Keywords
INTRODUCTION
Mortality due to acute myocardial infarction (AMI) has declined in recent years. Studies have estimated that around 35% to 50% of the reduction in deaths due to coronary heart disease between 1980 and 2000 are due to the use of treatments that have been demonstrated to be effective in clinical trials1 and are recommended in clinical practice guidelines. However, very few studies have analyzed trends in in-hospital and medium-term mortality following AMI in Spain.2,3
Clinical practice guidelines for the treatment of AMI currently recommend a more invasive management strategy involving early revascularization in patients with non-ST-elevation myocardial infaction and primary percutaneous coronary intervention (PCI) in those with ST-elevation myocardial infarction (STEMI).4-6 The definition of AMI has also changed in the last decade.7-9 The new definition of AMI and the widespread use of more sensitive and specific markers of myocardial damage such as the troponins have resulted in an increase in the recorded incidence of AMI and a reduction in 28-day mortality,10-14 partly because some cases that would previously have been considered unstable angina are now defined as AMI.
The RESCATE (Recursos Empleados en los Síndrome Coronario Agudo y Tiempos de Espera [Resources Used in Acute Coronary Syndromes and Waiting Times]) study15 was undertaken between 1992 and 1994 in 4 hospitals to determine whether availability of tertiary facilities in the admitting hospital for patients with a first AMI was related to the number of diagnostic and therapeutic procedures used and whether their availability was associated with differences in in-hospital and 6-month outcomes. Between 2001 and 2003, a second study was undertaken in the same hospitals, allowing us to assess trends in the short-term and medium-term prognosis of patients with a first AMI at the same hospitals a decade later.
The aim of this study was to analyze trends in inhospital mortality and 6-month outcomes in patients admitted to hospital with a first AMI between 1992- 1994 and 2001-2003.
METHODS
Design
RESCATE I was a follow-up study of patients with AMI carried out between 1992 and 1994 in 4 university hospitals in northeast Spain. All patients younger than 80 years of age who were admitted to hospital with a first AMI less than 72 hours since onset were consecutively enrolled. Diagnosis was based on World Health Organization criteria,7 with the appearance of a new Q wave in serial electrocardiograms or 2 of the following criteria: elevation of cardiac enzymes (elevation of creatine kinase at least twice the upper limit of the normal reference value and/or >10% increase in the MB fraction) and typical chest pain lasting more than 20 minutes.
RESCATE II was undertaken between 2001 and 2003 in the same hospitals and included all admitted patients who met the same inclusion criteria. In this analysis, we included only those patients who met the same diagnositc criteria as those included in RESCATE I in order to facilitate comparison between the groups.
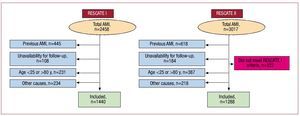
Patients with AMI who lived outside the hospital catchment area were excluded due to the follow-up limitations presented, as were those patients who had prior disease that would affect life expectancy or who did not provide signed informed consent to inclusion in the study. A flow diagram of patients included in the study is shown in Figure 1.
Figure 1. Flow diagram of patients included in both cohorts and reasons for exclusion. AMI indicates acute myocardial infarction.
Outcome Measures
The primary outcome measures were in-hospital mortality and death or readmission 6 months after AMI for the following causes: reinfarction, ventricular fibrillation or tachycardia, congestive heart failure, or unstable angina. Reinfarction was defined according to the same diagnostic criteria applied for inclusion in the study. Ventricular fibrillation or tachycardia were considered if they were sustained and led to hospital admission. Heart failure was defined according to standard diagnostic criteria.16,17 Finally, unstable angina was defined as progressive angina or angina occurring at rest that required hospital admission, according to the criteria of Braunwald.18
Follow-up was carried out on an outpatient basis or by telephone (in patients who could not attend the outpatient clinic). In patients who were readmitted to hospital, confirmation was obtained as to whether admission was for one of the outcome measures. If a death was identified through telephone contact with a family member, the cause was determined through interview with the patient's relatives or via contact with the doctor who signed the death certificate.
Treatment of Myocardial Infarction
Each hospital applied its own treatment protocol and no attempt was made to standardize management of AMI in patients at the different participating hospitals. During both periods, however, the participating hospitals used treatment protocols for AMI based on current national and international clinical practice guidelines.6,19-22 In the first cohort, only 1 hospital had a catheterization laboratory and could perform elective PCI, whereas in the second cohort 3 hospitals had these facilities; one of those was able to carry out primary PCI 24 hours a day, 7 days a week and the other 2 could only offer it during normal working hours (8 am to 5 pm, Monday to Friday). If a catheterization laboratory was not available in the hospital, reperfusion treatment for AMI involved fibrinolysis in both cohorts. In some isolated cases in RESCATE II (<1%), patients were transferred between hospitals for the purpose of primary PCI.
