Current guidelines recommend centralizing the care of patients with cardiogenic shock in high-volume centers. The aim of this study was to assess the association between hospital characteristics, including the availability of an intensive cardiac care unit, and outcomes in patients with ST-segment elevation myocardial infarction (STEMI)-related cardiogenic shock (CS).
MethodsDischarge episodes with a diagnosis of STEMI-related CS between 2003 and 2015 were selected from the Minimum Data Set of the Spanish National Health System. Centers were classified according to the availability of a cardiology department, catheterization laboratory, cardiac surgery department, and intensive cardiac care unit. The main outcome measured was in-hospital mortality.
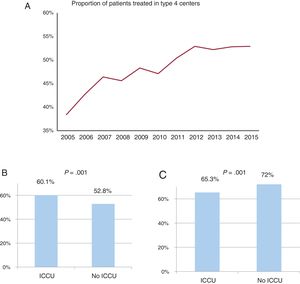
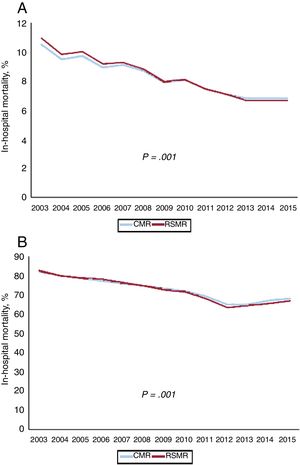
ResultsA total of 19 963 episodes were identified. The mean age was 73.4±11.8 years. The proportion of patients with CS treated at hospitals with a catheterization laboratory and cardiac surgery department increased from 38.4% in 2005 to 52.9% in 2015 (P <.005). Crude- and risk-adjusted mortality rates decreased over time, from 82% to 67.1%, and from 82.7% to 66.8%, respectively (both P <.001). Coronary revascularization, either percutaneous or coronary artery bypass grafting, was independently associated with a lower mortality risk (OR, 0.29 and 0.25; both P <.001, respectively). Intensive cardiac care unit availability was associated with lower adjusted mortality rates (65.3%±7.9 vs 72±11.7; P <.001).
ConclusionsThe proportion of patients with STEMI-related CS treated at highly specialized centers increased while mortality decreased during the study period. Better outcomes were associated with the increased performance of revascularization procedures and access to intensive cardiac care units over time.
Keywords
Cardiogenic shock (CS) is a state of severe hypoperfusion due to cardiac dysfunction that commonly leads to multiorgan failure. This diagnosis accounts for approximately 5% of admissions to general intensive care units, and its incidence has increased during the last few years.1 Despite the widespread use of revascularization in patients with ST-segment elevation acute myocardial infarction (STEMI) and other therapeutic advances in the management of critically-ill patients, in-hospital mortality due to CS remains very high (40%-50% in most series).2–4 Furthermore, mortality may change according to the volume of treating centers and the experience of medical teams.5 Current guidelines recommend centralizing the care of these patients in high-volume centers, with 24/7 availability of the catheterization laboratory (cathlab), and short-term mechanical circulatory support.6
Significant heterogeneity has been reported in the management of CS. To the best of our knowledge, no study has assessed the impact of (hospital departments) where patients are treated, and the structure and organization of treating centers on clinical outcomes in this clinical scenario.
The aims of this study were the following: a) To describe the temporal trends in management patterns and outcomes in patients with STEMI-related CS; b) to characterize the type of treating centers where STEMI-related CS patients are admitted throughout the Spanish National Health System (SNHS), and c) to assess the potential association between changing patterns of care and in-hospital mortality.
MethodsData source, population, and designWe performed an observational retrospective study of patients hospitalized for STEMI-related CS. Anonymous standard data were obtained from the minimum data set (MDS), an administrative database that includes both demographic and clinical information of all patients discharged (alive or dead) from all public hospitals affiliated to the SNHS, which covers 98.4% of the Spanish population. Information includes age, sex, length of stay, type of hospital information, primary discharge diagnosis, up to 13 secondary diagnoses, and 20 procedures performed during hospitalization, all coded according to the ICD-9-CM (International Classification of Diseases-9th Revision-Clinical Modification).7 The quality of these data for the study of acute coronary syndrome has been previously validated.8 The inclusion of this information in the MDS is mandatory for all hospitals in the SNHS.
