Many patients undergoing transcatheter aortic valve implantation (TAVI) have concomitant mitral regurgitation (MR) of moderate grade or less. The impact of coexistent tricuspid regurgitation (TR) remains to be determined. We sought to analyze the impact of moderate vs none-to-mild MR and its trend after TAVI, as well as the impact of concomitant TR and its interaction with MR.
MethodsMulticenter retrospective study of 813 TAVI patients treated through the transfemoral approach with MR ≤ 2 between 2007 and 2015.
ResultsThe mean age was 81 ± 7 years and the mean Society of Thoracic Surgeons score was 6.9% ± 5.1%. Moderate MR was present in 37.3% of the patients, with similar in-hospital outcomes and 6-month follow-up mortality to those with MR < 2 (11.9% vs 9.4%; P = .257). However, they experienced more rehospitalizations and worse New York Heart Association class (P = .008 and .001, respectively). Few patients (3.8%) showed an increase in the MR grade to > 2 post-TAVI. The presence of concomitant moderate/severe TR was associated with in-hospital and follow-up mortality rates of 13% and 34.1%, respectively, regardless of MR grade. Moderate-severe TR was independently associated with mortality (HR, 18.4; 95%CI, 10.2-33.3; P < .001).
ConclusionsThe presence of moderate MR seemed not to impact short- and mid-term mortality post-TAVI, but was associated with more rehospitalizations. The presence of moderate or severe TR was associated with higher mortality. This suggests that a thorough evaluation of the mechanisms underlying concomitant mitral and tricuspid valve regurgitation should be performed to determine the best strategy for avoiding TAVI-related futility.
Keywords
Aortic stenosis is the most frequently treated heart valve disease in our society, followed by mitral regurgitation (MR).1 Double valve replacement may cause up to a 5-fold increase in risk for cardiac surgery compared with single valve replacement, which has limited the surgical management of dual-valve disease to less than 30% of the patients with these conditions.2 This is despite the recommendation for double valve intervention by clinical practice guidelines if both valves are severely diseased.3,4 Transcatheter aortic valve implantation has emerged as an alternative treatment strategy for patients with multivalvular disease, but the impact of significant concomitant MR has received limited evaluation in the main TAVI trials.5,6 Several studies, however, have suggested heightened mortality when significant MR persists following TAVI.7–10
In many patients undergoing TAVI, concomitant MR–when present–is usually of mild-to-moderate severity. There is a paucity of data on the implications of coexistent MR of varying severity in the post-TAVI population, which may be present in up to 70% of these patients. Additionally, although some studies have assessed the impact of tricuspid regurgitation (TR) and pulmonary hypertension (PHT) post-TAVI,11–15 the role played by right-heart hemodynamics in the outcomes of concomitant nonsignificant mitral disease is currently unknown. A better understanding of the interplay between dual-valve (and dual-sided) disease could shed further light on TAVI-related outcomes, including TAVI-related futility, which ultimately could impact decision-making strategies for such patients, while also raising further speculation on alternative percutaneous treatment strategies. The aim of this study was: a) to analyze the clinical impact of moderate vs none-to-mild MR and its variations following TAVI; and b) to determine the impact of concomitant TR in TAVI recipients with no, mild, or moderate MR.
