Keywords
INTRODUCTION
In Japan in 1990, Sato et al1,2 described a syndrome consisting of chest pain, electrocardiographic, and biochemical changes, all similar to those of acute myocardial infarction, and abnormalities of apical left ventricular contractility. The unusual component was the lack of lesions of the coronary vessels and the almost complete resolution of the segmental disorders after a few days or weeks. This syndrome was called "apical ballooning," "tako-tsubo," or transient apical dyskinesia. Of note was the segmental involvement of various coronary territories and the excellent prognosis. Cases were later reported from all over the world and involving all races.3-5
METHODS
We report the first series of consecutive cases in Spain, all with similar symptoms, but with different segmental involvement, who had the same benign course. The patients all had midventricular abnormalities, similar to those recently described.6-10
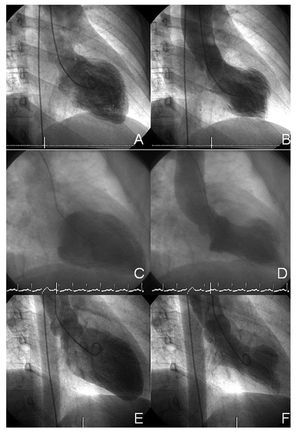
The patients were all Caucasian women, with symptoms compatible with acute coronary syndrome (Table 1); elevation (on serum analysis) of markers of myocardial necrosis; electrocardiographic abnormalities (ST segment elevation >1 mm in 2 leads and/or the appearance of negative T waves in 2 or more leads); left ventricular contractility disorders (severe dyskinesia/akinesia/ hypokinesia) on ventriculography, but with no apical involvement; with no significant coronary vessel abnormalities (obstruction <50% and absence of unstable plaque that might cause the symptoms), with complete recovery of ventricular contractility. Patients with cranioencephalic abnormalities that might have caused the symptoms were excluded. The initial segmental classification was done with ventriculography (Figures 1 and 2), and transthoracic echocardiography was used for the follow-up (Table 2).
Figure 1. Ventriculograms. A and B: case 1. C and D: case 2. E and F: case 3. Diastole is shown on the left (A, C, and E) and systole on the right (B, D, and F).
Figure 2. Ventriculograms. G and H: case 4. I and J: case 5. Diastole is shown on the left (G and I) and systole on the right.
RESULTS
Case 1
A 44-year-old woman who presented dizziness and syncope that lasted just seconds, in relation with a family problem. Because of generalized negative T waves and high troponin I levels coronary arteriography was carried out. No coronary lesions were seen, but anterolateral akinesia and inferior hypokinesia were detected (left ventricular ejection fraction, 32%) with moderate mitral insufficiency. A transthoracic echocardiogram performed 5 days later showed normalization of the earlier findings. Cardiac magnetic resonance imaging before discharge showed no segmental abnormalities or signs of myocarditis.
Case 2
A 62-year-old woman was admitted with increased dyspnea, respiratory infection, and bronchospasm; there were no data suggestive of myocardial involvement. Twenty-four hours later she reported central chest pressure and had ST elevation on the upper lateral surface, as well as raised levels of markers of necrosis. A coronary angiogram showed normal coronary vessels, and a ventriculogram showed anterior dyskinesia with basal hyperkinesia. The follow-up echocardiogram carried out four months later showed normalization of the contractility abnormalities.
Case 3A 52-year-old woman presented to the emergency department with a 3-hour history of typical exertion pain that ceased with nitroglycerin. She had negative T waves and raised troponin I concentrations. A coronary angiogram showed normal coronary vessels and a ventriculogram showed an area of severe hypokinesia localized on the anterolateral surface. The echocardiogram on discharge was normal and the patient remains asymptomatic.
