In this article, we review the contributions of the most important imaging techniques used in cardiology, reported in 2014. Echocardiography remains the cornerstone for diagnosing and monitoring valvular heart disease, and there has been a continuing effort to improve quantification of this condition and obtain prognostic parameters for follow-up. The study of regional myocardial function is anchored in the diagnosis of subclinical ventricular dysfunction, and 3-dimensional transesophageal echocardiography has become the perfect ally in interventional procedures for structural heart disease. Cardiac magnetic resonance imaging and cardiac computed tomography are the focus of most publications on cardiac imaging in ischemic heart disease, reflecting their consolidated use in clinical practice. Nuclear medicine excels in the study of myocardial viability after interventional treatment of acute coronary syndromes and its performance is validated in the diagnosis of ischemic heart disease.
Keywords
There have been no important technological advances in echocardiography, but some striking developments have emerged in software applications for fusing transesophageal echocardiography (TEE) and X-ray fluoroscopy images to facilitate minimally-invasive treatment of structural heart disease.1 In addition, systems to measure cardiac contractility based on new algorithms have led to improvements in ultrasound wave analysis, optimizing lateral resolution.2
Contrast Myocardial Perfusion and Stress EchocardiographyRecent evidence has further supported the use of myocardial contrast echocardiography to study perfusion.3 In a multicenter study,4 the use of dipyridamole with this technique showed higher sensitivity but lower specificity than single-photon emission computed tomography (SPECT) for the detection of significant coronary artery disease in a population with a high incidence of risk factors and an intermediate-high prevalence of this condition.
Published documents on the appropriate use of stress techniques and recent guidelines from the European Society of Cardiology have indicated that these tests play an important role and are preferred over conventional stress testing.5–7 Individuals with pretest probability < 15% or > 85% do not require noninvasive testing.
Recent studies have confirmed the improved yield of images obtained at peak stress.8 In an attempt to standardize ischemia grading with different techniques, a working group designed the ISCHEMIA9 study to determine the equivalence of the results of various tests in predicting ischemic events. In patients with left bundle branch block, the yield of stress echocardiography was shown to be lower than that of dobutamine stress cardiac magnetic resonance (CMR) imaging.10 In valvular disease, such as myxomatous mitral valve regurgitation11 or aortic regurgitation,12 and in hypertrophic cardiomyopathy,13 stress echocardiography has continued to show considerable value.
Interventional ProceduresThe role of imaging techniques, particularly 3-dimensional (D) TEE, is evident in the management of patients undergoing percutaneous treatment of structural heart disease and atrial appendage closure.14 A new system has been reported for percutaneous suture ligation of the atrial appendage (LARIAT device), requiring precise 2D and 3D-TEE guidance.15
In addition, a new nomenclature system based on simple anatomic relationships has been described to define the location of paravalvular leaks; this system is easier to accommodate to the fluoroscopic view than the nomenclature based on the surgeon's view.16 In patients with severe aortic stenosis undergoing percutaneous device implantation, preprocedure measurement of the aortic annulus by a new 3D echocardiography method provides results similar to those obtained by cardiac computed tomography (CT) study and predicts the development of paravalvular regurgitation with similar precision.17
Two excellent reviews by Faletra et al18,19 have described the contribution of echocardiography in general and the 3D technique in particular before and during MitraClip implantation. It may also be possible to introduce the use of 3D-TEE in other settings, such as pulmonary vein ablation.20
Valvular Heart DiseaseLow-gradient severe aortic stenosis with preserved ejection fraction (EF) is a controversial condition. One prospective study including 260 patients reported that this condition has a poor prognosis and that valve replacement is associated with greater survival than medical treatment.21 By contrast, in another large series,22 survival was greater in low-gradient aortic stenosis than in high-gradient cases, and there was a gradual increase in the gradient over time, which could indicate that the low-gradient form is less severe. In a comparative study, echocardiography underestimated the aortic valve area compared with CMR imaging in patients with low-gradient stenosis but not in those with normal gradient, which casts doubt on the assumption that this entity is always a more advanced form of the disease.23