METHODSStudy PopulationBetween August 2007 and January 2015, 1110 consecutive patients underwent TAVI in 6 different centers. The effect of moderate (3+) and severe (4+) MR has previously been reported in this study cohort.8 In the present analysis, we included 813 patients without prior mitral prostheses, with moderate (grade 2) MR severity or less with severe aortic stenosis. Only patients treated via the transfemoral approach were included. All patients were previously accepted for TAVI by a multidisciplinary team and subsequently each patient was evaluated to determine the most appropriate valve type/size and approach. Finally, clinical outcomes according to Valve Academic Research Consortium 2 (VARC-2) criteria were evaluated at each clinical visit.16
Imaging EvaluationAll patients underwent complete 2-dimensional and color-Doppler echocardiography at baseline, before discharge, and at 1- and 6-months post-TAVI. All images were digitally stored. Off-line retrospective analysis of the grade and etiology of MR and TR was performed by an experienced echocardiographist blinded to further data of the post-TAVI outcomes. Other parameters included left ventricular indices (end-diastolic and end-systolic diameters, left ventricular ejection fraction obtained by biplane Simpson's method), determination of the organic or functional/ischemic origin of the MR, mitral and aortic annular diameters, tenting height and area when indicated, and pulmonary artery systolic pressure. Baseline measurements were graded following the recommendations of the European Association of Echocardiography.17
Tricuspid regurgitation and MR grade were assessed following the European and American Guidelines on Echocardiography3,4 and accordingly classified as follows: 0 (none), 1+ (mild), 2+ (nonsignificant moderate), 3+ (significant moderate), and 4+ (severe). Patients were classified into 2 groups according to the grade of baseline MR following the same guidelines3,4: a) none or mild (0 and 1+), and b) nonsignificant moderate MR (2+). Patients with significant moderate (3+) or severe MR (4+) were excluded from this study. For statistical purposes, any decrease of 1 or more grades was considered an improvement of the MR. Pulmonary artery systolic pressure was estimated by echocardiography as previously described elsewhere3 and the remaining echocardiographic parameters, including assessment of the function of other valves and the left ventricle, followed the recommendations of scientific societies.3,4
Statistical AnalysisData are expressed as absolute frequency and percentage for qualitative variables. Quantitative variables are described as mean ± standard deviation or median (25th-75th interquartile range) depending on their distribution. Group comparisons according to the grade and improvement of MR were analyzed using the Student t test or its nonparametric equivalent, the Mann-Whitney U test for continuous variables, and the chi-square test or Fisher exact test for categorical variables. Statistical significance was defined as a P value < .05. Multivariate analysis was performed to determine independent predictors of 6-month overall mortality. Survival curves for 6-month overall and cardiac mortality were compared using a log rank test according to the MR grade and as affected by the TR for each grade.
All analyses were conducted using the statistical package IBM SPSS Statistics, version 20.0.
RESULTSFrom a total of 1110 unselected TAVI patients whose main characteristics have already been reported,8 813 (73.2%) with MR ≤ 2+ and who were treated via a transfemoral approach were selected for inclusion in the current analysis.
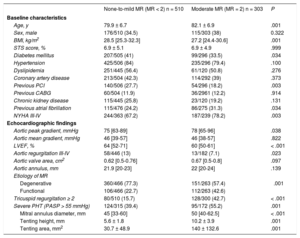
