizer S.A, Spain
Correspondence: Dra. M.D. Aguilar.
Técnicas Avanzadas de Investigación en Servicios de Salud (TAISS). Cambrils, 49. 28034 Madrid. Spain.
E-mail: daguilar@taiss.com
Received February 11, 2010.
Accepted for publication July 12, 2010.