There are concerns about indexing aortic valve area by body surface area, as this system increases the prevalence of severe aortic stenosis cases by including patients with less advanced disease, without improving the diagnostic accuracy for valvular disease-related events.24 This is especially important in obese patients because indexing by body surface area could clearly overestimate the severity of aortic valve stenosis.25
A new score to predict the outcome of mitral valvuloplasty that incorporates mitral valve area ≤ 1 cm2, maximum leaflet displacement at diastole ≤12 mm, commissural area ratio ≥ 1.25, and subvalvular involvement has been validated in a large patient sample and has shown better predictive capacity than the Wilkins score.26
Mitral regurgitation is common following a non-ST-elevation myocardial infarction, and a long-term prospective study has shown that the presence and grade of regurgitation are both associated with a poorer prognosis. In part, this effect may be explained by negative ventricular remodeling and a higher incidence of atrial fibrillation.27
Measurement of aortic regurgitation by 2D and 3D echocardiography has been compared with CMR as the reference technique. Three dimensional echocardiography showed a better correlation and Kappa index of agreement, less dispersion, and narrower confidence limits than 2D echocardiography.28
To estimate the severity of tricuspid regurgitation, 3D echocardiography was more accurate than 2D for determining the effective regurgitant orifice area and the regurgitant volume (especially in eccentric jets) by evaluation of the proximal isovelocity surface area (PISA), using quantitative Doppler and 3D planimetry as reference29 (Figure 1).
Automatic 3D PISA, seen as a green area over a 3D color Doppler image. The upper panel provides 3 reference views (left, 4-chamber view; center, 2-chamber view; right, short-axis view), and the lower left panel shows a 3-D reconstruction of the PISA. ERO, effective regurgitant orifice; PISA, proximal isovelocity surface area.
The association between dopamine agonist use for treating pituitary tumors and valvular disease has been called into question following a multicenter study conducted in the United Kingdom30 that found no clinically significant association between the dose of this drug and age-adjusted valvular disease.
Aortic DiseaseThe aortic dilatation patterns and growth rates in patients with bicuspid aortic valve were compared with those of patients with Marfan syndrome or degenerative aortic disease. In patients with bicuspid aortic valve, dilatation of the tubular aorta was the most common pattern and exhibited the fastest growth (similar to Marfan syndrome), regardless of the valve morphology. In comparison with Marfan syndrome patients, a larger percentage of patients with bicuspid valve did not show progression of aortic dilatation. Dilatation of the sinuses was uncommon and was related with the valve morphology. Baseline aortic diameter was not proportional to the rate of progression, which implies that systematic follow-up is needed in this condition.31
In a registry of 1850 patients with a transient ischemic attack, the incidence of recurrent vascular events was related to the presence and severity of aortic atheroma detected by TEE, which supports systematic screening of this factor to optimize risk stratification in these patients.32
Ventricular FunctionDespite the growing interest in applying ventricular deformation parameters in clinical practice, one of the main limitations is that the normal values and the effect of various demographic, hemodynamic, and technical factors on these parameters is unknown. Recent publication of reference values obtained by 2D33 and 3D34 speckle tracking may foster the implementation of these parameters in routine practice. The continuing development of this technique with the emergence of new technology based on 3D deformation has had positive repercussions. Three-dimensional speckle tracking is particularly useful in the study of right ventricular function.35 Several studies have been performed comparing the 3D technique with the 2D modality, seeking simpler and more reproducible parameters, with results that are sometimes contradictory.36–38
CardiomyopathyThe usefulness of echocardiography in systematic preparticipation screening of competitive athletes was evaluated in a recent study to improve the effectiveness of programs to prevent sudden death in this population.39 The results led the authors to propose that this measure would increase sensitivity in the diagnosis of sudden death-related heart disease and would provide data showing the need for close follow-up. The reason why echocardiography study has this added value resides in the moderate sensitivity and specificity of the symptoms, clinical signs, and electrocardiography findings among sportspersons.