Study Variables in the Acute Phase of Infarction
In addition to demographics, data were collected on the following variables: history of hypertension, diabetes mellitus, hypercholesterolemia, smoking, previous angina, site of AMI, presence of Q waves in the electrocardiogram, development of pulmonary edema or cardiogenic shock, presence of malignant arrhythmias in the first 48 hours following AMI (defined as the appearance of at least 1 episode of sustained ventricular fibrillation or tachycardia that required immediate medical attention, including primary ventricular fibrillation), use of fibrinolysis or primary angioplasty, ischemia tests (pharmacologic or stress testing), performance of an echocardiogram, coronary angiography, PCI, or coronary revascularization surgery. Data on medical treatment while in hospital and upon discharge were only fully available for RESCATE II; this information was only available for 1 hospital in RESCATE I and accounted for around a third of the patients included in that cohort.
Statistical Analysis
Comparisons between the 2 cohorts were done by t test or Mann-Whitney U test for continuous variables, depending on whether or not they were normally distributed, and the c2 test for categorical variables. Comparisons of in-hospital mortality were done by unconditional logistic regression, and differences at 6-month follow-up were analyzed using Cox proportional hazards models, with adjustment for all potential confounders. In addition to the period, the multivariate models included those variables that were associated with an outcome measure and differed between the time periods studied. Clinical variables associated with prognosis (age, sex, etc) were also included in the multivariate models. Kaplan-Meier survival analysis was done and the log-rank test was used to compare the curves obtained. The cutoff for statistical significance was set at P<.05.
RESULTS
RESCATE I included 1440 consecutive patients enrolled between 1992 and 1994. In the second period, between 2001 and 2003, 1610 patients were admitted to hospital, but only those who met the original criteria for AMI and were included in the RESCATE II cohort were used in the comparative analysis (n=1288). The clinical and demographic characteristics of the patients are shown in Table 1, along with the 322 patients who were excluded from the analysis because they did not meet the diagnostic criteria applied in RESCATE I.
RESCATE II included a larger proportion of patients who were hypertensive, dyslipidemic, or had non-Q-wave AMI. In RESCATE II, more patients received reperfusion therapy (Table 2), including primary PCI, which was not available in any of the hospitals during the RESCATE I study period. Among the patients who received fibrinolysis, the median door-to-needle time was reduced from 93 (P25-75, 54-120) minutes in RESCATE I to 41 (20-90) minutes in RESCATE II (P<.001), with minimal reduction in the median time from onset of symptoms to initiation of reperfusion: 180 (120-300) minutes in RESCATE I and 180 (120-255) minutes in RESCATE II (P=.036). The median door-to-balloon time for primary PCI in RESCATE II was 90 (60-150) minutes.
More invasive procedures (coronary angiography, PCI, and surgical revascularization) and echocardiography but fewer ischemia tests were performed in RESCATE II (Table 2).
Although data on the treatments received in RESCATE I were not available for all patients, the data obtained in one of the hospitals (corresponding to almost a third of all patients) showed that administration of antiplatelet drugs and beta blockers during hospital admission increased considerably in the second cohort (71.3% vs 93.7% and 21% vs 69.6%, respectively), and that angiotensin converting enzyme (ACE) inhibitors and statins were also widely used in RESCATE II (70.2% and 76.4%, respectively).
Trends in In-Hospital and 6-Month Outcomes
Analysis of in-hospital complications revealed that the proportions of patients with maximum Killip class III-IV, angina following AMI, and ventricular arrhythmias were lower in RESCATE II. Inhospital mortality was also reduced in RESCATE II (Table 3). This in-hospital mortality remained lower following adjustment for different variables and severity of AMI (Table 4A).
Of those patients who survived the acute phase, 6-month follow-up was available for 99.9% of patients in RESCATE I and 97% in RESCATE II. There was a reduction in mortality and readmission due to angina, ventricular arrhythmias, or heart failure in RESCATE II (Table 3).
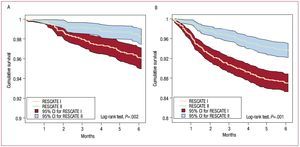
The Kaplan-Meier survival curves for fatal events (Figure 2A) and readmissions (Figure 2B) revealed a lower rate of events in patients from RESCATE II. In the multivariate analysis, following adjustment for comorbidity and indicators of AMI severity, the association between RESCATE II and improved prognosis at 6 months remained statistically significant (Table 4B-D).
Figure. 2. A: Kaplan-Meier curves for total mortality at 6 months in survivors of the acute phase in RESCATE I and II. B: Kaplan-Meier curves for readmission due to nonfatal cardiovascular causes at 6 months in survivors of the acute phase. CI indicates confidence interval.
DISCUSSION
The results of the present study show that inhospital mortality and the rate of events at 6-month follow-up in patients with a first AMI have declined in the last decade. This decline is not related to changes in the clinical characteristics or severity of AMI.
Some studies have shown an improvement in the prognosis of patients with AMI2,22-25; thus, the results of clinical trials that have demonstrated the efficacy of new treatments are supported by observations in clinical practice,26 as is the suggestion that prognosis is improved by greater adherence to the recommendations of clinical practice guidelines.27,28 In our study, reperfusion techniques (fibrinolysis and primary PCI) were more frequent and used earlier in patients from the second cohort. Reperfusion was more common in RESCATE II than in other recent Spanish studies, such as MASCARA,3 in which 62% of patients with STEMI were reperfused compared with 72.6% in RESCATE II.