Clinical and Imaging Baseline Characteristics of the Study PopulationThe mean age of the study sample was 81 ± 7 years with 35.8% being men. The mean logistic EuroSCORE and the Society of Thoracic Surgeons scores were 15.9% ± 10.5% and 6.9 ± 5.1, respectively. The main clinical and imaging baseline characteristics of the whole sample and according to MR grade are summarized in Table 1.
Baseline and Echocardiographic Characteristics According to the Grade of Mitral Regurgitation (Moderate vs Mild or None)
| None-to-mild MR (MR < 2) n = 510 | Moderate MR (MR = 2) n = 303 | P | |
|---|---|---|---|
| Baseline characteristics | |||
| Age, y | 79.9 ± 6.7 | 82.1 ± 6.9 | .001 |
| Sex, male | 176/510 (34.5) | 115/303 (38) | 0.322 |
| BMI, kg/m2 | 28.5 [25.3-32.3] | 27.2 [24.4-30.6] | .001 |
| STS score, % | 6.9 ± 5.1 | 6.9 ± 4.9 | .999 |
| Diabetes mellitus | 207/505 (41) | 99/296 (33.5) | .034 |
| Hypertension | 425/506 (84) | 235/296 (79.4) | .100 |
| Dyslipidemia | 251/445 (56.4) | 61/120 (50.8) | .276 |
| Coronary artery disease | 213/504 (42.3) | 114/292 (39) | .373 |
| Previous PCI | 140/506 (27.7) | 54/296 (18.2) | .003 |
| Previous CABG | 60/504 (11.9) | 36/2961 (12.2) | .914 |
| Chronic kidney disease | 115/445 (25.8) | 23/120 (19.2) | .131 |
| Previous atrial fibrillation | 115/476 (24.2) | 86/275 (31.3) | .034 |
| NYHA III-IV | 244/363 (67.2) | 187/239 (78.2) | .003 |
| Echocardiographic findings | |||
| Aortic peak gradient, mmHg | 75 [63-89] | 78 [65-96] | .038 |
| Aortic mean gradient, mmHg | 46 [39-57] | 46 [38-57] | .822 |
| LVEF, % | 64 [52-71] | 60 [50-61] | < .001 |
| Aortic regurgitation III-IV | 58/446 (13) | 13/182 (7.1) | .023 |
| Aortic valve area, cm2 | 0.62 [0.5-0.76] | 0.67 [0.5-0.8] | .097 |
| Aortic annulus, mm | 21.9 [20-23] | 22 [20-24] | .139 |
| Etiology of MR | |||
| Degenerative | 360/466 (77.3) | 151/263 (57.4) | .001 |
| Functional | 106/466 (22.7) | 112/263 (42.6) | |
| Tricuspid regurgitation ≥ 2 | 80/510 (15.7) | 128/300 (42.7) | < .001 |
| Severe PHT (PASP > 55 mmHg) | 124/315 (39.4) | 95/172 (55.2) | .001 |
| Mitral annulus diameter, mm | 45 [33-60] | 50 [40-62.5] | < .001 |
| Tenting height, mm | 5.6 ± 1.8 | 10.2 ± 3.9 | .001 |
| Tenting area, mm2 | 30.7 ± 48.9 | 140 ± 132.6 | .001 |
BMI, body mass index; CABG, coronary artery bypass grafting; LVEF, left ventricular ejection fraction; MR, mitral regurgitation; NYHA, New York Heart Association; PCI, percutaneous coronary intervention; PHT, pulmonary hypertension; PASP, pulmonary artery systolic pressure; STS, Society of Thoracic Surgeons.
Data are expressed as mean ± standard deviation, No. (%), or median [interquartile range].
A total of 303 patients (37.3%) had moderate MR and 510 patients (62.7%) had no or mild MR. There were several differences in the baseline characteristics between the groups including older age and lower left ventricular ejection fraction in patients with moderate MR. Those with worse MR grade also had higher rates of atrial fibrillation (31.3% vs 24.2%; P = .034) and New York Heart Association (NYHA) class III-IV (78.2% vs 67.2%; P = .003). Median aortic peak gradient was lower in the none-to-mild MR group (75 [63-89] mmHg vs 78 [65-96] mmHg; P = .038) but without differences in the median aortic valve area. Concerning the mitral apparatus, the presence of degenerative changes was detected in 57.4% of patients with moderate MR vs 77.3% in those with none-to-mild MR (P = .001).
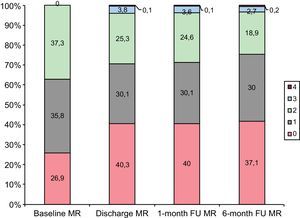
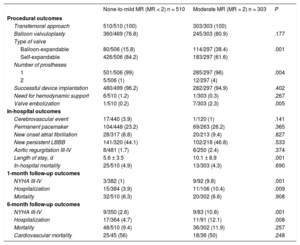
Periprocedural and Follow-up Outcomes of the Study PopulationThe main procedural, in-hospital, and follow-up outcomes are reported in Table 2. Changes in MR grade from baseline up to 6 months of follow-up are shown in Figure 1 and the predictors of this improvement are depicted in Table 1 of the . Twenty-seven percent of patients had no MR at baseline and this percentage increased up to 40% postprocedurally. Of patients with moderate MR at baseline, 3.8% experienced a deterioration in their MR grade, 15.6% improved, and the rest experienced no change.
