Cardiac resynchronization therapy improves the prognosis and symptoms of patients with advanced heart failure and intraventricular conduction disturbances.1 However, 30% of the patients do not respond to this treatment. The identification of reproducible and easily obtained parameters predictive of the response during implantation could eventually increase the number of responders.
Our objective was to determine the prognostic value of reverse modeling with regard to the different electrical parameters obtained intraoperatively.
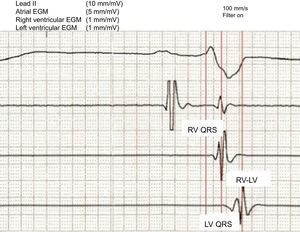
We included 62 patients with an accepted indication for implantable cardioverter defibrillator with cardiac resynchronization therapy. Paced patients were excluded. The baseline characteristics of the enrolled patients are summarized in the Table. The device was implanted in accordance with the standard procedure, with the dual-coil pacemaker-defibrillator lead placed in the apex of the right ventricle (RV) and a bipolar pacing lead placed in a vein that drains into the coronary sinus (preferably lateral or posterior). During implantation, we recorded bipolar intracavitary electrocardiograms in the left ventricle (LV) and RV simultaneously with a surface lead (II) during spontaneous rhythm at 100mm/s. We obtained the following measurements: electrical delay between the onset of the QRS complex and the intrinsic deflection in the bipolar LV electrogram (LV QRS), between the intrinsic deflections of the bipolar RV and LV electrograms (RV-LV), and between the onset of the QRS complex and the intrinsic deflection of the bipolar RV electrogram (RV QRS), in addition to the ratio between the LV QRS and the total QRS duration (Figure). The pacing configuration of the device was programmed on an individual basis (biventricular or LV alone) to optimize QRS narrowing. During the paced electrocardiogram, we determined the ΔQRS (baseline QRS width - paced QRS width). The results were obtained by averaging 3 measurements made by a single observer.
Baseline Clinical and Echocardiographic Characteristics
| Responders (n=41) | Nonresponders (n=21) | P | |
| Age, mean (SD), y | 62 (10) | 61 (12) | .80 |
| Men | 28 (70) | 12 (60) | .41 |
| Etiology | |||
| Ischemic | 12 (30) | 7 (33) | |
| Nonischemic | 29 (70) | 14 (66) | .77 |
| Baseline rhythm | |||
| Sinus rhythm | 36 (87) | 17 (80) | |
| Atrial fibrillation | 5 (12) | 4 (20) | .47 |
| Left bundle branch block | 39 (95) | 19 (90) | .49 |
| Lateral/posterior LV lead placement vs anterior position | 39 (95) | 20 (95) | .98 |
| NYHA functional class, mean (SD) | 3 (0.22) | 2.9 (0.2) | .29 |
| Drug therapy | |||
| Beta blockers | 38 (92) | 19 (90) | .76 |
| ACE inhibitors, mean (SD) | 36 (87) | 17 (80) | .47 |
| LVEF, mean (SD), % | 26 (6) | 24 (8) | .43 |
| LVEDV, mean (SD), mL | 217 (94) | 216 (100) | .96 |
| LVESV, mean (SD), mL | 163 (87) | 160 (81) | .9 |
ACE, angiotensin-converting enzyme; LV, left ventricle; LVEDV, left ventricular end-diastolic volume; LVEF, left ventricular ejection fraction; LVESV, left ventricle end-systolic volume; NYHA, New York Heart Association; SD, standard deviation.
Data are expressed as No. (%) or mean (standard deviation).
Intracavitary electrogram recording with the device programmer. EGM, electrogram; LV, left ventricle; LV QRS, interval between the onset of QRS and the intrinsic deflection of the bipolar left ventricle electrogram; RV, right ventricle; RV-LV, interval between the intrinsic deflections of the bipolar right ventricle and left ventricle electrograms; RV QRS, interval between the onset of QRS and the intrinsic deflection of the bipolar RV electrogram.
Six months after implantation, 41 patients (66%) were classified as responders as their LV end-diastolic volume had been reduced by ≥ 15% with respect to baseline.
When the baseline electrical parameters of responders were compared with those of nonresponders, we observed that a longer LV QRS (mean [SD]: 151 [30] ms vs 126 [28] ms; P=.003), a longer RV-LV (93 [28] ms vs 69 [20] ms; P=.001), and a higher LV QRS to QRS ratio (0.9 [0.2] vs 0.8 [0.2] ms; P=.03) were associated with a higher response rate 6 months after implantation. No significant differences were observed in the remainder of the parameters analyzed (baseline QRS width, 160 [17] ms vs 151 [30] ms; P=.23; RV QRS, 60 [22] ms vs 57 [17] ms; P=.53; and ΔQRS, 33 [24] ms vs 29 [22] ms; P=.62). In a multivariate analysis that included those variables with a P value of less than .10 in the univariate analysis (LV QRS, RV-LV, and LV QRS/QRS), only a longer RV-LV interval was identified as an independent predictor of response (P=.024). On the basis of the analysis of the receiver operating characteristic (ROC) curves, we established that a cutoff point of 72ms for the RV-LV interval was able to differentiate between responders and nonresponders, with a sensitivity of 83% and a specificity of 71%.
The usual objective of the implantation of cardiac resynchronization devices is to place the LV pacing lead in posterolateral veins of the coronary sinus. However, position may not be appropriate in every case, since the ventricular activation pattern varies in the presence of different intraventricular conduction disturbances. Thus, an optimal anatomical position might not correspond to the region of maximal electrical delay.
Recent subanalyses of multicenter studies have demonstrated the absence of differences in response regardless of the vein in which the electrode is placed, provided positions too near the apex are avoided.2
In 2006, Singh et al demonstrated that the duration of the LV QRS predicts the acute hemodynamic response following implantation.3 In a substudy of the SMART-AV trial involving a large patient population, Gold et al showed that the LV QRS interval predicts reverse remodeling during follow-up.4
The results obtained on the prognostic value of the RV-LV interval have been contradictory. Kristiansen et al demonstrated the existence of a direct relationship between the RV-LV interval and the decrease in ventricular volumes, but found no significant differences in response 6 months after implantation, as defined in our study.5 Likewise, in a controlled clinical trial, Miranda et al recently showed that implantation of the RV lead guided by the maximal electrical delay during LV pacing in RV outflow tract, septum, or apex increases the rate of response to cardiac resynchronization therapy compared with standard implantation in the RV apex.6
According to our results, both the LV QRS interval as a measurement of intraventricular electrical delay and the RV-LV interval as a measurement of interventricular electrical delay are predictors of reverse remodeling following the implantation of cardiac resynchronization therapy devices.