Despite advances in the treatment of heart failure, mortality, the number of readmissions, and their associated health care costs are very high. Heart failure care models inspired by the chronic care model, also known as heart failure programs or heart failure units, have shown clinical benefits in high-risk patients. However, while traditional heart failure units have focused on patients detected in the outpatient phase, the increasing pressure from hospital admissions is shifting the focus of interest toward multidisciplinary programs that concentrate on transitions of care, particularly between the acute phase and the postdischarge phase. These new integrated care models for heart failure revolve around interventions at the time of transitions of care. They are multidisciplinary and patient-centered, designed to ensure continuity of care, and have been demonstrated to reduce potentially avoidable hospital admissions. Key components of these models are early intervention during the inpatient phase, discharge planning, early postdischarge review and structured follow-up, advanced transition planning, and the involvement of physicians and nurses specialized in heart failure. It is hoped that such models will be progressively implemented across the country.
Keywords
Because of the epidemiological dimensions of heart failure (HF), its clinical complexity, its impact on patients’ quality of life, and the workload that it represents for health care systems with finite resources, this syndrome is one of the greatest health care, organizational, and economic challenges to be faced in the coming years.1–3 Despite undeniable advances in HF treatment and the organization of HF management, in recent years2,4–7 mortality, the number of readmissions, and associated health care costs remain very high.1,3 These data demonstrate the need for further advances in optimizing HF management in the different phases of the continuum of care. Specifically, it has been demonstrated that the transition between hospital discharge and outpatient follow-up is a key stage.8 Although theoretically short, this transition has strong prognostic potential and can affect future episodes of decompensation and early readmissions.8,9 The appropriate management of these transitions is an unmet need in most current chronic HF management programs. In this review, we analyze the key aspects of the transitional care of HF and the features of the programs aimed at improving its management.6,8,10–12
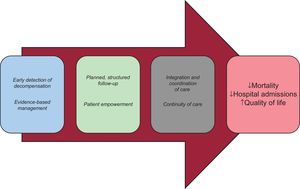
HEART FAILURE UNITS: COMPONENTS AND SCIENTIFIC EVIDENCE FROM THE TRADITIONAL CARE MODELHeart failure care models inspired by the chronic care model are called disease management programs for HF, also known as heart failure programs or heart failure units (HFU).5–7,13 These models aim to reduce mortality and hospital admissions in patients with HF and improve their health-related quality of life (Figure 1). From a theoretical standpoint, these models could promote evidence-based care and reduce variability in health care delivery, thereby helping to raise the bar for quality of care and increase the equity of our healthcare system.4–7,13–15
Within the general framework of HFUs, multiple models of care have been described, ranging from a single educational session before discharge or a single educational home visit by a specialist nurse and regular telephone follow-up to a multidisciplinary intervention centralized in a physical unit, with or without liaison with primary care (PC). Most HFUs combine several of these interventions.4–7,13–16 The widespread implementation of these care models has been favored by the initial results of several analyses and meta-analyses,5,6 which have led to a IA level of recommendation in clinical practice guidelines.17,18 In this type of unit or program, a variety of interventions (education, follow-up, treatment, social support) may be selected from those that have been demonstrated to improve quality of life, reduce the number of HF and all-cause hospital admissions and even reduce mortality.5,6 This reduction in hospital admissions4,14,15,19–21 and improved survival have also been demonstrated in Spain, encouraging the implementation of various HFUs in our country.22
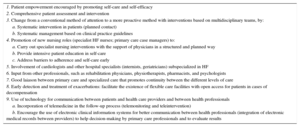
Some more recent studies, however, have failed to demonstrate a clear benefit of these HFUs,23 which has brought into question their structure and even their usefulness. Regarding specific aspects of care, the setting of care (hospital, PC, home), the intensity of interventions, the components and professionals involved in such interventions, and the target population, among other factors, vary widely in both the literature and in clinical practice. A Cochrane review24 that analyzed 25 studies with nearly 6000 patients in total concluded that it was not possible to identify the ideal components of the various interventions (HFUs or other care formats) due to the wide heterogeneity of the distinct models. Despite these limitations, we believe that there are some basic key components that should form the basis of all HF programs or HFUs (Table 1).4–7,17,18
Chronic Care Model and Heart Failure Care Programs: Recommended Compontents4,7,17,18
| 1. Patient empowerment encouraged by promoting self-care and self-efficacy |
| 2. Comprehensive patient assessment and intervention |
| 3. Change from a conventional method of attention to a more proactive method with interventions based on multidisciplinary teams, by: |
| a. Systematic intervention in patients (planned contact) |
| b. Systematic management based on clinical practice guidelines |
| 4. Promotion of new nursing roles (specialist HF nurses; primary care case managers) to: |
| a. Carry out specialist nursing interventions with the support of physicians in a structured and planned way |
| b. Provide intensive patient education in self-care |
| c. Address barriers to adherence and self-care early |
| 5. Involvement of cardiologists and other hospital specialists (internists, geriatricians) subspecialized in HF |
| 6. Input from other professionals, such as rehabilitation physicians, physiotherapists, pharmacists, and psychologists |
| 7. Good laiason between primary care and specialized care that promotes continuity between the different levels of care |
| 8. Early detection and treatment of exacerbations: facilitate the existence of flexible care facilities with open access for patients in cases of decompensation |
| 9. Use of technology for communication between patients and health care providers and between health professionals |
| a. Incorporation of telemedicine in the follow-up process (telemonitoring and teleintervention) |
| b. Encourage the use of electronic clinical information systems for better communication between health professionals (integration of electronic medical records between providers) to help decision-making by primary care professionals and to evaluate results |
HF, heart failure.