Periprocedural and Follow-up Outcomes According to the Grade of Baseline Mitral Regurgitation
| None-to-mild MR (MR < 2) n = 510 | Moderate MR (MR = 2) n = 303 | P | |
|---|---|---|---|
| Procedural outcomes | |||
| Transfemoral approach | 510/510 (100) | 303/303 (100) | |
| Balloon valvuloplasty | 360/469 (76.8) | 245/303 (80.9) | .177 |
| Type of valve | |||
| Balloon-expandable | 80/506 (15.8) | 114/297 (38.4) | .001 |
| Self-expandable | 426/506 (84.2) | 183/297 (61.6) | |
| Number of prostheses | |||
| 1 | 501/506 (99) | 285/297 (96) | .004 |
| 2 | 5/506 (1) | 12/297 (4) | |
| Successful device implantation | 480/499 (96.2) | 282/297 (94.9) | .402 |
| Need for hemodynamic support | 6/510 (1.2) | 1/303 (0.3) | .267 |
| Valve embolization | 1/510 (0.2) | 7/303 (2.3) | .005 |
| In-hospital outcomes | |||
| Cerebrovascular event | 17/440 (3.9) | 1/120 (1) | .141 |
| Permanent pacemaker | 104/448 (23.2) | 69/263 (26.2) | .365 |
| New onset atrial fibrillation | 28/317 (8.8) | 20/213 (9.4) | .827 |
| New persistent LBBB | 141/320 (44.1) | 102/218 (46.8) | .533 |
| Aortic regurgitation III-IV | 8/481 (1.7) | 6/250 (2.4) | .374 |
| Length of stay, d | 5.6 ± 3.5 | 10.1 ± 8.9 | .001 |
| In-hospital mortality | 25/510 (4.9) | 13/303 (4.3) | .690 |
| 1-month follow-up outcomes | |||
| NYHA III-IV | 3/382 (1) | 9/92 (9.8) | .001 |
| Hospitalization | 15/384 (3.9) | 11/106 (10.4) | .009 |
| Mortality | 32/510 (6.3) | 20/302 (6.6) | .908 |
| 6-month follow-up outcomes | |||
| NYHA III-IV | 9/350 (2.6) | 9/83 (10.8) | .001 |
| Hospitalization | 17/364 (4.7) | 11/91 (12.1) | .008 |
| Mortality | 48/510 (9.4) | 36/302 (11.9) | .257 |
| Cardiovascular mortality | 25/45 (56) | 18/36 (50) | .248 |
LBBB: left bundle branch block; MR, mitral regurgitation; NYHA, New York Heart Association.
Data are expressed as mean ± standard deviation or No. (%).
Aortic valvuloplasty was performed in most patients (76.8% in those with baseline MR < 2+ vs 80.9% in those with MR = 2+; P = .177), and the predominant type of implanted valve was the self-expandable CoreValve system (75.8% of the entire cohort) including the 2 more recent device iterations: CoreValve ReValving System and CoreValve Evolute-R (CoreValve, Medtronic, United States). Although self-expanding devices were the preferred devices across both groups, those with moderate MR at baseline were more likely to receive a balloon-expandable prosthesis (38.4% vs 15.8%; P = .001), (Edwards, Edwards Lifesciences, United States) with no differences in the rate of successful device implantation according to VARC-2 criteria.16
Concerning in-hospital outcomes, no differences were found in the rate of stroke, permanent pacemaker implantation, new-onset atrial fibrillation (8.8% for MR < 2+ vs 9.4% for MR = 2+; P = .827), or significant aortic regurgitation (1.7% vs 2.4%; P = .374). Patients with moderate MR had a longer length of stay (7 [5-12] days vs 5 [4-6] days in patients with baseline MR < 2+; P = .001). In-hospital death was similar between the 2 groups (4.9% vs 4.3%; P = .69).
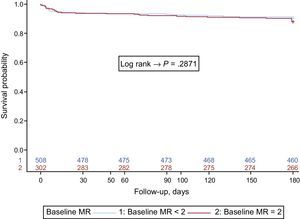
At 1-month follow-up, compared with patients with a baseline MR of 2+, those with MR < 2+ had better functional capacity (99% were NYHA I-II vs 90.2%; P = .001) and overall mortality was also comparable (6.3% vs 6.6%; P = .85). However, the need for new hospitalizations was higher in patients with baseline MR = 2+ (10.4%) than in those with lower MR grades (3.9%, P = .009). Similar tendencies persisted at 6-months’ follow-up, with no differences in overall and cardiac mortality between the 2 patient groups and greater rehospitalization rate in the moderate MR group. Survival curves according to the grade of MR are represented in Figure 2.
