This article summarizes the main developments reported in 2013 on ischemic heart disease, together with the most important innovations in the management of acute cardiac patients.
Keywords
Cardiovascular diseases are the leading cause of death in the Spanish population older than 30 years; of these diseases, ischemic heart disease has the greatest impact on this age group. A recently published estimate of the number of acute coronary syndromes (ACS) in the Spanish population in the coming years suggests that there will be more than 115 000 cases in 2013 (56% will be non-ST-segment elevation ACS [NSTEACS]), with mortality reaching nearly 35% in the first month.1 Although prehospital mortality rates have remained unchanged in recent years, there has been a decrease in hospital mortality. Projections for the next 30 years suggest that the number of ACS cases will stabilize in the population younger than 75 years and will increase in those older than 75 years such that, due to population aging, there will be an overall increase in the total number of ACS cases.1 Studies conducted in the United States show that mortality from ischemic heart disease has decreased in recent years, due to the improved control of smoking, hypertension, and dyslipidemia, but with a progressive increase in obesity and diabetes mellitus.2,3. The obesity epidemic from early ages onward remains a cause of concern. In Spain, it has been estimated that 26% of children between 8 and 17 years are overweight and 13% are obese, although this ratio seems to have stabilized during the last 12 years.4
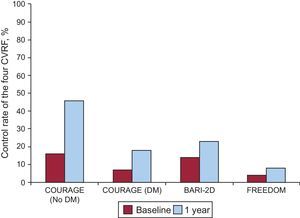
Risk factor control is far from ideal, even in the setting of secondary prevention where it could achieve greater benefit. In this regard, a recently published analysis of pooled data from 3 clinical trials (COURAGE, BARI-2D, and FREEDOM) in the diabetic population showed that, even in the controlled setting of a clinical trial, only between 8% and 23% of patients met all 4 treatment targets: low-density lipoprotein cholesterol<100 mg/dL (70 mg/dL in the FREEDOM trial), systolic blood pressure<130 mmHg, glycemic control (glycosylated hemoglobin<7%), and smoking cessation (Fig. 1).5 The main reasons given for the poor control of cardiovascular risk factors include medication underdosing and poor adherence in patients prescribed long-term polymedication therapy.
Percent control rate of the four cardiovascular risk factors in the COURAGE (data on diabetic and nondiabetic cohorts are presented separately), BARI-2D, and FREEDOM clinical trials. CVRF, cardiovascular risk factors; DM, diabetes mellitus. Adapted with permission from Farkouh et al.5.
A recently published review article by Crea et al6 proposed a new classification of ACS into 3 groups based on pathogenesis: ACS patients with obstructive atherosclerosis and systemic inflammation, ACS patients with obstructive atherosclerosis without inflammation, and ACS patients without obstructive atherosclerosis. Patients in the first group have a worse outcome and can be identified by measuring inflammation markers and even by invasive techniques. In patients without systemic inflammation, individuals at the greatest risk and the level of risk are determined by plaque characteristics (greater lesion size, reduced lumen area, or reduced fibrous cap thickness). Patients without obstructive lesions may account for a third of ACS patients and have the best outcome, although up to 10% undergo a major cardiovascular event in the first year. In this group of individuals, the cause of the problem is impaired vascular tone leading to epicardial or microvascular vasoconstriction; future research should investigate how to improve vascular tone.
CARDIOVASCULAR PREVENTIONIn primary prevention, a clinical trial showed the benefit of the Mediterranean diet in patients at high cardiovascular risk in relation to the incidence of severe cardiovascular events. The PREDIMED multicenter trial was conducted in Spain and randomly assigned 7447 participants at cardiovascular risk to a Mediterranean diet supplemented with extra virgin olive oil, a Mediterranean diet supplemented with mixed nuts, or a control diet. The results of following a Mediterranean diet were striking, with a reduction in 3 cardiovascular events per 1000 person-years and a 30% reduction in relative risk among high-risk participants who were free of cardiovascular disease.7 This effect reaffirms the benefit of a heart-healthy diet in secondary prevention, in which diet quality is inversely related to cardiovascular risk.8 This beneficial effect is additive to the pharmacologic benefit already obtained in secondary prevention. In contrast, in another large clinical trial that randomized 12 513 patients, supplementary omega-3 polyunsaturated fatty acids did not reduce cardiovascular morbidity and mortality in a population at high cardiovascular risk.9
These data highlight the crucial importance of intensive secondary prevention in patients with ischemic heart disease, especially because a recent epidemiological study has predicted that mortality from myocardial infarction will decrease in American patients compared with Spanish patients, thus reversing the trend of the last 20 years.10 The authors of this study suggest a more aggressive approach to identifying and correcting cardiovascular risk factors.