Widespread implementation of these integrated care models for patients with HF has been difficult for several reasons. These reasons include the heterogeneity of the models evaluated in clinical trials, the questionable applicability of study results in “real world” clinical practice, and their organizational complexity. In addition, there is wide variability in the organization and delivery of care in chronic patients in each health care area or area covered by a particular hospital, which is determined by the resources available and by organizational dynamics. Therefore, we cannot speak of a “class effect” in these organizational models.4,5,7,16 In this regard, the quality programs launched by the Spanish Society of Cardiology (SEC-Excelente)25 and the Spanish Society of Internal Medicine (UMIPIC)26 aim to establish quality standards in the organization of HF care in Spain.
HEART FAILURE TRANSITIONAL CARE MODELS: WHY?In Spain, between 2003 and 2011, the number of admissions for HF in patients older than 65 years increased by 26%, in a period when the population of persons older than 65 years grew by 13%.2 Hospital admissions for HF have a bimodal distribution and are more frequent at the onset and end of the disease. Approximately one third of all HF patients present with a hospital admission.27 Admitting a patient can be an opportunity to adequately document the diagnosis, make an individualized adjustment to chronic HF treatment, provide the patient with better health education, and develop a follow-up plan.27 A recent population-based study observed that having a recent hospital admission was associated with higher mortality and more readmissions and was an independent predictor of increased health care costs in the following year.1
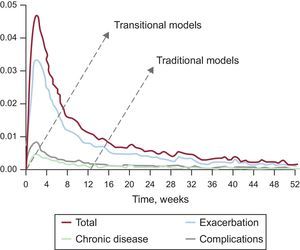
After discharge, rehospitalization rates for HF are fairly high and tend to be concentrated in the first few months following discharge4 (Figure 2).28 In Catalonia in 2005-2014, readmission rates for such patients at 30 days postdischarge were between 14% and 15%, while readmissions at 90 and 180 days were 25% and 30%, respectively.1 In this context, readmissions clinically-related to the prior admission for HF are mostly due to exacerbation of the underlying disease,4 and could be prevented in up to 75% of cases.9 Early readmissions after discharge are strongly linked to the quality of inpatient care and, although they may be due to incomplete patient stabilization, they are often due to poor discharge coordination and the inability to ensure good-quality care early after discharge.8,27 This, along with the readmission patterns shown in Figure 2, mean that the traditional care processes for HF should be redesigned toward a care model that revolves around transitions of care, creating more opportunities for the prevention of rehospitalizations.8
Weekly probability of readmission after a prior hospital admission for HF: all-cause readmission (total), readmission due to a cause clinically-related to HF (recurrence), readmission due to other chronic conditions (chronic diseases) and readmission due to complications of care (complications). Data from the registry of the Minimum Basic Data Set of Acute Care Hospitals in Catalonia from 2010-2011. The arrows indicate the points where the traditional care models are activated compared with transitional care models (which are started before discharge). This representation illustrates marked differences in the opportunities for preventing readmission according to the dominant model. Modified with permission from the Catalan Health Service.28
The recent paradigm shift in the management of chronic diseases is based on the development of a multidisciplinary model that provides integrated care of HF patients throughout the entire disease process, which spans the diagnosis and inpatient phase until discharge to home, with special emphasis on subsequent follow-up and transition of care to different health care settings depending on the progress of the condition.4,8,13,27 New strategies in this field seek to concentrate these clinical management resources and interventions at the times when there is a transition of care between health care professionals. The aim is to achieve a shift from traditional HFUs to multilevel transitional care programs for HF. Data from most studies indicate that a smooth transition in HF patients reduces the rate of potentially avoidable readmissions and decreases the risk of adverse clinical events.8,10–12,29
THE CARE PATHWAY: INITIAL KEY ELEMENTA crucial element is a consensus document, developed jointly by the hospital, PC, and health and social care, that encompasses distinct levels of care (a care pathway).4,8 The document is a combination of protocols and systems agreed upon among professionals that includes the different interventions that should be carried out throughout the patient's process. This document specifies who, where, how, and how often the patient should be reviewed, with the aim of improving the clinical approach by offering the most appropriate care in each situation. It defines who is responsible for the patient's management at each point and when and how that responsibility should be transferred to other professionals (handover), and is based on the care agreement between the professionals involved.4,8
