Cardiovascular disease develops in a slow and subclinical manner over decades, only to manifest suddenly and unexpectedly. The role of prevention is crucial, both before and after clinical appearance, and there is ample evidence of the effectiveness and usefulness of the early detection of at-risk individuals and lifestyle modifications or pharmacological approaches. However, these approaches require time, perseverance, and continuous development. The present article reviews the developments in 2013 in epidemiological aspects related to prevention, includes relevant contributions in areas such as diet, weight control methods (obesity is now considered a disease), and physical activity recommendations (with warnings about the risk of strenuous exercise), deals with habit-related psychosocial factors such as smoking, provides an update on emerging issues such as genetics, addresses the links between cardiovascular disease and other pathologies such as kidney disease, summarizes the contributions of new, updated guidelines (3 of which have recently been released on topics of considerable clinical importance: hypertension, diabetes mellitus, and chronic kidney disease), analyzes the pharmacological advances (largely mediocre except for promising lipid-related results), and finishes by outlining developments in the oft-neglected field of cardiac rehabilitation. This article provides a briefing on controversial issues, presents interesting and somewhat surprising developments, updates established knowledge with undoubted application in clinical practice, and sheds light on potential future contributions.
Keywords
Cardiovascular disease (CVD) is a major cause of disability, substantially increases health care costs, and is the most common cause of death in developed countries. One of the most important health care activities is cardiovascular (CV) prevention, whether primary or secondary (the latter being closely linked to cardiac rehabilitation). CV prevention shows clear benefits, and has contributed to a notable reduction in CV morbidity and mortality in developed countries in recent decades. Nonetheless, much work remains to be done, as shown by data on the so-called residual risk, and the achievements made fail to mask patent deficiencies in numerous areas.1–3
The current article examines in depth the most notable developments of the last year, critically analyzing and summarizing recent results and serving as a comprehensive although not exhaustive update on these topics.
EPIDEMIOLOGICAL ASPECTSAlthough atherosclerotic CVDs are the main cause of death worldwide,2 this group of diseases have known risk factors that can be tackled by prevention.
In 2012, the latest European guidelines on CV prevention were published.3 While the guidelines continue to recommend the use of the SCORE scale for risk stratification, they include some changes and make various recommendations to achieve the targets for the different risk factors, focusing on lifestyle interventions and cardioprotective drug use. All patients should reach these targets, but that goal is far from being met, which is why knowledge of the degree of guideline implementation is essential. Accordingly, results from the EUROASPIRE IV study were presented at the recent European Society of Cardiology (ESC) meeting. This study was performed in 24 European countries to determine whether the recommendations of the latest guidelines are being followed in patients with established coronary heart disease and whether prevention has improved compared with the EUROASPIRE I, II, and III surveys.1
Reports were collected on 13 500 coronary patients, 49% of whom were interviewed. Only those younger than 80 years that had had an event between 6 months and 3 years before the interview were selected. Only 51% of smokers ceased smoking, although the percentage was 73% in Spain; 82% were overweight, a third were obese, and half had abdominal obesity. Moreover, only 41% participated in some type of prevention program. The participation rate did increase to 81% in those who were notified of the existence of the program, but only half had been informed.
A higher than recommended blood pressure (BP) was shown by 43% of patients (by 40% in Spain); 25% were unaware that they were hypertensive, and only 53% of those receiving treatment reached the BP targets. The lipids of 2 out of every 3 patients were not controlled, and 81% had a low-density lipoprotein (LDL) cholesterol level above 70mg/dL. Spain showed the best lipid control, in 59% of patients. Although 87% of patients in the survey were being treated with lipid-lowering drugs, only 21% of these were controlled. An average of 27% of the patients (or 33% in Spain) was diabetic. Another 13% had a fasting blood glucose level > 126mg/dL and, of these, 47% had a glycated hemoglobin hba level above 7%.
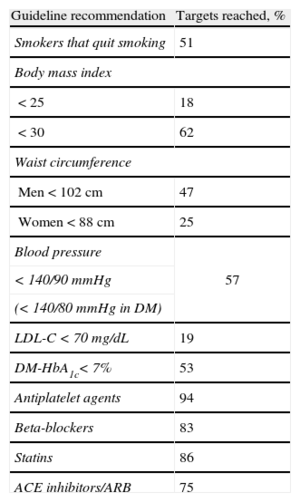
Therefore, according to this study, most coronary patients do not achieve their risk factor control targets (Table 1), even those undergoing treatment, and in turn half are not aware of the presence of these risk factors or of their levels, suggesting inadequate treatment and control. Nonetheless, the percentage of patients receiving the recommended treatments was high: anticoagulants were being taken by 94%, statins by 86%, beta-blockers by 83%, and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers 75%. In sum, not only is risk factor control poor, but also improvements are not seen.