The benefit of studying ventricular deformation parameters in the diagnosis and prognosis of chemotherapy-related cardiovascular toxicity was brought to light following publication of several relatively small research trials over the last few years. A recent systematic review of this subject has confirmed the value of these parameters for the early detection of treatment-related myocardial abnormalities and prediction of cardiovascular toxicity.40 Use of tissue Doppler to assess the strain rate seems to provide more consistent detection of the initial changes occurring in the myocardium during therapy, whereas the best measure by speckle tracking echocardiography seems to be the overall maximum longitudinal strain. A 10% to 15% decrease during therapy seems to be the most useful parameter to predict cancer therapy-related cardiovascular toxicity, defined as an EF drop or heart failure. An excellent review on the yield of currently available noninvasive imaging modalities, clinical parameters, and research findings to identify and characterize this condition supports the systematic use of these techniques.41
NUCLEAR CARDIOLOGYIn an original study using gated-SPECT myocardial perfusion in patients with a first myocardial infarction treated with primary percutaneous revascularization, Romero-Farina et al42 described a formula that enables estimation of the at-risk and salvaged myocardium by the discordance between the extent of left ventricular wall motion and perfusion changes in the necrotic region at 4 weeks after the acute event.
In another study, the basis for indicating a second gated-SPECT myocardial perfusion study following a standard stress-rest gated SPECT consisted of clinical variables (more than 3 risk factors, or previous infarction or revascularization) as well as ergometric factors (presence of clinical or electrocardiographic ischemia).43
Abnormal systolic thickening on gated SPECT was a highly sensitive factor for early detection of left ventricular systolic dysfunction; detection of ischemia provided additional prognostic information.44
Fourier analysis using gated-SPECT myocardial perfusion has resulted in new studies on the prognostic value of left ventricular dyssynchrony in ischemic and nonischemic cardiomyopathy.45–47
This year, Rapiscan (regadenoson) was licensed for use in pharmacological stress testing in Spain. Rapiscan is a selective A2A adenosine receptor agonist with considerable activity as a coronary vasodilator, but almost no activity in the bronchi. These characteristics make it suitable for use in patients with asthma or mild/moderate chronic obstructive pulmonary disease.48
Schaap et al49 have indicated that hybrid SPECT-CT images have higher specificity than either of these techniques used alone for diagnosing ischemic heart disease in populations with an intermediate or high pretest probability of having this condition.
The use of rubidium-82 positron emission tomography (PET) myocardial perfusion imaging has demonstrated an incremental prognostic value to clinical variables in surgically revascularized patients.50
The methodological contribution of images acquired 3hours after nucleotide administration has been highlighted in the diagnosis of cardiovascular inflammation/infection with 18F-FDG-PET-CT.51,52 Use of these late images improves diagnostic accuracy without sacrificing the specificity of the technique.53
The current situation and future of PET-MR in the cardiovascular setting is described in an interesting update of these 2 techniques,54 which underscores their use in assessing myocardial viability and heart failure (Figure 2). An excellent review has compared the risks and benefits of various cardiac imaging techniques, including calcium scoring, CT angiography, dobutamine echocardiography, dobutamine cardiac MR, adenosine MR, exercise SPECT, pharmacological SPECT, adenosine PET, and invasive coronary angiography). The authors estimate that the overall risk of these techniques (due to radiation, contrast administration, and challenge maneuvers) is much lower than that of undiagnosed ischemic heart disease, ischemia prophylaxis with acetylsalicylic acid, or even any type of daily activity.55
Selected short-axis views of the left ventricle, using 99mTc-tetrofosmin myocardial perfusion SPECT at rest (A), 18F fluorodeoxyglucose PET (B), and CMR with late gadolinium enhancement (C) in a patient with an inferolateral infarction. The viability criteria show no viability in the SPECT (uptake<50%), but viability is seen in the PET (uptake ≥ 50%) and MRI (transmurality of necrosis<75%) images. CRM, cardiovascular magnetic resonance; PET, positron emission tomography; MR, magnetic resonance; SPECT, single-photon emission tomography.