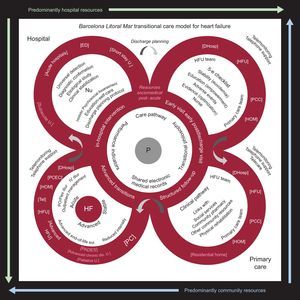
The regional-based integrated care model for patients with HF developed in the Barcelona Litoral Mar Integrated Health Area between Hospital del Mar, PC, and health and social care in this urban area of Barcelona is a good example of the implementation of an integrated, multidisciplinary, patient-centered transitional care program. Previous publications have described the organizational and developmental characteristics and the beneficial outcomes in terms of hospital admission and survival with this care model.4,14,15,30Figure 3 shows the key aspects of this urban-based model that are, in summary: a) starting intervention in the inpatient phase; b) active discharge planning process; c) early review after discharge; d) structured follow-up based on clinical practice guidelines, and e) planning of other advanced transitions.4,8,17,18
Barcelona Litoral Mar transitional care model for heart failure. The central circle represents the core elements needed to put the model into practice, with the patient and the professional at the center (P). The philosophy of transitional care implies integrated, collaborative, early, continuity-based, structured and planned care with contingency plans for emergencies. The content of the circles includes the actions to be carried out; in the outlines of the circles, the ideal care services are specified (in pink, the health and social care resources). DHosp, day hospital dis., disease; diur, diurectis; ED, emergency department; Flex, flexible regimen; IV, intravenous; HOM, home; HF, heart failure; HFU, heart failure unit; Nu, nursing; PADES, home care team and support teams for palliative care; PC, primary care; PCEC, primary care emergency centers; PCC, primary care center; PO, per os; Sol, solutions; Tel, telephone follow-up; U, unit.
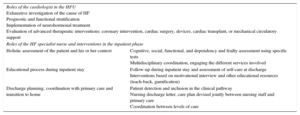
The success of the implementation of a hospital-based HF care process depends on the systematic execution of interventions specified in clinical pathways. Along with physicians, specialist HF nurses (Table 2) are key health care professionals in the HF care process.31
Roles of the Cardiologist and Nurse in a Heart Failure Program During the Inpatient Period4,31
| Roles of the cardiologist in the HFU Exhaustive investigation of the cause of HF Prognostic and functional stratification Implementation of neurohormonal treatment Evaluation of advanced therapeutic interventions: coronary intervention, cardiac surgery, devices, cardiac transplant, or mechanical circulatory support | |
| Roles of the HF specialist nurse and interventions in the inpatient phase | |
| Holistic assessment of the patient and his or her context | Cognitive, social, functional, and dependency and frailty assessment using specific tests Multidisciplinary coordination, engaging the different services involved |
| Educational process during inpatient stay | Follow-up during inpatient stay and assessment of self-care at discharge Interventions based on motivational interview and other educational resources (teach-back, gamification) |
| Discharge planning, coordination with primary care and transition to home | Patient detection and inclusion in the clinical pathway Nursing discharge letter, care plan devised jointly between nursing staff and primary care Coordination between levels of care |
HF, heart failure; HFU, heart failure unit.
For a comprehensive assessment and integrated intervention process to be successful, HF programs with a functional structure are needed (Table 1). These units must have team members in all areas that could admit HF patients, so that they may be identified and included in the HF care pathway and included in the HF management care pathway in each area.31 Clinical information systems can be useful for this detection. The units involve cardiology, emergency medicine, internal medicine, acute geriatric units, emergency department short-stay units, and subacute units, among others.4,22,32 In all these areas, it is crucial to have: a) confirmation of the HF diagnosis based on clinical criteria and use of biomarkers,17,18 and b) active involvement in the care pathway and the discharge planning process, aspects that still have a wide margin for improvement in our health care systems.32
A comprehensive psychosocial assessment of the patient by a nurse is considered one of the key strategies in HF programs4,8,17,18 and should be started in the first 24hours of the inpatient stay. The nurse coordinator for the inpatient HF process liaises with the different services involved (neuropsychology, rehabilitation, geriatrics, etc) and the core components of cardiology and internal medicine that form HFUs.4,8,15 The nurse implements the key actions described in Figure 3 and, in particular, coordinates hospital discharge. Early intervention in these aspects aims to pave the way for an early functional recovery, improve self-care as early as possible, identify the main caregiver, correctly plan the patient's discharge, and minimize the risk of readmission. Coordination with social work services will sometimes be necessary to overcome social barriers that may interfere with the achievement of clinical goals and the patient's aims.4,8,14,15,29,31 In this transition, health and social resources may be required (Figure 3).