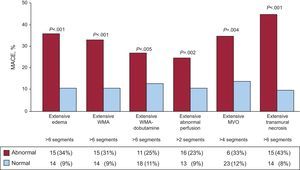
DIAGNOSTIC TECHNIQUESThe use of magnetic resonance imaging in the prognosis of postinfarction patients continues to provide valuable information. We highlight a recent Spanish study that found that a simple semiquantitative analysis of the extent of transmural necrosis was the best magnetic resonance imaging index to predict long-term outcome.11 Several resonance parameters were quantified in 206 consecutive patients 1 week after a first ST-segment elevation ACS. A semiquantitative assessment was also performed that included dobutamine wall motion abnormalities, first-pass perfusion, and microvascular obstruction. The simple and non-time-consuming semiquantitative analysis of the extent of transmural necrosis was the best index to predict the long-term outcome of these patients (Fig. 2). On the other hand, in segments with questionable viability on cardiac magnetic resonance imaging, gated single-photon emission computed tomography studies using threshold values can show uptake, as shown by a recent study published in Revista Española de Cardiología.12
Major adverse cardiovascular event rates of patients with and without extensive abnormalities in the semiquantitative indexes evaluated. MACE, major adverse cardiovascular events; MVO, microvascular obstruction; WMA, wall motion abnormalities. Reprinted with permission from Merlos et al.11.
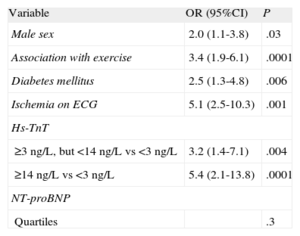
Interest in the role of the high-sensitivity cardiac troponin assay has recently increased, after its implementation in several hospitals.13 Furthermore, this assay raises questions about the role of other biomarkers. The PITAGORAS multicenter study recently showed that in low-risk patients with chest pain of uncertain origin assessed using high-sensitivity T troponin, the N-terminal pro-brain natriuretic peptide does not contribute additional predictive value to diagnosis or the prediction of short-term outcomes, whereas high-sensitivity T troponin shows a strong association with the diagnosis of NSTEACS14 (Table).
Multivariable Model With the Clinical Variables N-terminal Pro-brain Natriuretic Peptide and High-sensitivity Troponin T for the Diagnosis of Acute Coronary Syndrome
| Variable | OR (95%CI) | P |
| Male sex | 2.0 (1.1-3.8) | .03 |
| Association with exercise | 3.4 (1.9-6.1) | .0001 |
| Diabetes mellitus | 2.5 (1.3-4.8) | .006 |
| Ischemia on ECG | 5.1 (2.5-10.3) | .001 |
| Hs-TnT | ||
| ≥3 ng/L, but <14 ng/L vs <3 ng/L | 3.2 (1.4-7.1) | .004 |
| ≥14 ng/L vs <3 ng/L | 5.4 (2.1-13.8) | .0001 |
| NT-proBNP | ||
| Quartiles | .3 | |
95%CI, 95% confidence interval; ECG, electrocardiogram; hs-TnT, high-sensitivity troponin T; NT-proBNP, N-terminal pro-brain natriuretic peptide; OR, odds ratio.
Reprinted with permission from Sanchis et al.14
Copeptin is a marker of endogenous stress levels that is released immediately after the onset of chest pain. It has been proposed as a useful biomarker in the diagnosis of patients with chest pain in the emergency room15 in combination with high-sensitivity T troponin.16 Thus, the combination of high-sensitivity T troponin<14 ng/L and copeptin<14 pmol/L showed a negative predictive value of 91%.
The importance of renal function has been confirmed in the prognosis of ACS. Several studies conducted in Spain have shown that abnormal renal function17 (whether estimated using various formulas or assessed using biomarkers previously proposed as indicators of renal function) is associated with the development of clinical events in patients.18 Other studies have shown the potential role of classical biomarkers, such as inflammatory markers.19,20 Future studies could investigate novel biomarkers, such as circulating microparticles or micro-RNA,21,22 and new technologies, such as proteomics and metabolomics.23 It remains unclear whether analysis of these biomarkers, associated with prognosis, should change clinical practice with real-world patients.
NON-ST-SEGMENT ELEVATION ACUTE CORONARY SYNDROMEThe majority of information on the new oral antiplatelet agents, prasugrel and ticagrelor, has been previously published and included in the European and American guidelines for the management of NSTEACS; however, there have been few developments in recent months.