The study population included patients aged between 35 and 94 years who were discharged (dead or alive) between January 1, 2003 and December 31, 2015 from SNHS hospitals with a principal or secondary diagnostic code of STEMI (410.1, except 410.71) and a principal or secondary diagnostic code of CS (785.51) (CS-STEMI). The comparison group consisted of patients with STEMI without CS (non–CS-STEMI) during the same period. Percutaneous coronary intervention (PCI) was identified by ICD-CM procedure codes 00.66, 36.01, 36.02, 36.05, 36.06 and 36.07 and coronary artery bypass grafting (CABG) by codes 36.10-36.19.
To improve data consistency and quality, episodes with discharge to home in less than 1 day, discharge against medical advice, or unknown discharge destination were excluded, as well as those classified within the major diagnostic category 14 (pregnancy, childbirth, and puerperium) of the All-Patient Refined Diagnosis-Related Groups. Discharges to other hospitals were only excluded when it was not possible to identify the destination hospital. Clinical results in transferred patients were assigned to the center finally discharging the patient.
The main clinical outcome measure was all-cause, in-hospital mortality. We analyzed the association between mortality and the availability of cardiology-related resources (cath lab, cardiac surgery department, and intensive cardiac care unit [ICCU]) in the hospitals attending the included patients.
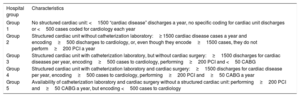
Hospital characteristicsHospitals were classified according to the availability of cardiology-related resources using the RECALCAR criteria9 (table 1). This information was available for the period 2005 to 2015. The absolute number of centers of each type by year is shown in . For the purpose of this study, the few centers with a cath lab and cardiac surgery facilities but in which patients were not directly assigned to cardiology departments (type 5) were not included.
RECALCAR criteria for classifying the different types of center
| Hospital group | Characteristics |
|---|---|
| Group 1 | No structured cardiac unit: <1500 “cardiac disease” discharges a year, no specific coding for cardiac unit discharges or <500 cases coded for cardiology each year |
| Group 2 | Structured cardiac unit without catheterization laboratory:≥ 1500 cardiac disease cases a year and encoding≥500 discharges to cardiology, or, even though they encode≥1500 cases, they do not perform≥200 PCI a year |
| Group 3 | Structured cardiac unit with catheterization laboratory, but without cardiac surgery:≥1500 discharges for cardiac diseases per year, encoding≥500 cases to cardiology, performing≥200 PCI and <50 CABG |
| Group 4 | Structured cardiac unit with catheterization laboratory and cardiac surgery:≥1500 discharges for cardiac disease per year, encoding≥500 cases to cardiology, performing≥200 PCI and≥50 CABG a year |
| Group 5 | Availability of catheterization laboratory and cardiac surgery without a structured cardiac unit: performing≥200 PCI and≥50 CABG a year, but encoding <500 cases to cardiology |
CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention.
Additionally, the availability of an ICCU was obtained from the survey conducted by the Working Group on Ischemic Heart Disease and Acute Cardiovascular Care of the Spanish Society of Cardiology10 (). The requirements for the qualification as an ICCU included: a) comprehensive critically-ill patient management capability, including those requiring invasive mechanical ventilation, and b) administrative adscription of the ICCU to the cardiology department.
Statistical analysisContinuous variables are expressed as mean±standard deviation or median [IQR]. Categorical variables are expressed as number (%). The risk-standardized in-hospital mortality ratio (RSMR) was defined as the ratio between predicted mortality (which individually considers the performance of the hospital attending the patient) and expected mortality (which considers a standard performance according to the average of all hospitals) multiplied by the crude mortality rate. If the RSMR from one hospital is higher than the crude mortality rate, the risk of death in that center is higher than the mean risk of all the hospitals. The RSMR was calculated using multilevel risk adjustment models developed by the Medicare and Medicaid Services,11 adapted to the structure of the MDS database, considering both inter-hospital variability and clinical and demographic variables.12–14 Secondary diagnoses were included in groups of risk factors as described by Pope,15 updated each year by the Agency for Health Research and Quality and including the Charlson I index in the risk factor analysis.16,17 In the adjustment model, we included only comorbidities with an OR> 1. All factors entered into the final model and their coefficients were calculated from our data. Levels of significance for selecting and eliminating risk factors were P <.05 and P ≥ .10, respectively.