In patients admitted with HF, diagnosis and the medical management plan should be done by physicians specialized in HF. Cardiologists specialized in HF must play a significant role in these processes, whether directly on the cardiology ward or by providing support to other medical specialties31,33 in specific hospital units for frail patients, where the cardiologist should be available for consultation. In addition, a holistic view of the patient is fundamental in any type of multidisciplinary structure, whether led by cardiologists or internists. This is a defining aspect in the organizational model proposed in the UMIPIC program by the Spanish Society of Internal Medicine, through the creation of integrated management units for patients with HF and multiple comorbidities. The initial implementation of these units has produced a highly significant reduction in hospital readmissions for this type of patient.26
Discharge Planning and Transition of CareContinuity of care in HF requires different professionals, in distinct clinical settings (multilevel), and at different times, to establish a shared view of the care required with a common focus: the patient.4,8,14,15,29,30
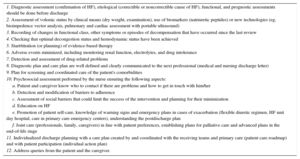
The effectiveness of integrated, multidisciplinary, patient-centered HF care programs focusing on transitions of care8,15 largely depends on: a) adequate discharge planning; b) the patient meeting stability criteria before discharge; c) evaluation that quality of care objectives are met by using checklists before and after discharge (Table 3); and d) adequate information transfer to the health care professional who will take the lead at follow-up (Tables 3 and 4).4,8,14,15
Checklist of the Actions That Should be Carried out Before Discharge, at the First Early Review After Discharge and in Subsequent Visits for Patients With Heart Failure4,8,17,18
| 1. Diagnostic assessment (confirmation of HF), etiological (correctible or noncorrectible cause of HF), functional, and prognostic assessments should be done before discharge |
| 2. Assessment of volemic status by clinical means (dry weight, examination), use of biomarkers (natriuretic peptides) or new technologies (eg, bioimpedence vector analysis, pulmonary and cardiac assessment with portable ultrasound) |
| 3. Recording of changes in functional class, other symptoms or episodes of decompensation that have occurred since the last review |
| 4. Checking that optimal decongestion status and hemodynamic status have been achieved |
| 5. Start/titration (or planning) of evidence-based therapy |
| 6. Adverse events minimized, including monitoring renal function, electrolytes, and drug intolerance |
| 7. Detection and assessment of drug-related problems |
| 8. Diagnostic plan and care plan are well defined and clearly communicated to the next professional (medical and nursing discharge letter) |
| 9. Plan for screening and coordinated care of the patient's comorbidities |
| 10. Psychosocial assessment performed by the nurse ensuring the following aspects: |
| a. Patient and caregiver know who to contact if there are problems and how to get in touch with him/her |
| b. Detection and modification of barriers to adherence |
| c. Assessment of social barriers that could limit the success of the intervention and planning for their minimization |
| d. Education on HF |
| e. Promotion of patient self-care, knowledge of warning signs and emergency plans in cases of exacerbation (flexible diuretic regimen, HF unit day hospital, care in primary care emergency centers), understanding the postdischarge plan |
| f. Joint care (professionals, family, caregivers) in line with patient preferences, establishing plans for palliative care and advanced plans in the end-of-life stage |
| 11. Individualized discharge planning with a care plan created by and coordinated with the receiving teams and primary care (patient care roadmap) and with patient participation (individual action plan) |
| 12. Address queries from the patient and the caregiver. |
HF, heart failure.
Contents of Heart Failure Nurse Discharge Letter4
| Interventions performed (educational, social, and functional) and goals achieved |
| Interventions pending for the next level of care (blood test, titration of medications) |
| Presence of complexity criteria |
| Discharge status (functional class, weight) |
| Follow-up method at discharge and communication channels with contact with the hospital HF unit |
HF, heart failure.
The defining elements transitional care in the Barcelona Litoral Mar model (Figure 3)4 are: a) nurse-led coordination of the in-hospital intervention; b) systematic in-hospital intervention by members of the multidisciplinary HF program (acute beds assigned to the HF program), and c) planning of discharge and transfer to home, based on in-person meetings between the in-hospital and community health care professionals in a discharge coordination session. This meeting is held weekly and carried out in the hospital setting between hospital HF professionals and the PC nurse case managers.4 It allows an appropriate integrated intervention to be designed for each patient admitted with HF (roadmap), taking advantage of the physical proximity and the opinion of each of the professionals involved in his or her management (HFU and PC multidisciplinary team).