Case 4
A 69-year-old woman, who had had asthma since childhood, peripheral facial palsy, and a history of paroxystic atrial fibrillation, presented to the emergency department with a hypertensive crisis which ceased with no further complications. The following day she reported epigastric oppression accompanied by rapid palpitations and cephalea. Her blood pressure was 180/90 mm Hg. Troponin was raised (2.11 ng/mL). The coronary angiogram showed normal epicardic arteries and the ventriculogram revealed anterior hypokinesia. Following catheterization, the electrocardiogram showed negative T waves in the precordial leads, which were later corrected.
An echocardiogram 5 days after her admission showed no abnormalities. She has since presented with episodes of rapid atrial fibrillation. She has been admitted once, but with no clinical involvement, increase in markers of necrosis or new electrocardiographic abnormalities indicative of ischemia.
Case 5
A 69-year-old woman who had had olivopontocerebellar atrophy for several years presented to the emergency department with a 12-hour history of central chest oppression accompanied by dyspnea. She had ST elevation of 1 mm in leads I and aVL, with later T wave inversion at the same level, and raised markers. Coronary arteriography showed no abnormalities of the coronary tree, with akinesia localized to the anterolateral region with normal apical contractility. An echocardiogram prior to discharge showed no segmental abnormalities.
DISCUSSION
This new variant of transitory dyskinesia is unusual because it does not apparently affect the apex of the left ventricle, unlike the classic form of tako-tsubo. In spite of the little experience with the 2 conditions, it would appear that, as well as sharing a lack of coronary lesions and the distribution of the motility abnormality in various vessels, they both have a benign prognosis with no complications, at least over the short term.7 The incidence of transient apical dyskinesia is unknown, although it could account for 1% of infarctions.3 However, its frequency may be greater but go unnoticed due to its lack of clinical expression. The midventricular variant appears to occur less often.7 Apical dyskinesia occurs predominantly in women,3 whilst Western persons tend to have inverted T waves rather than ST elevation, which is more common in Asian patients.10
Many etiological and pathological mechanisms have been suggested as explanations for these transitory ventricular abnormalities, which can resemble acute myocardial infarction in their clinical, analytical, electrocardiographic, and echocardiographic aspects.3-16
Of note are myocarditis,3,4 non-obstructive plaque rupture with spontaneous thrombolysis, anatomic abnormalities (very long left anterior descending artery),16 and geometric ventricular predisposition14 (gradient with left ventricular outflow tract obstruction), sepsis,15 and the most commonly proposed lately: elevated concentrations of catecholamines and neuropeptides due to stress.13 This latest theory is based on the clinical, anatomical, and pathological association between transitory dyskinesia due to psychic stress (death of a relative) or physical stress (asthma, surgery), and that which is neuromediated in ictus, subarachnoid hemorrhage, cranioencephalic trauma, and pheochromocytoma. The mechanism between sympathic stimulus and myocardial contusion is far from being discerned: spasm of the epicardic coronary vessels, microvascular spasm with reduction of coronary reserve, and endothelial dysfunction, or direct myocardial lesion (calcium overload mediated by cyclic adenosine monophosphate, free radicals).
No conclusive theories yet exist to explain the exclusive abnormality of the midventricular segments. It could reflect the temporal evolution of apical dyskinesia in the process of recovery, although given the haste with which cardiac catheterization was done this hypothesis seems questionable. The low values of the markers of necrosis and the rapid recovery of the patients (4 out of 5 prior to discharge) could suggest that it may be an abortive or attenuated variant of the classical form. Whatever the case, no demographic, clinical, biochemical, or angiographic differences have been noted between this and the classical form, although regional metabolic abnormalities coinciding with abnormalities in motility have been found.7
Currently, no clear therapeutic recommendations exist, and those recommendations available are restricted to the usual management of the complications and propose the use of beta-blockers.
In conclusion, further studies are required to explain the mechanisms associated with this type of involvement and to design efficient diagnostic and therapeutic attitudes.
Correspondence: Dr. I.J. Núñez Gil.
Avda. del Talgo, 83, 1.o E. 28023 Aravaca. Madrid. España.
E-mail: ibnsky@yahoo.es
Received June 26, 2007.
Accepted for publication September 24, 2007.