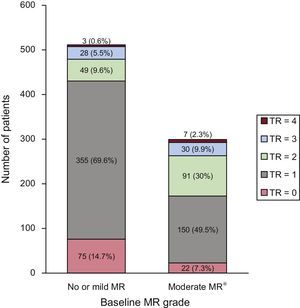
Influence of Tricuspid Regurgitation on Global OutcomesThe main baseline, procedural, and in-hospital characteristics according to baseline TR grade were comparable, as summarized in Table 2 of the . The distribution of TR grade according to the baseline MR grade (moderate vs none-to-mild) is shown in Figure 3. At baseline, 15.7% of the patients with MR < 2+ had at least moderate TR (2+), whereas this rate was 42.7% in the moderate MR group (P = .001). As summarized in the , those with a higher baseline TR grade had more progressive mitral valve disease (P < .001) at the 6-month follow-up. In addition, the rate of severe PHT was also higher in the moderate MR group (55.2%) compared with 39.4% in the none-to-mild MR group (P = .001). At 6 months of follow-up, the rate of PHT was comparable among both groups.
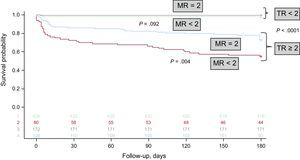
As depicted in Figure 4, the probability of survival was influenced by the presence of TR (TR ≥ 2+). Indeed, the rate of 6-month mortality among patients with moderate MR was 11.9% with no differences compared with patients with none-to-mild MR at baseline (9.4%; P = .257) and this absence of differences remained if TR was < 2+ (P = .092), with a 6-month mortality rate of 2.17%. On the contrary, the presence of TR ≥ 2+ increased overall mortality (P < .001) irrespective of the MR grade, with a rate of in-hospital mortality of 13% and 6-month mortality of 34.1%. The combination of baseline moderate MR and TR ≥ 2+ was associated with an overall mortality rate of 27.4% whereas none-to-mild MR combined with none-to-mild TR was associated with a 6-month mortality rate of 2.8% (P < .001).
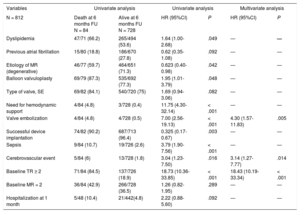
Predictors of 6-month MortalityThe main factors associated with 6-month mortality are summarized in Table 3. Independent predictors of mortality identified on multivariate analysis, with a C-index of 0.817 (95% confidence interval, 0.770-0.864), were the presence of significant baseline TR, the development of cerebrovascular events after TAVI, and valve embolization during the procedure.
Main Predictors of 6-month Mortality in the Overall Transcatheter Aortic Valve Implantation Population
| Variables | Univariate analysis | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|---|
| N = 812 | Death at 6 months FU N = 84 | Alive at 6 months FU N = 728 | HR (95%CI) | P | HR (95%CI) | P |
| Dyslipidemia | 47/71 (66.2) | 265/494 (53.6) | 1.64 (1.00-2.68) | .049 | — | — |
| Previous atrial fibrillation | 15/80 (18.8) | 186/670 (27.8) | 0.62 (0.35-1.08) | .092 | — | — |
| Etiology of MR (degenerative) | 46/77 (59.7) | 464/651 (71.3) | 0.623 (0.40-0.98) | .042 | — | — |
| Balloon valvuloplasty | 69/79 (87.3) | 535/692 (77.3) | 1.95 (1.01-3.79) | .048 | — | — |
| Type of valve, SE | 69/82 (84.1) | 540/720 (75) | 1.69 (0.94-3.06) | .082 | — | — |
| Need for hemodynamic support | 4/84 (4.8) | 3/728 (0.4) | 11.75 (4.30-32.14) | < .001 | — | — |
| Valve embolization | 4/84 (4.8) | 4/728 (0.5) | 7.00 (2.56-19.13) | < .001 | 4.30 (1.57-11.83) | .005 |
| Successful device implantation | 74/82 (90.2) | 687/713 (96.4) | 0.325 (0.17-0.67) | .003 | — | — |
| Sepsis | 9/84 (10.7) | 19/726 (2.6) | 3.79 (1.90-7.56) | < .001 | — | — |
| Cerebrovascular event | 5/84 (6) | 13/728 (1.8) | 3.04 (1.23-7.50) | .016 | 3.14 (1.27-7.77) | .014 |
| Baseline TR ≥ 2 | 71/84 (84.5) | 137/726 (18.9) | 18.73 (10.36-33.85) | < .001 | 18.43 (10.19-33.34) | < .001 |
| Baseline MR = 2 | 36/84 (42.9) | 266/728 (36.5) | 1.26 (0.82-1.95) | .289 | — | — |
| Hospitalization at 1 month | 5/48 (10.4) | 21/442(4.8) | 2.22 (0.88-5.60) | .092 | — | — |
95%CI, 95% confidence interval; FU, follow-up; HR, hazard ratio; MR, mitral regurgitation; SE, self-expandable; TR, tricuspid regurgitation.