EARLY FOLLOW-UP AFTER DISCHARGE AND TRANSITION OF CAREEarly follow-up after discharge is an essential step in the success of the transition from the acute phase to long-term outpatient management. Most HF programs8,18 include a follow-up visit after discharge, which ideally should be done in the first 7 to 10 days. The contents of the first postdischarge visit should be well defined and are summarized in Table 3. It is also important to define in which cases an even earlier contact (24-48 hours) could be helpful, whether in-person (in the clinic or at home) or by telephone. Some models include these earlier contacts.4,8,15,18
This intervention (Figure 3, right upper circle) can be conducted in the outpatient or inpatient setting (HFU), either in-person (at home, primary care center, HFU clinic, day hospital) or remotely (telemedicine). A systematic assessment using checklists allows the nurse to check that the patient is euvolemic, reinforce the knowledge required for good self-care, detect adverse events (clinical, hemodynamic, renal, or electrolyte deterioration), prevent drug-related problems by means of drug reconciliation, and lay the foundation for treatment optimization according to the scientific evidence (Table 3 and Figure 3).
In this regard, many transitional care programs incorporate a postdischarge follow-up call. This can be done at different points and with different aims: an early postdischarge call as a bridging intervention to maintain a safe transition and/or follow-up calls to ensure continuity of care after hospitalization, improve treatment adherence, and reduce hospital readmissions.4,8,15,16
Continuing the education process is another basic element in transitional care. The aim of the intensive educational intervention is to improve the 3 aspects of self-care: maintenance (diet, exercise, and medications), monitoring (daily evaluation to detect deterioration), and self-management (appropriate responses to problems such as warning signs and use of a flexible diuretics regimen).4,6,8,29 Educational materials (paper or electronic support), as well as group or motivational interventions, can be of help on this matter.
A medication review and drug reconciliation at the first postdischarge follow-up allow assessment of treatment adherence and the detection of drug-related problems, whether by nurses or pharmacists involved in the program. In some regions, shared electronic prescription is available: this is undoubtedly a very useful tool for treatment reconciliation.4,6,8,29
Last, health care access is highly important in these patients to ensure the equity in care delivery implicit in a system with universal coverage and to guarantee a rapid response to contingencies. Thus, in cases of early decompensation, patients must have immediate access to health care professionals. The implementation of an open-access day hospital dedicated to HF or telemonitoring follow-up could be useful for this purpose.4,8,15
A recent meta-analysis29 that analyzed the impact of discharge planning for patients with HF showed a relative risk reduction for HF and all-cause readmission of 32% and 15%, respectively, compared with conventional care. Models of early postdischarge home follow-up and those combining different follow-up methods (hospital clinic, home visit, or telephone) are the most efficient in reducing readmissions.
In Spain, the HFU of the Hospital Universitario Germans Trias i Pujol in Badalona demonstrated that a specific multidisciplinary support program after discharge with early follow-up for complex patients with HF allowed a relative reduction of > 40% in readmissions for clinically-related causes.34
In addition, the Barcelona Litoral Mar HF care model includes early postdischarge follow-up (< 7 days) for all patients.4 In this care model, a home-based postdischarge transitional intervention was designed for chronic complex HF patients, in whom frailty is a dominant factor.4,30 In this intervention, PC nurse case managers physically attend the hospital to: a) liaise with the in-hospital HF team to produce a discharge plan while the patient is still admitted; b) coordinate the discharge with the PC team; c) carry out (or advocate) an early postdischarge home visit in the first 48hours, and d) support the PC team in patient follow-up over for the first 3 months after discharge using a clinical pathway.4 A pragmatic assessment of this intervention showed, in comparison with usual care, a significant reduction in readmissions for HF (risk ratio [RR] = 0.4; 95% confidence interval [95%CI], 0.2-0.8; P = .02), all-cause readmissions (RR = 0.4; 95%CI, 0.2-0.8; P = .009), and all-cause mortality (RR = 0.3; 95%CI, 0.1-0.9; P = .03). It also showed a marginally nonsignificant relative reduction of 24.1% in direct costs estimated with full-costing allocation methods (P=.07) in favor of the patient group receiving this transitional intervention.30
POSTDISCHARGE MANAGEMENT: STRUCTURED FOLLOW-UPAfter the early postdischarge contact, patients should be included in management programs that ensure a structured and planned follow-up based on specific detailed clinical pathways that ensure evidence-based intervention.8,11,12 This follow-up should be based on nurses with specialized training in HF, either in the hospital (HF nurses) or the community setting (case managers), with the support of the HF specialist and in coordination with their PC team members.4,8
The concept of transitional care includes a wide range of interventions in terms of intensity (Table 5)12 and content.8,10–12 A recent meta-analysis that included 41 studies12 analyzed the impact of different transitional care interventions on rehospitalizations and emergency department visits. These interventions included patient education prior to discharge (in the management of HF, nonpharmacological strategies and medication management, normally done by a specialist HF nurse using written educational materials or videos), a discharge plan (including a medication review, the development of a personalized care plan, and a discharge report sent to the family physician or cardiologist), and a scheduled, structured, proactive follow-up. This meta-analysis demonstrated that transitional interventions after discharge significantly reduce the risk of readmission and emergency department visits by 8% and 29%, respectively (RR = 0.92; 95%CI, 0.87-0.98; P = .006, and RR = 0.71; 95%CI, 0.5-11.0; P = .04). High-intensity interventions reduced the risk of readmission independently of the duration of the intervention in all patients, but especially in those older than 75 years. Moderate-intensity transitional interventions were effective only if they were implemented for at least 6 months. In contrast, low-intensity interventions were not effective.12 Similar results have been observed in other studies8,10,11 that also reported an improvement in survival with these interventions.