A subanalysis of the TRILOGY ACS trial was published this year,24 with results consistent with those of the TRITON-TIMI 38 trial.25 This subanalysis confirmed the benefit of prasugrel vs clopidogrel in patients undergoing coronary angiography prior to initiating treatment with prasugrel. Of the 7243 patients younger than 75 years included in the TRILOGY ACS trial, 3085 (43%) had previously undergone coronary angiography and 4158 (57%) had not. The patients with previous angiography and who were randomly assigned to prasugrel had fewer cardiovascular deaths, myocardial infarctions, or strokes (primary endpoint at 30 months) than those assigned to clopidogrel (122/1524 [10.7%] and 159/1561 [14.9%], respectively; hazard ratio [HR]=0.77; 95% confidence interval [95%CI], 0.61-0.98; P=.032), whereas no differences were found between the 2 treatments in patients without previous angiography (242/2096 [16.3%] and 238/2062 [16.7%], respectively; HR=1.01; 95%CI, 0.84-1.20; P=.94; P interaction=.08). Severe bleeding was rare in both treatment arms; although there were more episodes with prasugrel, the difference was not significant.
In contrast, the TRILOGY ACS Platelet Function Substudy,26 which included 2564 participants (27.5% of total participants), showed that in NSTEACS patients, prasugrel was associated with lower platelet reactivity than clopidogrel irrespective of age, weight, or dose (5 mg/day or 10 mg/day). Unfortunately, these differences in platelet reactivity were not matched by differences in clinical benefit, nor was a significant association found between platelet reactivity and risk of cardiovascular events.
The results of the ACCOAST trial27 were published this year. This study assessed the effect of initiating treatment with prasugrel before coronary angiography vs after angiography in 4033 NSTEACS patients. The results showed that prasugrel administered before coronary angiography in NSTEACS patients did not reduce the risk of ischemic events (cardiovascular death, myocardial infarction, stroke, or need for glycoprotein IIb/IIIa bailout at 7 days) vs administration after angiography (10% vs 9.8%; HR=1.02; 95%CI, 0.84-1.25; P=.81), but did increase the risk of major bleeding complications (2.6% vs 1.4%; HR=1.90, 95%CI, 1.19-3.02; P=.006).
Regarding novel anticoagulants in NSTEACS patients, the TAO trial28 compared the efficacy and safety of otamixaban, an intravenous direct factor Xa inhibitor, vs unfractionated heparin plus eptifibatide in 13229 NSTEACS patients treated with coronary primary percutaneous coronary intervention (PTCA). The primary endpoint (cardiovascular death or myocardial infarction at 7 days) occurred in 5.5% (279/5105) of patients treated with otamixaban and in 5.7% (310/5466) of those treated with heparin plus eptifibatide (relative risk [RR]=0.99; 95%CI, 0.85-1.16; P=.93). Furthermore, the primary safety outcome (major or minor bleeding at 7 days) occurred more frequently with otamixaban (3.1% vs 1.5%; RR=2.13; 95%CI, 1.63-2.78; P<.001).
ST-SEGMENT ELEVATION ACUTE CORONARY SYNDROMEFirst, new clinical practice guidelines have been published by the European Society of Cardiology for the management of patients with ST-segment elevation myocardial infarction (STEMI). The guidelines review the latest research on this disease and update the diagnostic and therapeutic recommendations.29 The latest developments are presented in the following sections.
Antiplatelet MedicationA new feature of the guidelines is the recommendation of the novel antiplatelet agents prasugrel and ticagrelor (I-B) vs clopidogrel for patients treated with primary PTCA. When neither of these agents is available or both are contraindicated, clopidogrel should be given instead. Clopidogrel is also the recommended antiplatelet agent as adjunct to fibrinolysis, a reperfusion strategy that has not yet been investigated using the novel antiplatelet agents. The above-mentioned recommendation of prasugrel and ticagrelor is based on data from the TRITON-TIMI 38 and PLATO clinical trials and some of their substudies.25,30–32
In the cohort of 3534 STEMI patients undergoing stent revascularization in the TRITON study, prasugrel reduced the primary endpoint vs clopidogrel (6.5% vs 9.5%; P=.002). This 30% reduction in relative risk was not associated with an increase in major bleeding. However, intracranial bleeding was significantly increased with prasugrel in subgroups of patients older than 75 years, low-weight patients (<60 kg), and patients with a history of stroke or transient cerebral ischemia.25,30
In addition, the PLATO trial also showed the superiority of ticagrelor vs clopidogrel in the subgroup of 8430 STEMI patients intended for reperfusion with primary PTCA. The primary objective was again significantly reduced (9.3% vs 11.0%; RR=0.85; P=.02) by the novel drug. Ticagrelor also reduced all-cause mortality at the limit of statistical significance, with an 18% reduction in relative risk (P=.05) and no increase in major bleeding.31,32
Therapeutic strategies and devicesAt a time when clinical practice guidelines clearly recommend PTCA as the method of choice for reperfusion and Spanish regional reperfusion programs are steadily increasing, the STREAM study analyzed the effect of prehospital fibrinolysis in patients with an early diagnosis of infarction (<3 h after symptom onset) vs primary PTCA.33 This important study randomized 1892 patients to the 2 strategies when they presented within 3h after symptom onset and were unable to undergo primary PTCA within 1 h. In the fibrinolysis group, 36% required emergency PTCA and the remainder underwent angiography within 1 day. The primary endpoint (death, shock, congestive heart failure, or reinfarction up to 30 days) was similar with both strategies, although intracranial hemorrhages were more frequent in the fibrinolysis group. The authors concluded that this pharmacoinvasive strategy may be a very good option when primary PTCA cannot be performed within 1 h after the first medical contact.