At this time, cardiac CT is the cardiac imaging tool with the greatest potential to change clinical practice. Several first-rate articles in various settings have described its value for detecting cardiac allograft vasculopathy, and PET-CT has proven very useful in complex endocarditis cases.56,57
In coronary disease assessment, several studies have provided data on the prognostic value of this technique and have shown that evaluation of the extent of disease is as important as simple detection of obstructive lesions58,59 (Figure 3). The value of CT has also been observed in the emergency room, where it was shown that plaque morphology may help in predicting an acute coronary syndrome.60
The hottest topic in research with cardiac CT is the possibility of studying ischemia. The classic approach is adenosine stress testing, which has provided a diagnostic yield similar to that of cardiac MR in comparison with a pressure guidewire61 or a combination of invasive coronary angiography and nuclear medicine.62 This high yield dramatically improves the performance of the technique in complex settings, such as stent evaluation.63 Nonetheless, there is even greater interest in noninvasive study of the coronary flow reserve with cardiac CT. Data from the NXT64 study indicate that cardiac CT is a robust tool that provides better results than conventional techniques and improves the positive predictive value. Some authors have proposed that cardiac CT should be used in the follow-up of the new, bioresorbable stents because of the absence of artifacts in the images.65
Finally, there have been 2 notable technological developments: integration of CT imaging in the catheterization laboratory66 and the development of an iterative reconstruction method. This is a new image processing method, in which the radiation dose needed for the study can be reduced to 0.2 mSv,67 a reasonably low figure that may eliminate many of the concerns regarding cardiac CT.
MAGNETIC RESONANCEThe main publications this year have continued to underline the diagnostic and prognostic value of CMR in various cardiovascular diseases. In the research setting, an experimental study68 has reveled that the myocardial fibers forming both ventricles have a continuous helicoidal structure, which would confirm the helical ventricular band model proposed by Torrent-Guasp.
In patients with ischemic heart disease, wall thickness ≤ 5.5mm has been classically considered a marker of nonviable myocardium. However, a multicenter study by Shah et al69 has shown that in myocardial segments ≤ 5.5mm, nontransmural late enhancement (< 50% of wall thickness) predicts which segments will recover wall thickness and function following coronary revascularization.
In acute myocardial infarction treated by percutaneous revascularization, cardiac MR provides information that can be used to predict which patients are likely to develop malignant arrhythmia over follow-up. The main determinants of experiencing an arrhythmic event are an EF ≤ 36% and necrotic mass ≥23.5 g/m2.70
In the last few years, stress CMR has been consolidated as an excellent diagnostic and prognostic technique for evaluating patients with coronary artery disease. The combined information obtained with myocardial perfusion and coronary angiography techniques increases the diagnostic value for detecting this condition.71 Furthermore, stress-inducible ischemia is associated with a greater probability of death and experiencing an acute infarction or cardiovascular events during follow-up.72
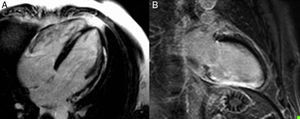
Another relevant application of CMR is in the setting of arrhythmias. In this line, CMR localization of necrosis before an ablation procedure to treat nonidiopathic ventricular tachycardia results in better planning of the access route and optimization of the results (Figure 4).73 In patients treated with resynchronization therapy, Fabregat et al74 observed that those with an EF ≥ 35% or < 35% estimated by cardiac MR showed an improvement in functional class and recovery of EF values at 6 months. Furthermore, presentation of a myocardial necrosis pattern was associated with higher rates of ventricular arrhythmia and death in both groups.
Pattern of lateral and septal subepicardial late enhancement (A) and inferior transmural late enhancement (B) in patients hospitalized for sustained monomorphic ventricular tachycardia. Localization of the fibrosis/necrosis enables planning of the access route for tachycardia ablation treatment.
CMR imaging is highly useful in the diagnosis of cardiomyopathy and right ventricular involvement. In patients with nonischemic dilated cardiomyopathy, late enhancement is a marker of increased risk of death, hospitalization for heart failure, and sudden death.75 Patients testing positive for a mutation associated with arrhythmogenic cardiomyopathy who show abnormal electrocardiography or Holter monitoring findings and morphologic changes on CMR have a higher risk of developing arrhythmic events and, therefore, are those who would benefit most from defibrillator use.76
Finally, in the evaluation of aortic stenosis, the existence of myocardial fibrosis is a predictor of death and cardiovascular events over follow-up in patients who have undergone aortic valve replacement or percutaneous treatment.77 Residual aortic regurgitation ≥ II following an interventional procedure is an indicator that the EF will not improve and that myocardial mass and ventricular volumes will decrease in comparison with patients without residual aortic failure.
CONFLICTS OF INTERESTNone declared.