Targets Reached in Each of the Recommendations of the Guidelines for Patients With Coronary Heart Disease, According to the EUROASPIRE IV Study
| Guideline recommendation | Targets reached, % |
| Smokers that quit smoking | 51 |
| Body mass index | |
| < 25 | 18 |
| < 30 | 62 |
| Waist circumference | |
| Men < 102 cm | 47 |
| Women < 88 cm | 25 |
| Blood pressure | 57 |
| < 140/90 mmHg | |
| (< 140/80 mmHg in DM) | |
| LDL-C < 70 mg/dL | 19 |
| DM-HbA1c< 7% | 53 |
| Antiplatelet agents | 94 |
| Beta-blockers | 83 |
| Statins | 86 |
| ACE inhibitors/ARB | 75 |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blockers; LDL-C, low-density lipoprotein cholesterol; DM, diabetes mellitus; HbA1c, glycated hemoglobin.
In the PURE study,4 performed in a cohort of 154 000 patients with history of coronary heart disease or stroke in 17 countries, the prevalence of healthy lifestyles was low, with only half quitting smoking, 19% still smoking, and just 39% and 35% with a suitable diet and level of physical activity, respectively. Although these percentages are increasing in developed countries, they remain below 50%.
In Spain, the ENRICA5 study found adequate blood cholesterol control in 43% of patients with previous CVD. A registry of the Barbanza group6 also showed poor risk factor control in 1108 patients with chronic ischemic heart disease, with data even worse than those of the EUROASPIRE study. Lower percentages of cardioprotective drug use were seen, with the exception of lipid-lowering drugs, which reached 88%.
Clearly, the data indicate the need for comprehensive and multidisciplinary prevention programs in both patients and their families, and, fundamentally, an integrated organizational model of primary and specialized care.
DIET, WEIGHT, AND PHYSICAL ACTIVITYThe most relevant diet-related contribution has been provided by the PREDIMED. The Spanish authors of this study demonstrated that a Mediterranean diet with olive oil reduced the incidence of serious CV complications by 30% in individuals at high CV risk.7 Another Spanish study, HELENA, showed that the dietary consumption of dairy is associated with lower levels of adiposity and greater cardiorespiratory fitness in adolescents.8 A meta-analysis seemed to clear egg consumption of contributing to CV risk.9 Finally, the serious impact was reiterated of artificial sweeteners and artificial sweetener-containing drinks on CV risk.10
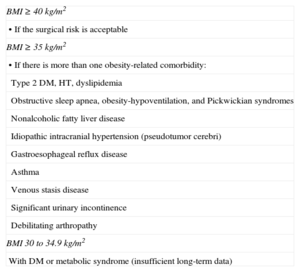
The decision of the American Medical Association to consider obesity a disease (June 2013) sparked controversy.11 Fat distribution was confirmed to influence CV risk more than weight itself.12 The lack of efficacious and safe drugs that combat obesity was confirmed once more.13,14 Thus, attention has returned to functional foods (enriched in substances that can improve health).15 The indications for bariatric surgery have been expanded (Table 2), following technical improvements and better results.16–18 As a logical consequence of the magnitude and importance of obesity, a number of initiatives have been undertaken to combat it, some in Spain.19
Indications for Bariatric Surgery (2013)
| BMI ≥ 40 kg/m2 |
| • If the surgical risk is acceptable |
| BMI ≥ 35 kg/m2 |
| • If there is more than one obesity-related comorbidity: |
| Type 2 DM, HT, dyslipidemia |
| Obstructive sleep apnea, obesity-hypoventilation, and Pickwickian syndromes |
| Nonalcoholic fatty liver disease |
| Idiopathic intracranial hypertension (pseudotumor cerebri) |
| Gastroesophageal reflux disease |
| Asthma |
| Venous stasis disease |
| Significant urinary incontinence |
| Debilitating arthropathy |
| BMI 30 to 34.9 kg/m2 |
| With DM or metabolic syndrome (insufficient long-term data) |
BMI, body mass index; DM, diabetes mellitus; HT, hypertension.