Calibration of models was assessed by calculating risk tertiles of the observed and expected in-hospital mortality obtained by the logistic multilevel model. To evaluate the goodness-of- fit, we tested for a significant decrease in the statistical likelihood ratio test compared with the null model. Discrimination of the models was assessed by calculating the receiver operating characteristics curves and their corresponding area under the curve (AUROC). The RSMR was used to compare outcomes between hospitals with different characteristics according to the availability of the cardiology-related resources. The association between in-hospital mortality and hospital characteristics was analyzed by considering the performance of PCI and CABG during the hospitalization episode or the existence of an ICCU as independent variables in the multilevel logistic regression models or by the Student t test or ANOVA test, when appropriate. The analysis of the impact of ICCU on mortality was performed taking into account only type 3 and type 4 hospitals.9
Temporal trends for in-hospital mortality during the observed period were modeled using Poisson regression analysis with year as the only independent variable. In all models, incidence rate ratios (IRR) and their 95% confidence intervals (95%CI) were calculated. All contrasts were bilateral, and differences were considered significant when P <.05. Odds ratios and their corresponding 95%CI were also calculated. All analyses were performed with Stata 13.0 (Stata Corp., College Station, Texas, United States) and SPSS. 20.
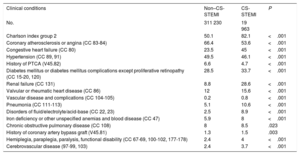
ResultsA total of 392 169 STEMI episodes were identified during the study period (2003-2015), of which 60 976 (15.5%) were excluded because they did not meet the inclusion criteria (not mutually exclusive). A total of 19 963 (6.03%) of the remaining 331 193 episodes were STEMI-related CS. The proportion of women was 28.8% for non–CS-STEMI and 38.8% for CS-STEMI (P <.001). The mean age was 67.2±13.8 years for non–CS-STEMI and 73.4±11.8 years for CS-STEMI (P <.001). The CS-STEMI group showed a higher degree of comorbidity than the non–CS-STEMI group (Charlson index ≥ 3 points 82.1% vs 50.1%, P <.001), except for cardiovascular disease-related comorbidities (table 2).
Comorbidities of patients with non–CS-STEMI and CS-STEMI
| Clinical conditions | Non–CS-STEMI | CS-STEMI | P |
|---|---|---|---|
| No. | 311 230 | 19 963 | |
| Charlson index group 2 | 50.1 | 82.1 | <.001 |
| Coronary atherosclerosis or angina (CC 83-84) | 66.4 | 53.6 | <.001 |
| Congestive heart failure (CC 80) | 23.5 | 45 | <.001 |
| Hypertension (CC 89, 91) | 49.5 | 46.1 | <.001 |
| History of PTCA (V45.82) | 6.6 | 4.7 | <.001 |
| Diabetes mellitus or diabetes mellitus complications except proliferative retinopathy (CC 15-20, 120) | 28.5 | 33.7 | <.001 |
| Renal failure (CC 131) | 8.8 | 28.6 | <.001 |
| Valvular or rheumatic heart disease (CC 86) | 12 | 15.6 | <.001 |
| Vascular disease and complications (CC 104-105) | 0.2 | 0.8 | <.001 |
| Pneumonia (CC 111-113) | 5.1 | 10.6 | <.001 |
| Disorders of fluid/electrolyte/acid-base (CC 22, 23) | 2.5 | 8.9 | <.001 |
| Iron deficiency or other unspecified anemias and blood disease (CC 47) | 5.9 | 8 | <.001 |
| Chronic obstructive pulmonary disease (CC 108) | 8 | 8.5 | .023 |
| History of coronary artery bypass graft (V45.81) | 1.3 | 1.5 | .003 |
| Hemiplegia, paraplegia, paralysis, functional disability (CC 67-69, 100-102, 177-178) | 2.4 | 4 | <.001 |
| Cerebrovascular disease (97-99, 103) | 2.4 | 3.7 | <.001 |
CC, condition categories; secondary diagnoses grouped in risk factors (Pope et al.); 15 CS, cardiogenic shock; PTCA, percutaneous transluminal coronary angioplasty; STEMI, ST-segment elevation myocardial infarction.