Unless otherwise indicated, data are expressed as No. (%).
Nonsignificant baseline MR is far more common in TAVI candidates than significant MR, as recently pointed out by Mavromatis.18 In itself, within the nonsevere MR spectrum, it has no specific or direct influence on post-TAVI outcomes according to our results. This contrasts with poorer outcomes reported for patients with moderate (3+) and severe (4+) MR.8 However, coexisting baseline TR of moderate or severe grades seems to significantly impact post-TAVI outcomes in the presence of baseline MR ≤ 2 with a 10-fold increase in follow-up mortality. These findings highlight that the presence of severe aortic stenosis together with moderate regurgitation of both atrioventricular valves (even 2+) should be meticulously evaluated pre-TAVI to clarify their mechanism and the potential outcomes with the various current therapeutic strategies.
Changes in Moderate Mitral Regurgitation and Impact on OutcomesAs previously reported,8 16% of the patients in the overall cohort (n = 1110) had significant MR, which was independently associated with poorer outcomes in line with former studies.7,9–12 Only 3.8% of the patients with baseline MR of 2+ severity progressed to significant MR, but this may be an underestimate given the relatively short follow-up period. Furthermore, no relationship could be found the etiology (functional vs degenerative) of MR and the mortality, which could also be explained by the inaccuracy of this simple classification in a group of patients with several concomitant degenerative cardiac changes.10 In addition, up to 12% of the patients with baseline MR of 2+ improved to none or mild MR 6 months after TAVI, with an associated decrease in pulmonary artery systolic pressure and an improvement in NYHA class in all patients.
Although some discrepancies exist regarding the impact on outcomes of atrioventricular valve regurgitation post-TAVI in aortic stenosis patients, most of them show an improvement in the grade of the regurgitation with a parallel improvement in heart failure symptoms or functional capacity.14 However, as pointed out by Barbanti et al.,19 the response of TR to TAVI was extremely variable, and in general, TR was not an independent predictor of mortality. This highlights the relevance of our results showing a significant impact of TR on post-TAVI mortality in a selected group of patients with MR grade ≤ 2.15
Prognostic Impact of Tricuspid Regurgitation and Pulmonary Hypertension in Patients With Nonsignificant Mitral RegurgitationIn the group of patients with persistent nonsignificant MR but who had a significant grade of TR, 6-month survival was significantly lower (Figure 4). Of note, no clinically relevant baselines differences were found according to baseline TR grade, including a comparable rate of PHT and right ventricular function, reinforcing the idea that moderate and severe TR is a marker of poor prognosis in itself. Recent data suggest that both TR and PHT influence long-term survival post-TAVI.11–15 However, the impact of these 2 parameters obviously varies. By selecting a subgroup of patients with a lower grade of MR, we aimed to clear the way for interpreting the impact of TR and PHT. Indeed, our findings suggest that the presence of significant TR in the absence of significant MR in patients with severe aortic stenosis has a strong prognostic impact and requires further investigation. In some cases, treating the etiology of a tricuspid annular dilation (such as PHT resulting from different baseline conditions) may be enough. However, in some other cases, the presence of large tricuspid annuli (> 40mm of diameter)20 may tip the balance in favor of surgical (or percutaneous in the near future) tricuspid annuloplasty, especially in lower-to-intermediate risk patients.