The EXAMINATION trial provided important information on the use of drug-eluting stents vs bare-metal stents in patients with STEMI treated with primary PTCA.34. Although the use of everolimus-eluting stents did not reduce the primary endpoint (death, myocardial infarction or revascularization at 1 year), it did significantly reduce target lesion revascularization and stent thrombosis. These data support the latest indication (IIa-A) for primary PTCA in the European guidelines, which recommend the use of drug-eluting stents when the patient has no contraindications to prolonged dual antiplatelet therapy (indication for oral anticoagulation or estimated high bleeding risk).29
PrognosisMyocardial regeneration, despite its demonstrated complexity, continues to be studied by several groups seeking new efficacy targets after the technique was shown to be at least safe. Two important clinical trials were presented at the 2012 American Heart Association Congress. The SWISS-AMI trial evaluated the optimal time for the infusion of bone-marrow-derived mononuclear cells in STEMI patients after primary PTCA.35 One group receiving intracoronary infusion at 5 to 7 days and another at 3 to 4 weeks were studied vs a control group. Cell infusion did not improve left ventricular function at 4 months (primary endpoint) in either group vs the control group.
A similar approach was followed by the TIME trial, which randomized ST-segment elevation ACS patients with an ejection fraction of < 45% after primary PTCA to receive intracoronary cell infusion at day 3 or at day 7 after infarction.36 Ejection fraction did not significantly improve in either group compared with the placebo group.
SPECIAL POPULATIONSFemale SexAlthough a large registry has reported similar outcomes in men and women with stable coronary artery disease,37 nonobstructive coronary artery disease in women appears to be associated with worse mid- and long-term outcome,38 and women have more events within the first year of coronary angiography39 then men. Symptoms appear to differ between the sexes. A study analyzing the symptoms induced by a 60-s occlusion of the coronary artery in the setting of PTCA showed that, although the incidence of chest pain did not differ between men and women, other symptoms, such as nausea or nonchest pain, were significantly more common in women (31% vs 14%; P=.02).40
A Cochrane review confirmed that hormone replacement therapy in postmenopausal women does not reduce coronary events, but does increase the risk of stroke and venous thromboembolic events.41 However, it should be emphasized that fertility therapies appear to be safe.42
Radiotherapy for breast cancer increases the risk of ischemic heart disease.43 It has been shown that there are sex differences in the development of cardiovascular disease related to hypertension and that blood pressures considered “normal” are associated with increased cardiovascular events in women but not in men.44
Elderly PatientsThe benefits of coronary artery bypass surgery without cardiopulmonary bypass in elderly patients compared with surgery with cardiopulmonary bypass remain undetermined. In an effort to clarify the situation, 2 recently published multicenter randomized trials compared bypass surgery with and without cardiopulmonary bypass. The German COPCABE45 trial included 2539 patients older than 75 years. At 30 days and 1 year of follow-up, there were no significant differences in the composite endpoint of death, stroke, myocardial infarction, repeat revascularization, or renal replacement therapy. A Danish study46 randomized 900 patients and no differences were found at 30 days or 6 months of follow-up. Both studies showed that both techniques gave very good results in terms of morbidity and mortality, suggesting that the choice of one technique or the other mainly depends on the surgeon's skill and the quality of the center; neither technique can be recommended over the other.
The use of drug-eluting stents in the elderly has been compared with other revascularization techniques (bare-metal stents and balloon PTCA) in 2 recent American studies conducted in 2 different clinical settings. The first study47 analyzed their use in the setting of in-stent restenosis, finding that the use of drug-eluting stents was associated with a reduced risk of mortality, myocardial infarction, and stroke compared with the other 2 techniques; however, the risk of bleeding was similar. The second study48 found a reduced risk of death, myocardial infarction, and repeat revascularization in patients undergoing revascularization of chronic total coronary occlusions.