Unless otherwise indicated, values are expressed as percentage.
The absolute number of in-hospital deaths was 25 949/311 230 (8.3%) for STEMI without CS and 14 627/19 963 (72.9%) for STEMI-related CS. The mean length of stay was 8.6 days for STEMI without CS and 9.9 days for STEMI-related CS. Excluding deaths, the mean length of hospital stay was 9±7.3 days for patients with STEMI without CS and 21.1±19.2 days for patients with STEMI-related CS (P <.001).
Clinical and demographic variables independently associated with in-hospital mortality in the multilevel risk adjustment model are shown in table 3, with CS being the most important variable (OR, 14.6; 95% CI, 14.2-15). This model showed good discriminative ability (AUROC, 0.89; 95%CI, 0.887-0.891). The specific model for in-hospital mortality for the CS-STEMI group is shown in . The AUROC for this model was 0.72; 95%CI, 0.71-0.73).
Variables independently associated with in-hospital mortality adjusted by risk in a multilevel logistic regression model in the whole cohort
| OR | P | 95%CI | |
|---|---|---|---|
| Women | 1.27 | .001 | 1.24-1.31 |
| Age (per year increase) | 1.07 | .001 | 1.06-1.07 |
| Mechanical complications of AMI (429.5 and 429.6) | 3.73 | .001 | 2.62-5.32 |
| History of CABG surgery (ICD-9 codes V45.81) | 1.22 | .001 | 1.10-1.35 |
| Congestive heart failure (CC 80) | 1.18 | .001 | 1.15-1.21 |
| Cardio-respiratory failure or shock (CC 79) | 14.58 | .001 | 14.18-15.00 |
| Stroke (CC 95-96) | 6.01 | .001 | 5.47-6.61 |
| Renal failure (CC 131) | 1.81 | .001 | 1.75-1.88 |
| Diabetes mellitus or diabetes mellitus complications except proliferative retinopathy (CC 15-20. 120) | 1.10 | .001 | 1.07-1.13 |
| Dementia or other specified brain disorders (CC 49-50) | 2.58 | .001 | 2.46-2.71 |
| Hemiplegia, paraplegia, paralysis, functional disability (CC 67-69, 100-102, 177-178) | 1.64 | .001 | 1.53-1.76 |
| Vascular disease and complications (CC 104-105) | 7.05 | .001 | 5.75-8.63 |
| Metastatic cancer, acute leukemia, and other severe cancers (CC 7-8) | 2.63 | .001 | 2.37-2.91 |
| Trauma in last year (CC 154-156, 158-162) | 1.55 | .001 | 1.33-1.81 |
| Chronic liver disease (CC 25-27) | 2.29 | .001 | 1.90-2.77 |
95%CI, 95% confidence interval; CABG, coronary artery bypass graft; CC, condition categories; CI, confidence interval; ICD-9, International Classification of Diseases-9th Revision; OR, odds ratio.
Secondary diagnoses grouped in risk factors (Pope et al.).15
This model showed acceptable calibration, with optimal agreement between observed and expected in-hospital mortality (first tertile: 0.54 vs 0.55, respectively, second tertile: 0.78 vs 0.77; and third tertile: 0.88 vs 0.88) and a significant decrease in the statistical likelihood ratio test compared with the null model (P <.001)
In the CS-STEMI group, the performance of revascularization procedures during hospitalization, either PCI or CABG, was independently associated with a lower in-hospital mortality risk (OR, 0.29; 95%CI, 0.26-0.31; P <.001 and OR, 0.25; 95%CI, 0.19-0.32; P <.001, respectively; AUROC, 0.76; 95%CI, 0.75-0.77) (). The RSMR was significantly lower in type 3 and 4 hospitals with an ICCU than in type 3 and 4 hospitals without ICCU (65.3%±7.9 vs 72±11.7; P <.001).