Classification of Intensity of Transitional Interventions12
| Intensity | Components |
|---|---|
| Low | Structured telephone follow-up without home visits, or regular follow-up in the clinic without home visits |
| Moderate | Home visits alone, or a combination of telephone follow-up and regular follow-up in outpatients without home visits, or telemonitoring (telemedicine) without planned patient visits |
| High | A combination of home visits with other types of follow-up (telephone and/or clinic) or telemonitoring (telemedicine) combined with planned patient visits (eg, home visits, telephone follow-up, videoconferences) |
Patients with chronic diseases such as HF require an integrated approach to their care using robust clinical pathways with well-defined objectives, ranging from the diagnostic approach to end-of-life care. Structured follow-up after a hospital admission is a key point in the patient process,4,13 with the goals of promoting patient empowerment and changing professionals’ actions from a conventional to a proactive approach with nursing-based interventions.4,8,13 Structured follow-up after discharge allows systematic application of interventions to reduce variability in clinical practice (Table 3), but must be planned according to the patient's characteristics. According to the Barcelona Litoral Mar model,4 in the hospital discharge planning process, 2 different clinical pathways are defined for structured postdischarge follow-up: a) home-based structured follow-up (face-to-face, telephone, and PC clinic) led by PC case manager nurses,4,30 and b) combined structured follow-up (at home, HFU clinic-day hospital, telemedicine) led by specialist HF nurses assigned to the HFU (hospital-based).4,15 The level of detail and the complexity of the cardiological interventions is greater for patients selected for the clinical pathway led by hospital-based nurses and therefore it includes patients at higher risk of readmission due to exacerbation of this condition. For patients with significant frailty and dependence, inclusion in the PC-based clinical pathway is encouraged: the holistic approach plays a major role in this setting. Details have been published of these clinical pathways and their favorable results in terms of reducing mortality, rehospitalizations, and health care costs.4,15,30
Structured Follow-up in Specialized Heart Failure Units: The Role of TelemedicineIn the HF care process focused on transitions of care, there are potential advantages of using telemedicine. Firstly, it allows remote monitoring of biological markers and/or symptoms to enable the early detection and monitoring of decompensation and other clinical events that would otherwise lead to readmission; secondly, it establishes a channel of communication with patients from their home to conduct structured follow-up after discharge, whether by telephone calls or videoconference.15,16
Trials assessing the efficacy of structured follow-up (telephone) or telemonitoring have shown mixed results. Overall, they have shown positive results in improving survival, reducing hospital admissions, and improving quality of life15,16,35; however, 2 large randomized controlled trials have shown neutral results.36,37 This may explain why clinical practice guidelines currently do not make specific recommendations on the use of telemedicine in HF.17,18
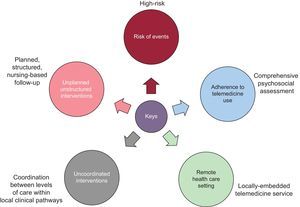
In Spain, there have been several experiences with the use of telemedicine in the field of HF. A clinical study assessed a platform for telemonitoring and the promotion of self-care in the HFU of Hospital Universitario Germans Trias i Pujol. Favorable results were observed, with a reduction of hospital admissions, particularly with the use of telemonitoring of these patients.38 In this setting, in the Hospital del Mar HF program (Barcelona), a telemedicine platform was developed (telemonitoring and teleintervention with videoconference) for the follow-up of patients with HF deemed at high-risk at the time of discharge. The efficacy of this platform was subsequently assessed in a randomized clinical trial.15 The trial showed a significant relative reduction of 61% for admissions due to HF and 45% for health care costs in favor of the group followed-up with telemedicine.15 There are multiple key factors for facilitating the successful implementation of telemedicine in the care process of HF patients, which are summarized in Figure 4.4,16,35–37 Given these findings, the Barcelona Litoral Mar HF program has incorporated telemedicine as part of its standard protocol in the transition of care at discharge for patients at high risk of readmission.4
Key Aspects in Community-based Structured Follow-up After Discharge: Integration With Primary CareIntegrated health care is based on a holistic view of the health care system with a population-based approach, based on the coordination of services and patient-centered care.13 Due to its accessibility and all-round knowledge of the patient, the PC setting is the ideal place for the treatment and follow-up of HF patients as part of the provision of continuity of care coordinated with hospital-based HFU. Data from clinical trials and pragmatic studies show that this component of integration clearly improves outcomes.30,39,40Table 6 summarizes the most important aspects to take into account for the integration of care between HFUs and PC.