New evidence has shown the efficacy of exercise in fighting CV complications. For example, people who exercise enough to sweat at least 4 times a week have a 20% lower risk of stroke than sedentary individuals.20 There were also warnings about the risks of strenuous exercise.21 Notably, barely half of Catalan physicians take enough exercise (in addition, 20% smoke); worse is that 60% of male physicians are overweight (compared with 18% of female physicians).22
SMOKING AND PSYCHOSOCIAL FACTORSThe most vulnerable social groups are those that are most affected by smoking. In the last year, the numbers of homeless have increased due to the economic crisis, and there are now more than 2 million homeless in the United States. Over 75% of homeless people smoke, and they struggle to quit smoking due to their high prevalence of psychiatric illnesses and psychological factors, such as their placement of a higher value on immediate than deferred rewards23; a similar situation occurs in older persons, another expanding social group.24
Regarding technological advances, mobile phone applications25 and internet groups26 are useful for quitting smoking. The electronic cigarette has conquered the market in the United States, but its regulator has no powers because the manufacturers have not claimed a therapeutic effect, which is what occurred with conventional cigarettes at the start of the 20th century. It should be the nature of the product and not the maker that determines its regulation by a given body. Thus, electronic cigarettes should be regulated by the European Medicines Agency in Europe and the Food and Drug Administration in the United States.27 Meanwhile, health care professionals should discourage their use.
Although varenicline is the most effective drug for smoking cessation, together with either counseling or behavioral therapy,28 the drug has been linked to depression. However, a recent study showed that varenicline can be safely used even when there is a history of depression.29
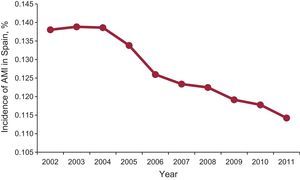
Social influence is critical in young people. Having friends or a partner who smokes is the most decisive factor in starting smoking.30 Preventing smoking from being seen as something routine would prevent many from becoming addicted. In July 2013, the Public Health Committee of the European Parliament approved a resolution aimed at stopping the tobacco industry from recruiting smokers from young people. The ESC and the Spanish Society of Cardiology support these initiatives, but the influence of cardiologists on smoking is still weak.31 Nonetheless, these measures are not fruitless: in the first year that the antismoking laws came into force in Spain, the incidence of acute myocardial infarction fell dramatically (Figure 1).32
Changes in the incidence of acute myocardial infarction in Spain from 2002 to 2011. Within an overall decreasing trend, notable decreases are seen between the years 2005 to 2006 and 2010 to 2011, coinciding with the introduction of each antismoking law. AMI, acute myocardial infarction. Reproduced from Fernández de Bobadilla et al.,32 with permission.
The developments in lipids have revolved around 2 key points: the suspension of the HPS2-THRIVE study,33 with the consequent withdrawal of niacin, and the enormous expectation generated by drugs that inhibit PCSK9 (proprotein convertase subtilisin/kexin type 9). In the case of the former, the safety committee of the HPS2-THRIVE1 study decided to prematurely end this trial due to a lack of efficacy and, more alarmingly, an increase in the incidence of serious secondary effects. The study randomly assigned patients with a history of symptomatic CVD (myocardial infarction, cerebrovascular disease, or peripheral arterial disease) undergoing statin treatment to receive either niacin plus laropiprant (2 g + 40 mg/24 h) or placebo. The suspension of the study at a mean follow-up of 3.6 years was largely due to the higher rate of treatment termination for medical reasons in the niacin group (25.4% vs 16.6%; P < .01), and increased incidences of diabetes mellitus (0.9% vs 0.4%; P < .01) and myopathies (1.8% vs 1.0%; P < .01). Study termination was accompanied by commercial withdrawal of the drug, which reignited the debate about which is the best adjunctive strategy to statin treatment. In February 2013, an update was published to the Canadian guidelines for the treatment of dyslipidemia, which continue to support treatment with statin monotherapy, at the highest tolerated dose, and does not recommend any specific combination with statins.34
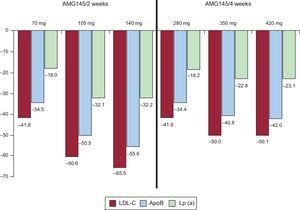
The other pharmacological strategy has garnered considerable interest: monoclonal antibodies against PCSK9, a protease that binds to the liver receptor of LDL and promotes its degradation; these monoclonal antibodies inhibit this binding action and reduce the turnover of the LDL liver receptors, increasing LDL uptake and elimination and eventually reducing its serum concentration. This therapeutic strategy has 3 key novel points compared with statins: a) its mechanism of action does not involve cholesterol synthesis, which is why it does not show the secondary hepatic and muscular effects of statins; b) it is administered subcutaneously, and c) it is administered every 2 to 4 weeks. In the annual meeting of the American College of Cardiology in March 2013, more than 7 studies were presented that showed an LDL-reducing efficacy of between 40% and 60% (Figure 2); some of these studies have already been published.35,36 Mid-way through 2013, clinical trials were started that randomize high-risk CV patients to these treatments or to placebo, which will enable determination of the real clinical benefit of this promising lipid-lowering strategy.