Time trends in CS incidence, management, mortality, and RSMR by hospital types (2003-2015)The incidence rate of CS in STEMI did not change significantly during the study period (lowest rate, 5.7%, in 2015; highest, 6.4%, in 2008) (IRR, 1; P=.62). The performance of PCI increased during the study period, from 19.2% in 2003 to 59.5% in 2015 (P for trend <.001) while there was no statistically significant change in the trend for CABG use (mean rate, 1.9%; P for trend=.35).
The proportion of type 4 hospitals () remained stable at 19.8±0.7% from 2005 to 2015 (). A total of 7807 patients with STEMI-related CS discharged from 2005 to 2015 (48%) were admitted to type 4 hospitals, while 74.2% were treated at type 3 or type 4 hospitals. The proportion of patients treated at type 4 hospitals significantly increased (P <.005) from 38.4% in 2005 to 52.9% in 2015.
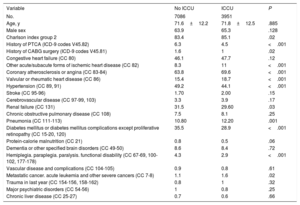
An ICCU was available in 23 Spanish hospitals in 2005 and in 28 hospitals in 2015. The proportion of type 3 and 4 hospitals with an ICCU in 2015 is shown in . There was an increase in the proportion of patients with STEMI-related CS admitted to type 3 and 4 hospitals (figure 1A), with no significant differences in age and sex in patients with STEMI-related CS according to ICCU availability. A Charlson index value ≥ 3 was more common in patients treated in type 3 and 4 hospitals with an ICCU (83.4% vs 85.1%; P=.02), although the prevalence of other comorbidities was similar according to ICCU availability (table 4). PCI in STEMI-related CS was more often performed in type 3 and 4 hospitals with ICCU than in hospitals without ICCU (60.1% vs 52.8%; P <.001) (figure 1B). The in-hospital risk-adjusted mortality rate was 65.3% in patients admitted to type 3 and 4 hospitals with an ICCU vs 72% in those without ICCU (P <.0001; figure 1C).
A: proportion of patients treated at type 4 hospitals across the study period. B: proportion of patients undergoing percutaneous coronary intervention in patients admitted to type 3 and 4 hospitals. C: risk-standardized mortality rates according to ICCU availability. ICCU, intensive cardiac care unit.
Clinical characteristics of patients with cardiogenic shock due to acute coronary syndrome treated at hospitals type 3 and 4
| Variable | No ICCU | ICCU | P |
|---|---|---|---|
| No. | 7086 | 3951 | |
| Age, y | 71.6±12.2 | 71.8±12.5 | .885 |
| Male sex | 63.9 | 65.3 | .128 |
| Charlson index group 2 | 83.4 | 85.1 | .02 |
| History of PTCA (ICD-9 codes V45.82) | 6.3 | 4.5 | <.001 |
| History of CABG surgery (ICD-9 codes V45.81) | 1.6 | 1 | .02 |
| Congestive heart failure (CC 80) | 46.1 | 47.7 | .12 |
| Other acute/subacute forms of ischemic heart disease (CC 82) | 8.3 | 11 | <.001 |
| Coronary atherosclerosis or angina (CC 83-84) | 63.8 | 69.6 | <.001 |
| Valvular or rheumatic heart disease (CC 86) | 15.4 | 18.7 | <.001 |
| Hypertension (CC 89, 91) | 49.2 | 44.1 | <.001 |
| Stroke (CC 95-96) | 1.70 | 2.00 | .15 |
| Cerebrovascular disease (CC 97-99, 103) | 3.3 | 3.9 | .17 |
| Renal failure (CC 131) | 31.5 | 29.60 | .03 |
| Chronic obstructive pulmonary disease (CC 108) | 7.5 | 8.1 | .25 |
| Pneumonia (CC 111-113) | 10.80 | 12.20 | .001 |
| Diabetes mellitus or diabetes mellitus complications except proliferative retinopathy (CC 15-20, 120) | 35.5 | 28.9 | <.001 |
| Protein-calorie malnutrition (CC 21) | 0.8 | 0.5 | .06 |
| Dementia or other specified brain disorders (CC 49-50) | 8.6 | 8.4 | .72 |
| Hemiplegia. paraplegia. paralysis. functional disability (CC 67-69, 100-102, 177-178) | 4.3 | 2.9 | <.001 |
| Vascular disease and complications (CC 104-105) | 0.9 | 0.8 | .61 |
| Metastatic cancer. acute leukemia and other severe cancers (CC 7-8) | 1.1 | 1.6 | .02 |