Integration of Care for Patients With Heart Failure Between Levels of Care4
| Key actions for the integration of levels of care between the hospital HFU and primary care |
| • Provide support for the diagnostic process and the initial management of patients with suspected HF in the primary care setting |
| • Maintain open, 2-way communication between the 2 levels of care |
| • Support from the HFU in the management of low-risk or moderate-risk patients in the primary care setting |
| • Provide quality care to high-risk patients who would not benefit from specialized follow-up in the HFU hospital setting |
| • Maintain an open channel of communication with high-risk patients followed-up in the hospital unit |
| Points for assessment in the monitoring of HF patients followed-up in primary care |
| • Functional class |
| • Knowledge of warning signs |
| • Patient knowledge about what to do if warning signs occur |
| • Adherence to daily weight monitoring |
| • Treatment adherence |
| • Fluid restriction |
| • Adherence to recommended diet |
| • Adherence to recommended exercise |
| • Understanding of the flexible diuretic regimen |
HF, heart failure; HFU, heart failure unit.
The process of structured PC follow-up must enable the early detection of decompensations and therapeutic optimization of patients and should be based on a specific clinical pathway, early follow-up after discharge,8 and delivery of care that is predominantly (but not exclusively) home-based and led by case manager nurses working together with the patient's PC team (PC cardiologist, nursing and family medicine).4,30,39,40 In our context, this approach is close to the British Model of HF care in PC, based on Community Heart Failure Services.40 This type of PC_led intervention can reduce HF and all-cause readmissions for HF after a recent hospital admission.4,24,30,39,40 This type of interventions should be developed in clinical pathways that include the actions proposed in Tables 3 and 6.4,8 This care process can also be applied to high-risk patients with no prior admissions, who can be identified in PC. This constitutes per se a transition of care that should be encouraged.4,15,30
POSTDISCHARGE MANAGEMENT: ADVANCED TRANSITIONSStructured postdischarge follow-up should consider the key moments at which new transitions of care could or should occur that, unless coordinated properly, could mean another readmission. The incorporation of checklists in the clinical pathways helps to facilitate their effective execution.4,8 These transitions, called advanced transitions, are summarized below.
Transfer to Primary Care-based ManagementOnce the prespecified treatment goals have been met and the risk of readmission has been reduced, care management can be transferred from outpatient hospital HFU-based structured follow-up to the PC team (family physician, family nurse, case manager, and PC cardiologist).4 Importantly, this phase should be based on active communication to highlight completed actions and pending interventions regarding education and self-care issues (including barriers to adherence), HF-related factors, comorbidities, social barriers, and steps that can be taken by the health professional if there is further deterioration.8
Transitions of Care in Patients with Acute Exacerbation (Decompensation): Alternatives to Conventional Urgent AdmissionOne of the hallmarks of transitional care models is the priority given to preventing reshospitalizations.8Table 7 and Figure 3 show the key elements and the health care resources proposed in the Barcelona Litoral Mar HF care model as alternatives to conventional admission in cases of exacerbation.4 During exacerbations, decongestion can be achieved in the outpatient setting by escalating oral diuretic doses or by using intravenous diuretics in intravenous diuretic therapy units in PC or in the HFU day hospital. In refractory cases, elective hospital admission in health and social care units (subacute units) or in acute care beds may allow the achievement of prolonged periods of stabilization not attainable by other means. The importance of telemedicine should be highlighted in several of the steps that define this care model.