KIDNEY DISEASETwo developments stand out. First, the publication of a prediction score for contrast-induced nephropathy37 that involves 15 of the 46 variables most closely linked to the development of contrast-induced nephropathy in patients undergoing an intervention37,38 (available online at https://bmc2.org/calculators/cin), which helps the selection of those that would benefit from prophylaxis. KDIGO39 guidelines for chronic kidney disease also appeared, which continue to recommend the use of the glomerular filtration rate as a fundamental indicator of renal function. The main change has been the modification of the classification of kidney disease; although 5 levels remain, level 3 has been subdivided into 3a and 3b (higher or lower than 45mL/min) and various levels have been added according to albuminuria status (A1, A2, and A3). The term albuminuria should be used instead of microalbuminuria, and all patients should be referred to a specialist when the glomerular filtration rate is < 30mL/min/1.73 m2, albuminuria is > 300mg/day, albumin/creatinine ratio in urine is > 300mg/g, or proteinuria > 500mg/d.
ARTERIAL HYPERTENSIONThe most important development has been the new European Society of Hypertension/ESC guidelines.40 Although there are few modifications with respect to the 2007 to 2009 guidelines, some changes should be noted. On the one hand, the therapeutic target has been simplified, homogenizing the systolic BP for the entire population at < 140 mmHg. Exceptions are made for older people and those with diabetes mellitus or kidney disease. For diagnosis, the guidelines highlight the growing importance of ambulatory BP monitoring compared with clinical office measurement. The guidelines also reconfirm that the 5 pharmacological therapy groups can be used, and should be selected bearing in mind the patient's comorbidities; these groups include beta-blockers, whose use has sometimes been doubted. Regarding drug combinations, diuretics with angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, or calcium antagonists are preferred, as well as angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with calcium antagonists, which is a modification of the classic approach.40
Two meta-analyses were published on the effects of reducing salt consumption.41,42 Decreased salt ingestion was associated with a fall in BP, but not with a reduction in CV morbidity and mortality, which means that the clinical recommendation concerning low sodium diets in hypertensive individuals should probably be less forceful.
In Spain, 2 studies stand out. One study into renal denervation concluded that this technique, implemented via a multidisciplinary program and a proper patient selection protocol, offers an improvement in BP that is similar to that of previous studies, with a greater reduction than that produced by antihypertensive drugs and higher efficacy.43 The second study refers to the data of the PRESCAP study, which showed that hypertension control noticeably improved in Spain between 2002 and 2010, coinciding with a greater use of drug combinations.44
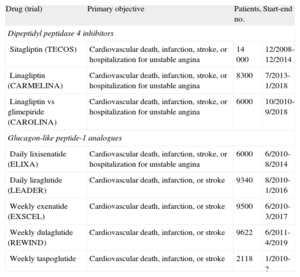
DIABETES MELLITUSRecent trials have shown that diverse lipid-lowering strategies are safe but ineffective in reducing CV events. Thus, the Look AHEAD Research Group study,45 an intensive weight-loss intervention, did not show differences in events, despite achieving reductions in weight, BP, and glycated hemoglobin. In the ORIGIN study,46 insulin glargine had no effect on CV events and cancer development, although it caused more hypoglycemia and a slight weight gain. In the SAVOR-TIMI 5347 and EXAMINE48 studies, conducted with the dipeptidyl peptidase 4 inhibitors saxagliptin and alogliptin, respectively, there was no disimprovement in CV events, although neither was there a reduction. Hospitalization from heart failure was more frequent with saxagliptin (P = .007). Although the difference in glycated hemoglobin between the groups was significant, the decrease was slight. Various trials are ongoing with glucagon-like peptide-1 analogues and dipeptidyl peptidase 4 inhibitors (Table 3).