| Trauma in last year (CC 154-156, 158-162) | 0.8 | 1 | .32 |
| Major psychiatric disorders (CC 54-56) | 1 | 0.8 | .25 |
| Chronic liver disease (CC 25-27) | 0.7 | 0.6 | .66 |
CABG, coronary artery bypass graft; CC, condition categories; ICCU, intensive cardiac care unit; ICD-9, International Classification of Diseases-9th Revision; PTCA, percutaneous transluminal coronary angioplasty.
Unless otherwise indicated, values are expressed as mean±standard deviation or percentage.
Secondary diagnoses grouped in risk factors (Pope et al.).15
Among patients treated at type 3 and 4 hospitals, the proportion of patients undergoing revascularization procedures was similar regardless of whether they were initially admitted to that hospital or transferred from other hospitals (PCI rates, 55.2% for nontransferred patients vs 52.9% for transferred-in patients, P=.66; CABG rates, 2.5% for nontransferred vs 3.4% for transferred-in patients, P=.48). RSMRs were similar in both groups of patients (69.6%±10.8 for nontransferred patients and 70.4±10.2 for transferred-in patients, P=.46).
There was a 35% relative reduction in the unadjusted mortality rate during the study period (from 10.5% in 2003 to 6.8% in 2015) for non-CS-STEMI while the relative reduction for STEMI-related CS was 17% (from 82% in 2003 to 67.1% in 2015). The mean RSMR also decreased significantly, from 10.9% in 2003 to 6.7% in 2015 for non–CS-STEMI (IRR per year, 0.958; P <.001) and from 82.7% in 2003 to 66.8% in 2015 (IRR per year, 0.978; P <.001, figure 2).
DiscussionOur study showed a progressive decline in crude and adjusted mortality rates in patients with STEMI-related CS at the national level in Spain during the study period. This seems to be a consequence, at least in part, of the increased proportion of patients admitted to hospitals with an ICCU and the greater use of coronary revascularization in these patients.
The incidence rate of CS among the patients with STEMI in our series was 6.03%. We used an administrative database for case identification. This may have led to an underestimation of the incidence of CS. However, the underestimation was not severe, since the rate of CS in our series falls within the lower range of previously reported incidence rates of CS in STEMI patients, between 5% and 10%.18–20
In-hospital mortality in CS remains very high and is the leading cause of death in STEMI patients.1,2,4 Patients included in our study were significantly older and had higher mortality compared with previously published CS series. Our study describes a large cohort of unselected CS patients admitted to hospitals with different resources and structures, which is in contrast with several prior publications, many of which were performed in highly selected tertiary centers, often referral centers for advanced care and therapies, and therefore included relatively younger and selected populations.1–4 This may explain the discrepancy in results as advanced age is consistently associated with worse outcomes in CS.1–3,21 More importantly, both crude and adjusted mortality progressively declined during the study period. This substantial improvement in outcomes can probably be explained by the widespread use of mechanical reperfusion in patients with STEMI during the last decade,22 along with the implementation of regional reperfusion networks in Spain.23 From 2009, 6 networks were created in 6 different regions. Similar results have been observed in other countries across Europe.24 Other factors, such as the improvement in life support techniques and overall critical patient care measures, may also have contributed to the substantial reduction in mortality observed in our study.
