It has been shown that cardiac resynchronization therapy (CRT) improves prognosis, symptoms, and exercise capacity of patients with heart failure, severe left ventricular dysfunction, and intraventricular conduction disorders. However, despite efforts to improve candidate selection, pacing site, and device programming, 30% to 35% of patients still do not respond to this treatment.1,2
Different studies have suggested that the greatest degree of benefit from CRT is obtained by maintaining almost constant biventricular pacing.3,4 However, achieving this goal can be limited by intrinsic atrioventricular (AV) conduction and atrial fibrillation with rapid conduction to the ventricles.
The aim of our study was to describe the performance of CRT during treadmill exercise testing and evaluate its usefulness during follow-up postimplantation.
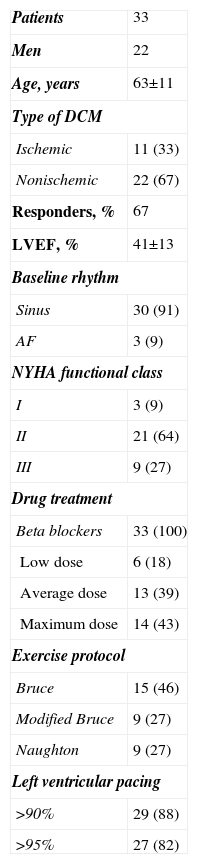
The study included 33 patients with dilated cardiomyopathy and indications for CRT; 21 (64%) responded to therapy (defined as a decrease in left ventricular end-systolic volume of at least 15% at 6 months postimplantation, compared to baseline). Table shows the clinical characteristics of the patients.
Patient Characteristics at Baseline
| Patients | 33 |
| Men | 22 |
| Age, years | 63±11 |
| Type of DCM | |
| Ischemic | 11 (33) |
| Nonischemic | 22 (67) |
| Responders, % | 67 |
| LVEF, % | 41±13 |
| Baseline rhythm | |
| Sinus | 30 (91) |
| AF | 3 (9) |
| NYHA functional class | |
| I | 3 (9) |
| II | 21 (64) |
| III | 9 (27) |
| Drug treatment | |
| Beta blockers | 33 (100) |
| Low dose | 6 (18) |
| Average dose | 13 (39) |
| Maximum dose | 14 (43) |
| Exercise protocol | |
| Bruce | 15 (46) |
| Modified Bruce | 9 (27) |
| Naughton | 9 (27) |
| Left ventricular pacing | |
| >90% | 29 (88) |
| >95% | 27 (82) |
AF, atrial fibrillation; DCM, dilated cardiomyopathy; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
Data are expressed as no. (%) or mean±standard deviation.
Treadmill exercise testing was performed using a protocol adapted to the functional status of the patient at baseline. Mean exercise time was 5.8 (3.4) min with an exercise load of 5.7 (2.1) MET and a maximum heart rate of 111 (19) bpm.
Biventricular pacing and capture was achieved in all patients at baseline except in 3 who had pseudofusion. Pacing and capture were lost in 8 (24%) of the remaining 30 patients during treadmill exercise testing. These losses were due to the maximum heart rate exceeding the set threshold (3 patients), physiological shortening of the PR interval (2 patients), loss of atrial sensing (2 patients), and the occurrence of ventricular extrasystoles induced by exercise (1 patient).
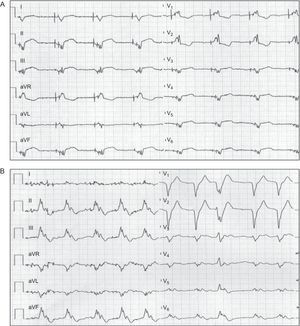
Of these 8 patients, 4 did not respond to therapy. Of the 3 patients in whom the maximum heart rate exceeded the set threshold, 2 were in atrial fibrillation and pacing was lost within the first minute of testing; AV node ablation was performed to resolve the event (Figure). For the remaining patients, the device was reprogrammed (raising the maximum heart rate threshold, shortening the AV interval, or increasing atrial sensitivity, as appropriate) and/or pharmacological treatment was optimized (increasing the dose of beta blockers).
In a retrospective study, Koplan et al.3 suggested that for CRT patients the greatest benefit was observed with >92% biventricular pacing. Subsequently, in a prospective cohort of 36 935 patients followed up in a remote-monitoring network, Hayes et al.4 observed a reduction in mortality in the group of patients with >98% biventricular pacing. This goal is difficult to achieve, especially in patients with atrial fibrillation; in these cases some researchers have recommended routine AV node ablation.5
The standard follow-up of patients with CRT includes device interrogation to evaluate the percentage of biventricular pacing and an electrocardiogram to assess capture. However, and especially when atrial fibrillation is present, assessment at rest may not be reliable.6
During exercise, physiological improvement of AV conduction, the occurrence of arrhythmias, and the potential loss of atrial sensing are the most likely causes of the loss of biventricular pacing. This loss can go unnoticed during assessment at rest and yet it affects the patient's functional capacity.
Treadmill exercise testing is a simple, accessible, and useful tool for follow-up of patients with CRT and helps to guide clinical decisions related to drug therapy, device programming, and indications for AV node ablation. The impact of the routine use of treadmill exercise testing on improving the functional capacity of these patients should be evaluated in future studies.