Ongoing Clinical Trials With Incretin-based Therapies
| Drug (trial) | Primary objective | Patients, no. | Start-end |
| Dipeptidyl peptidase 4 inhibitors | |||
| Sitagliptin (TECOS) | Cardiovascular death, infarction, stroke, or hospitalization for unstable angina | 14 000 | 12/2008-12/2014 |
| Linagliptin (CARMELINA) | Cardiovascular death, infarction, stroke, or hospitalization for unstable angina | 8300 | 7/2013-1/2018 |
| Linagliptin vs glimepiride (CAROLINA) | Cardiovascular death, infarction, stroke, or hospitalization for unstable angina | 6000 | 10/2010-9/2018 |
| Glucagon-like peptide-1 analogues | |||
| Daily lixisenatide (ELIXA) | Cardiovascular death, infarction, stroke, or hospitalization for unstable angina | 6000 | 6/2010-8/2014 |
| Daily liraglutide (LEADER) | Cardiovascular death, infarction, or stroke | 9340 | 8/2010-1/2016 |
| Weekly exenatide (EXSCEL) | Cardiovascular death, infarction, or stroke | 9500 | 6/2010-3/2017 |
| Weekly dulaglutide (REWIND) | Cardiovascular death, infarction, or stroke | 9622 | 6/2011-4/2019 |
| Weekly taspoglutide | Cardiovascular death, infarction, or stroke | 2118 | 1/2010-? |
Studies of the hypoglycemic peroxisome proliferator-activated receptors alpha and gamma agonist aleglitazar have been halted due to safety concerns, although the final results remain to be published.
The ESC and European Association for the Study Of Diabetes have published new guidelines on diabetes, prediabetes, and CVD. Because the complete translation will be published in Revista Española de Cardiología49 in conjunction with comments from the point ofview of Spanish cardiology, only the most relevant points will be summarized here: a) the investigational algorithm is maintained for both patients with CVD, with or without diabetes, and those diagnosed with diabetes mellitus, with or without heart disease, although the indications are not addressed with recommendation levels or level of evidence but with a general approach that should be individualized in each case; b) the detection of ischemia in asymptomatic diabetic patients is a class IIb level C indication; c) the diagnosis of diabetes mellitus is based on the glycated hemoglobin value or on the basal fasting glucose level, and the oral glucose tolerance test is reserved for questionable cases; d) the use of classical scoring methods for calculating risk is discouraged as all diabetics are considered to have high CV risk; e) the risk factor control targets and coronary revascularization strategies are the other recent guidelines of the ESC, and the use of acetylsalicylic acid in primary prevention is discouraged, and f) the glycated hemoglobin target is less stringent (in general, < 7%), but there is little information on the use of hypoglycemic agents in CVD.
GENETICSThe last few years have shown huge developments in the understanding of the genetics of monogenic diseases, in which the presence of certain genetic variants in one or several is usually sufficient for disease appearance, and some genetic tests are even used in routine clinical practice.50 In contrast, for complex diseases such as ischemic heart disease, which are more frequent and associated with numerous genetic variants (polymorphisms) as well as environmental factors, gene identification has been less fruitful. Genome-wide association studies51 have identified 45 polymorphisms associated with ischemic heart disease, some of which are also associated with LDL cholesterol, hypertension, and inflammation, which confirms the importance of these factors in the pathogenesis of this disease.52
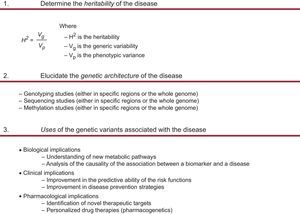
The translation of this knowledge into clinical practice and prevention is complex (Figure 3), but genetic analysis could have the following applications53: a) identification of new therapeutic targets in the treatment of hypercholesterolemia, such as antibodies against PCSK9 protein54; b) analysis of the causality of the association between biomarkers and diseases through Mendelian randomization studies, which have questioned the causal relationship between high-density lipoprotein cholesterol and ischemic heart disease55; c) improvement in the predictive ability of risk functions using genetic information, signaling their potential clinical usefulness for intermediate-risk individuals,56,57 and d) CV pharmacogenomics,58 although the results remain inconclusive. A good example of the latter is clopidogrel, a drug whose efficacy shows high interindividual variability, which has been associated in some studies with genetic variants in the CYP2C19 gene. Although the Food and Drug Administration has warned that its efficacy could depend on the patient's genetic characteristics, the American scientific societies published a consensus stating that the clinical usefulness of the genetic tests remains to be established.59 Recent meta-analyses have shown that the association is seen in studies with small sample sizes60 and have concluded that the evidence does not support the use of individualized doses of the drug according to CYP2C19 genotype.