Current guidelines6 recommend centralizing the care of patients with CS in highly specialized centers, since this approach has been consistently associated with better outcomes in this clinical setting.5 Although the proportion of type 4 hospitals remained stable during the study period, our data show a progressive increase in the number of patients treated at these hospitals (roughly, from slightly more than one third to half), indicating a significant improvement in the organization of care for CS patients over time. The availability of an ICCU was associated with higher survival rates, probably reflecting the effect of specialized training and expertise in the diagnosis and management of CS, such as pulmonary artery catheterization, implantation of temporary pacemakers, echocardiography, and the use of mechanical support devices. In addition, ICCUs may have faster and easier access to coronary revascularization procedures. This hypothesis is supported by the 14% higher rate of PCI in patients admitted to hospitals with an ICCU in our series (60.1% vs 52.8%). Patients admitted to an ICCU also had a different profile, with a higher degree of comorbidity and cardiovascular risk and greater use of therapeutic procedures such as coronary revascularization.25 This finding aligns with the recommendation to centralize the care of patients with CS. In addition, our data might support the need to expand the establishment of ICCUs in hospitals with high volumes of ACS patients. Although the high clinical complexity of these patients requires a multidisciplinary approach, the results of this study highlight the importance of the leading role of highly trained cardiologists in the management of critically-ill cardiac patients, such as those with CS.26
One of the most important strengths of this study is its high external validity, since it allows us to obtain a real picture of clinical characteristics, management, and outcomes of patients with STEMI-related CS in our setting. However, several limitations should be acknowledged. First, it is a retrospective analysis of administrative data, with inherent drawbacks. However, the use of administrative records to estimate outcomes in health care services has been validated by comparison with data from medical records7,27 and has been applied to research on health service outcomes.28 The reliability of studies of this type enables the public comparison of hospitals in terms of outcomes.29 In contrast to the methodology used by the Centers of Medicare and Medicaid Services,11,27 we did not measure 30-day mortality but rather in-hospital mortality. Additionally, secondary diagnoses as potential confounders could have been present at admission or during admission, but can also reflect suboptimal management.27 Information about the use of all types of short-term circulatory support was not available. Finally, we cannot exclude the presence of unmeasured confounding factors that may adversely impact prognosis. Despite these limitations, our study, one of the largest series of CS, provides relevant information on the factors involved in the improvement of STEMI-related CS prognosis in the era of contemporary management, particularly the fact that the clinical care of these patients in ICCUs may improve the use of revascularization therapies and patient prognosis.
ConclusionsThe proportion of patients with STEMI-related CS treated at hospitals with a cath lab and cardiac surgery facilities progressively increased during the study period, while there was a progressive reduction of both crude and adjusted mortality. Better outcomes were associated with the performance of revascularization procedures and the availability of an ICCU. These findings support the recommendation of centralizing the care of CS patients in highly specialized centers.
FundingThis work was supported by FIC (Fundación Interhospitalaria para la Investigación Cardiovascular) and Laboratorios Menarini (RECALCAR Project).
Conflicts of interestNone declared.
- –
Current guidelines recommend centralizing the care of patients with cardiogenic shock in high-volume specialized centers.
- –
No previous studies have assessed the association between the characteristics of treating centers–including the availability of an intensive cardiac care unit–and outcomes in patients with CS.
- –
The proportion of patients with STEMI-related CS treated at highly specialized centers increased while mortality decreased during the study period.
- –
Both coronary revascularization procedures and the availability of an ICCU were associated with lower adjusted mortality rates (65.3%±7.9 vs 72±11.7; P <.001).
- –
These findings strongly support the recommendation of centralizing care of these complex patients at highly specialized centers.
The authors thank the Spanish Ministry of Health, Consumer Affairs and Social Welfare for the help provided to the Spanish Society of Cardiology to perform the RECALCAR study, with special gratitude to the General Directorate of Public Health, Quality, and Innovation.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2019.10.004