It is well known that assessing right heart disease, including hemodynamics, is imprecise if performed only via echocardiographic methods. The echocardiographic guidelines for assessing TR3,4 are clear on the methods of measurement, but its severity is often quantified visually, and its visual severity is contingent upon the patient's preload conditions. In addition, indirect measurement of pulmonary artery systolic pressure may be inadequate and may differ by up to 10% to 20% with the measurement obtained via right heart catheterization.21 Nevertheless, several studies11,12 with echocardiographic measurements confirm its importance in post-TAVI outcomes and its direct relationship to measurements taken by right catheterization.22 In addition, a dilated tricuspid annulus despite the absence of significant TR could imply a change of therapeutic approach.23
Implications for Patients With Multivalvular DiseaseTricuspid regurgitation is often related to the grade of PHT3,4 and both are related to MR grade; therefore, those patients with MR improvement understandably stand to benefit the most, by achieving a lower rate of PHT and possibly also a subsequently lower TR grade, thus improving survival.13 However, up to 16% of the patients included in this cohort demonstrated significant persistent TR despite no or mild baseline MR. Moreover, up to 42% of the patients with moderate baseline mitral valve disease had concomitant significant baseline TR. In this group of patients, making a significant impact on survival will likely require alternative treatment options to primarily treat either de novo right heart disease or disease that could be related to nonreversible changes in the pulmonary vasculature and/or left heart. Whereas the treatment of a dilated tricuspid annulus may be of help in some cases, in others, with severe pulmonary vascular disease, greater attention will be needed for patient selection to avoid TAVI-related futility. Finally, the specific scenario of patients with prior mitral prostheses who undergo TAVI was not explored in this analysis, but in this context, the presence of TR is relatively common, which may play an important role in the prognosis and optimal therapeutic strategy for such patients.24,25
LimitationsThe main limitations of the present study include its retrospective design, which may have led to the exclusion of patients deemed surgical or inoperable who did not undergo TAVI. The off-line analysis of the images by operators unaware of the outcomes may have helped to rectify underscoring of the MR grade at the time of baseline evaluation. The follow-up period was limited to the first 6 months after discharge and the assessment of PHT by echocardiography may have been inaccurate as compared with systematic right catheterization. Finally, tricuspid annulus diameter, right chamber dimensions, and right ventricular function were not obtained, which could have shed light on the mechanisms linking TR with poor outcomes.
CONCLUSIONSThe presence of nonsignificant moderate MR did not impact short and mid-term mortality post-TAVI but was associated with a higher rate of rehospitalizations. In patients without significant mitral disease, the presence of moderate or severe TR increased mortality, suggesting that the mechanisms of this problem should be carefully evaluated to determine the best therapeutic strategy and avoid TAVI-related futility.
- –
Significant MR clearly impacts in the prognosis of patients undergoing TAVI, but the role of nonsignificant MR and concomitant significant TR remains relatively underexplored.
- –
Moderate MR in TAVI recipients influences functional recovery but not mortality whereas, in this scenario, concomitant moderate/severe TR independently predicts in-hospital and mid-term mortality.
- –
An accurate evaluation of the mechanisms underlying TR may be fundamental to determining the best therapeutic strategy for avoiding TAVI-related futility in TAVI patients with moderate MR.
Project granted by the Instituto de Salud Carlos III (PI14/00022), FEDER (Fondo Europeo de Desarrollo Regional) funds, Gerencia Regional de Salud (SACYL), and Coronary and Structural Course (award to “Multivalvular Score Project”).
CONFLICTS OF INTERESTI.J. Amat-Santos is advisor for Symetis. L. Nombela-Franco is advisor for St Jude. J.M. Hernández-Garcia is advisor for Medtronic. J. Rodés-Cabau is advisor for Edwards Lifesciences and St Jude.