CARDIAC REHABILITATIONFor the first time, the latest European guidelines on CV prevention3 contain a specific section on cardiac rehabilitation programs, which are considered a cost-effective approach to risk reduction following an acute coronary event because they improve prognosis and reduce hospitalizations and medical care costs, as well as prolong life. Cardiac rehabilitation after a CV episode is a class I recommendation of the ESC, the American Heart Association, and the American College of Cardiology.61,62 The new ESC clinical practice guidelines on the management of acute coronary syndrome with ST-segment elevation63 also insist on a class I indication for these programs, attaching considerable importance to the early initiation of secondary prevention measures as a way to maintain long-term adherence. In both guidelines, reference is made to the early management of psychological factors, such as stress, anxiety, and depression, and they recommend patient evaluation and appropriate treatment before hospital discharge.
New publications and a recent meta-analysis continue to show decreased morbidity and mortality through the use of these programs.64,65 However, the participation rate is low for various reasons, and strategies have been employed to improve access. A recent review stressed the need for mechanisms that automatically refer patients to rehabilitation after hospital discharge. This review also stresses the need to show health care professionals, physicians, and nonphysicians the clinical aspects and benefits of these programs.66,67 The number of prevention and cardiac rehabilitation programs in Spain is still low, and they are poorly distributed in certain regions. In recent years, some autonomous communities, such as Andalusia, the Basque Country, and the Community of Madrid, have endeavored to create new units or to increase the number of existing places to improve access to the population. However, in other regions there are no cardiac rehabilitation programs in the public health care setting. There are multiple causes for this lack of development, including the minimal support of the administrations, the economic situation, and the scant interest shown by cardiologists in some aspects of CV prevention, which is perhaps the most grievous. The Vascular Risk and Cardiac Rehabilitation Section of the Spanish Society of Cardiology is creating a register of the existing cardiac rehabilitation units, both public and private. This register will reflect the current situation and regional differences and will spur the creation of new units that improve patient access to these secondary prevention programs of proven value.
The basic components and objectives of cardiac rehabilitation have been standardized over many years, although their structures vary from one country to another. Various programs can be found, including residential, hospital-based, and home-based programs, as well as those localized in specialized units and primary care centers,68 with different levels of supervision.69 A recent review confirmed the benefits of home-based programs in low-risk patients, with results similar to those of traditional programs. Also praised were the use of new technologies (telephone, web, and videoconferencing) to improve patient access, resolving problems associated with distance, time, and compatibility with work.
Efforts should be made to maintain long-time compliance. The duration and intensity of the intervention, in addition to the participant's motivation of the participant, have been correlated with an improved prognosis. The possibility of strengthening the intervention in the long-term after a standard rehabilitation program would improve adherence. New technologies could have a prominent role in this aspect of the approach.
CONCLUSIONSVascular risk factors are of interest to all health care levels and have a social impact, because they also affect the general population. The present update indicates that while major drug trials offer results of little value, attention is shifting to classical aspects, such as lifestyle changes, because much work remains to be done in these areas, physicians can influence all segments of the population and the regulatory authorities, and the data are already available, as is happening with antismoking legislation. Marshaling the help of the skilled and available nursing staff is crucial in these tasks, particularly in health education, and, with the incorporation of telemedicine, could provide superior cost-effectiveness.
On a separate issue, consensus documents continue to appear and be updated, although the poor achievement of the indicated targets should give pause for thought. Even though drug therapy developments may be slowing, alternative interventions are appearing, from renal denervation to bariatric surgery, while new approaches fight to find a space, such as those connected to the genetic world. In the health care environs, new communication technologies between doctor, device, and patient are steadily emerging. The translation of all these approaches into improved general prevention remains a challenge.
CONFLICTS OF INTERESTNone declared.