The risk of in-hospital mortality in RESCATE II was lower than that observed in the PRIAMHO II study,2 which was undertaken in 2000 and in which a mortality of 11.3% was observed, an increase of more than 25% compared with RESCATE II. Although the proportions of patients with STEMI in both cohorts were similar (69% in PRIAMHO II and 71.9% in RESCATE II) and the rates of coronary risk factors were comparable, the older age of the patients in PRIAMHO II (65.4 vs 61.5 years) and the fact that 15% of those patients had a prior history of AMI could explain the higher mortality. In contrast, mortality in the MASCARA study3 was lower than in RESCATE II (5.7% vs 7.5%). The characteristics of the patients, however, differed substantially. In MASCARA, the majority of the patients had a coronary syndrome without ST elevation (only 38.3% of patients had STEMI), and these patients are known to have a lower rate of in-hospital mortality. As a result, it is difficult to make useful comparisons between the results of RESCATE II and MASCARA.
The use of invasive procedures could be an important factor in reducing the risk of in-hospital mortality,25 although the strategy has not always been associated with an improvement in outcomes.15,29 Other variables related to clinical management of patients, such as medical treatment received in hospital, are thought to have an important role in improving prognosis. Unfortunately, we cannot confirm this possibility in our study as data were only available on medical treatment for a subgroup of patients; nevertheless, the extensive use of drugs with proven efficacy for the treatment of AMI in RESCATE II could undoubtedly have played a role in improving prognosis in those patients. It is known that the combined use of beta blockers and ACE inhibitors plays an important role in improving the prognosis of patients with AMI, including in Spanish studies such as PRIAMHO II.30
The reduction in post-infarction complications, such as angina and ventricular arrhythmias, and the lower proportion of patients with Killip class III or IV is probably linked to improved patient management, although this reduction does not fully explain the decline in in-hospital mortality.
Although primary PCI is currently recommended for the treatment of STEMI,5 this technique was only used in 21.4% of reperfused patients in RESCATE II. This low percentage is explained by the general lack of availability outside normal working hours. Transfer of patients with AMI to other hospitals in order to perform primary PCI has been associated in some studies with an increase in the door-to-balloon time, delays in reperfusion, and an increase in in-hospital mortality,31 which reduces the probability of achieving the target time recommended in clinical practice guidelines.32 It would be useful to undertake future studies with multilevel analysis to evaluate qualitative aspects, such as the availability of catheterization laboratories in the same hospital, on the treatment of AMI and their relationship with mortality.
Although the same diagnostic criteria were applied in both cohorts, there was a significant increase in non-Q-wave infarctions in RESCATE II. This has been observed in other studies33 and appears to be linked not only to early reperfusion (fibrinolysis and primary PCI) but also to the widespread use of aspirin.
In our study, there was a higher prevalence of hypertension and dyslipidemia, although this may be linked to increased awareness of risk factors in the general population.34
Among those patients who survived the acute phase, there was an improvement in prognosis at 6 months, with improvements in mortality and fewer readmissions due to angina, heart failure, or ventricular arrhythmias. One of the main factors responsible for preventing loss of myocardial mass may be the greater frequency of reperfusion and this may explain the decline in readmissions observed in RESCATE II. The widespread use of ACE inhibitors and beta blockers may also explain the reduction.35,36
The main characteristic of this study is based on the consecutive recruitment of all patients with a first AMI in the same 4 hospitals, which guarantees the representativeness and external validity of the results. Furthermore, the same methodology and diagnostic protocol was used in 2 different periods, during which the clinical management of the patients involved greater use of invasive procedures and probably improvement in medical treatment.
The limitations include the previously mentioned change in the definition of AMI between the 2 periods, although the same traditional diagnostic criteria were applied in order to guarantee the reliability of the comparisons. Data on medical treatment were not available for all patients in both periods in order to analyze whether differences in mortality were linked to greater use of drugs with proven efficacy.
CONCLUSIONS
In-hospital and 6-month prognosis of patients with a first AMI in Spain have improved in the last decade. This improvement in prognosis cannot be explained by changes in clinical characteristics or severity of AMI. The increased use of reperfusion therapies, more invasive treatment of AMI (higher rates of percutaneous and surgical revascularization), and probably improvements in medical treatment may explain the reduction in in-hospital mortality and the improvement in medium-term prognosis in patients with a first AMI.
ABBREVIATIONS
AMI: acute myocardial infarction
PCI: percutaneous coronary intervention
STEMI: ST-segment elevation myocardial infarction
This study was partially funded by an unconditional grant from Sanofi-Aventis. The project was supported by the Carlos III Health Insitute (Red HERACLES RD06/0009 and CIBERESP).
Correspondence: Dr. C. García-García.
Servicio de Cardiologia. Hospital del Mar. Pg. Marítim, 25. 08003 Barcelona. Spain.
E-mail: CGarciaG@imas.imim.es
Received December 3, 2009.
Accepted for publication April 14, 2010.