Key Elements and Care Resources for Transitions in Cases of Acute Exacerbation of Heart Failure According to the Barcelona Litoral Mar Model of Care4
| Key actions |
| • Inclusion in the care pathway of a clear description of the action to be taken in cases of decompensation both in hospital and in primary care |
| • Consensus on the criteria and the care pathway for the decompensated patient within the integrated program |
| • Definition of a specific clinical pathway for patients who, after structured follow-up, continue to be at high risk of rehospitalization, which allows identification of patients for end-of-life care or candidates for advanced cardiological therapies |
| Heath area services portfolio within the integrated HF program: alternatives to hospital admission |
| • Assessment and treatment through open access and by referral from HF care pathway leaders if there are exacerbations |
| • Outpatient treatment of decompensation with adjustment of oral therapy or intravenous furosemide without admission |
| • Elective admission to health and social units (subacute units) with discharge planning for reinclusion in the care pathway |
| • Elective admission of refractory patients who are not candidates for advanced cardiac therapies in end-of-life units (long-stay health and social centers with the possibility of providing parenteral therapies) |
| • Support from the HF specialist in decision-making on patients hospitalized in alternative units to conventional hospitalization |
| • Prevention of acute exacerbations in patients with refractory or recurrent congestion including renal replacement therapy (peritoneal dialysis) and intermittent inotropic support program with inodilators and/or use of telemonitoring |
| Care settings and resources |
| • Hospital resource: HFU day hospital |
| • Primary care resource: primary care emergency centers |
| • Health and social care resources: subacute units, end-of-life units |
HF, heart failure; HFU, heart failure unit.
Finally, it is important to recognize that some acute admissions to acute care beds may be unavoidable. In some cases, elective admission enables patient stabilization by intensifying treatment in a way that can only be done in hospital, thus ensuring longer periods of stability.27
Transition Toward Advanced Heart Failure UnitsAdvanced HF is defined as HF that is refractory to conventional treatment such as neurohormonal drugs and devices.17,18 Some patients with advanced HF require additional complex therapies, such as device implantation, or other advanced solutions, such as cardiac transplant or mechanical circulatory support. To identify such patients, prognostic and functional assessment during a structured follow-up is essential. The clinical pathways must specify the criteria and mechanisms to facilitate early transfer of the care of such patients to advanced HF teams or units, to receive these therapies.4,18
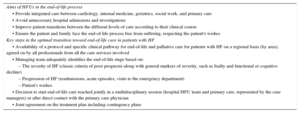
Transition Toward End-of-life CareIn patients with advanced HF, hospital readmission increase between 1 and 2 months before death. The strategies that reduce the risk of readmission in the early stages of the disease may not be effective for patients who have progressed to this advanced stage, which can occur despite optimal therapy and good self-care.27 A significant number of these patients will not be candidates for solutions such as cardiac transplant or mechanical circulatory support. The goals and key elements to ensure an optimal approach in this critical phase, which prioritizes end-of-life care, are summarized in Table 8. At this disease stage, some integrated care models propose home-based care (when family support is adequate), led by the PC team with additional input from palliative care teams.4,41 For patients with poor symptom control and/or suboptimal family support, admission to a health and social care setting should be considered (end-of-life units, long-stay units).41,42 Such units are well prepared to provide mid-term support at this stage, and allow these patients to be admitted to general acute beds. If patients require hospitalization at the end of life, direct admission to a palliative care unit is desirable. This whole process requires a redesign of end-of-life care in each health care area, based on an agreement between health care providers and should be defined in the care pathway.4,42
Transition of Care in End-of-life Phases4,17,18,41
| Aims of HFUs in the end-of-life process |
| • Provide integrated care between cardiology, internal medicine, geriatrics, social work, and primary care |
| • Avoid unnecessary hospital admissions and investigations |
| • Improve patient transitions between the different levels of care according to their clinical course |
| • Ensure the patient and family face the end-of-life process free from suffering, respecting the patient's wishes |
| Key steps in the optimal transition toward end-of-life care in patients with HF |
| • Availability of a protocol and specific clinical pathway for end-of-life and palliative care for patients with HF on a regional basis (by area), agreed on by all professionals from all the care services involved |
| • Managing team adequately identifies the end-of-life stage based on: |
| – The severity of HF (classic criteria of poor prognosis along with general markers of severity, such as frailty and functional or cognitive decline) |
| – Progression of HF (readmissions, acute episodes, visits to the emergency department) |
| – Patient's wishes |
| • Decision to start end-of-life care reached jointly in a multidisciplinary session (hospital HFU team and primary care, represented by the case managers) or after direct contact with the primary care physician |
| • Joint agreement on the treatment plan including contingency plans |
HF, heart failure; HFU, heart failure unit.
Care management programs for HF have traditionally focused on patients with chronic HF at high risk of readmission detected during their outpatient phase. The growing pressure from hospital readmissions in HF patients is shifting the focus of interest from traditional outpatient HF care in conventional HFUs toward multidisciplinary management programs focused on transitions of care, especially between the acute phase and the postdischarge phase. This has led to the application of multidisciplinary, patient-centered, integrated transitional care programs. These HF care models concentrating on transitions of care are based on a holistic assessment of patients during their inpatient stay, identification of specific needs, the discharge planning process, and an early, structured follow-up after discharge that includes advanced care transitions.
CONFLICTS OF INTERESTNone declared.