CRITICAL CARESeveral important studies have been published this year in the field of sudden cardiac death (SCD) and cardiopulmonary resuscitation (CPR).
In Spain, there are an estimated 24 000 to 50 000 out-of-hospital cardiac arrests per year, the majority being SCD.49 A recent study by Loma-Osorio et al.50 has described the characteristics and prognoses of 204 consecutive patients with resuscitated out-of-hospital SCD treated in 5 cardiac intensive care units. The most common reason for resuscitated SCD was ischemic heart disease (70% of cases); due to this close relationship, resuscitated SCD patients are commonly treated in intensive cardiac care units. Notably, 50% of patients were discharged with good neurological outcome. These figures represent a clear improvement in the survival of these patients in Spain compared with previous figures and indicate recent advances in the treatment and care of post-resuscitated SCD syndrome patients.51
One of the most significant advances in the treatment of resuscitated SCD patients is therapeutic hypothermia (TH). The clinical guidelines recommend cooling resuscitated SCD patients to 32 C to 34°C for 12 to 24h.52 In an interesting randomized pilot study, Lopez de Sa et al53 compared the effects of TH at 2 different hypothermia levels (32°C or 34°C). At 6 months follow up, the percentage of patients with resuscitated SCD and an initial shockable rhythm discharged without significant functional limitation was significantly higher in the group assigned to 32°C compared with 34°C (61.5% vs 15.4%; P=.029). These results merit further investigation in larger controlled randomized trials.
The real effectiveness of epinephrine administration in CPR has become a matter of controversy due to the publication of conflicting results. Recently, the controversy has been fueled by the results of a large observational study in which the use of epinephrine was associated with a higher rate of recovery of spontaneous circulation but lower survival at 1 month and worse neurological outcome.54 On the other hand, a recent randomized, double-blind, placebo-controlled trial conducted in in-hospital cardiac arrest patients assessed the effectiveness of the administration of combined epinephrine-vasopressin vs epinephrine alone.55. The results showed improved survival with good neurological outcome in the patients who received the combined treatment vs the standard treatment group (13.9% vs 5.1%; odds ratio=3.28; 95%CI, 1.17-9.20; P=.02). It is difficult to draw definite conclusions because the former study was limited by being registry-based and the latter study was limited by the small sample size.
During CPR, the correct performance of chest compressions correlates with recovery of spontaneous circulation and survival. The results of the LINC study were presented at the last congress of the European Society of Cardiology. This study assessed the effectiveness of the LUCAS automatic chest compression system vs manual chest compression in a randomized study of 2589 patients with out-of-hospital SCD.56. There was no difference between the 2 groups in survival with good neurological outcome at discharge, at 1 month, and at 6 months of follow-up. From a practical perspective, however, the LUCAS system seems to be an attractive option, since it ensures the quality of chest compressions even when CPR is performed in environments that hinder their continuity and correct application; for example, in patients requiring CPR in the catheterization laboratory during percutaneous coronary intervention or implantation of a mechanical circulatory assist device.
Finally, the IABP-SHOCK-II trial was clearly one of the studies with the greatest impact in the field of critical care cardiology last year. This trial randomized 600 patients with STEMI or non-ST-elevation myocardial infarction complicated by cardiogenic shock treated with primary PTCA to circulatory support with intra-aortic balloon counterpulsation (IABP) or without IABP. There were no differences between the 2 groups in the primary endpoint of 30-day all-cause mortality or in the time to hemodynamic stabilization, the need for vasoactive agents, serum lactate levels, or renal function.57 These results generated wide debate in the scientific community.58 Follow-up at 6 months and 1 year also showed no differences between the 2 groups.59 Thus, 3 meta-analyses and 2 randomized studies have been published, showing that IABP does not significantly reduce mortality in patients with cardiogenic shock in the setting of acute myocardial infarction. However, it is anticipated that IABP will continue to be used in selected patients in most centers, given its wide availability, ease of insertion, the low rate of complications, and extensive experience, and that uncertainty remains concerning the effectiveness of other alternative devices, such as Impella® or Tandem Heart®, or ventricular support with extracorporeal membrane oxygenation.57,60–64 The circulatory support system with the greatest potential in the immediate future is probably ventricular support with extracorporeal membrane oxygenation, which combines the advantages of percutaneous insertion at the bedside, complete circulatory support, and better tissue oxygenation in patients with ACS and acute pulmonary edema.65
Conflicts of interestNone declared.