To the Editor:
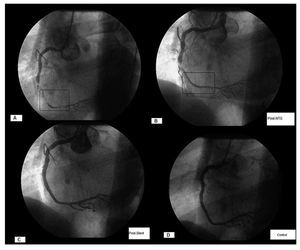
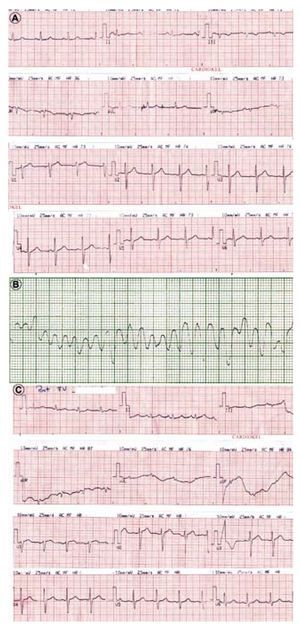
Although the incidence of ventricular fibrillation (VF) in non-ST segment elevation acute coronary syndrome (NSTE ACS) is low,1 VF after angioplasty in this context is extremely rare. We present the case of a 65 year old male, hypertensive and with dyslipidemia, admitted to the coronary service due to new onset angina, with a resting episode which ceased with sublingual nitroglycerine. The physical and laboratory tests displayed no significant findings, quantification of the MB fraction of the creatine kinase (CK-MB) was normal. The electrocardiogram highlighted minimal ST scooping in lead II and the echocardiogram disclosed a left ventricle with mild concentric hypertrophy and a preserved systolic function. He was treated with atenolol, aspirin, clopidogrel, atorvastatin, and heparin and nitroglycerine infusion. The patient had a repeat episode with ST scooping -0.5 mm in inferior leads. A coronary catheterisation was performed, which displayed sub-occlusive stenosis in the right mid coronary artery and severe distal vasospasm, dominant vessel with TIMI flow grade 2 (Figure 1A), with no significant lesions in the rest of the coronary tree. After administering intracoronary nitroglycerine, the vasospasm disappeared and the TIMI grade 3 flow was re-established, observing sub-occlusive residual stenosis in the mid-third with radiotranslucent appearance (Figure 1B). Next, treatment with tirofiban was commenced and a coronary angioplasty with a stent Flexmaster-F1 (Abbott®) 4×26 mm implant performed, post-dilated with 4.5×20mm balloon at 14 atm, with satisfactory angiographic result and no immediate complications (Figure 1C). The electrocardiogram after the angioplasty showed no significant alterations (Figure 2A). Two hours after the procedure with the patient completely asymptomatic, he presented an episode of VF (Figure 2B), immediately reverted with electrical cardioversion. Treatment with lidocaine was carried out for 24 h. The ECG after cardioversion displayed no ST segment elevation (Figure 2C). The laboratory test only displayed total CK elevation, with no significant CK-MB. Catheterisation was repeated 24 hours later and stent thrombosis excluded (Figure 1D) as well as alterations in other vessels. The patient evolved without complications, was discharged 5 days later and remained asymptomatic after a 10 month follow-up.
Figure. 1. A: basal angiogram of right coronary artery; in insert, vasospasm areas. B: angiogram after intracoronary nitroglycerine; the disappearance of vasospasm and radiotranslucent stenosis stands out. C: angiogram after stent implant. D: angiographic control after ventricular fibrillation.
Figure 2. A: electrocardiogram after angioplasty. B: ventricular fibrillation 2 hours later. C: electrocardiogram after cardioversion.
Among the possible trigger mechanisms, coronary vasospasm, with its subsequent reperfusion, could determine the appearance of malignant ventricular arrhythmias2; also, the right coronary artery is associated with a greater risk of VF during primary angioplasty.3 In our case, it was a highly developed dominant right coronary sub-occlusive stenosis. It is possible that the sudden reperfusion of the vessel determined a great formation of free radicals4 and the ventricular arrhythmia was an expression of lesion due to reperfusion. Although the incidence of vasospasm after the stent implant is unclear, in a provocation test with acetylcholine5 severe vasospasm was induced in 19.6% and 8% of the patients with and without previous vasospasm, respectively. Likewise, Kim et al6 reported a case of VF caused by vasospasm a few hours after multiple drug eluting stent implants. In this case, the initial angiograph displayed spasm at a distance from the lesion; although the patient did not experience precordial chest pain before the occasion, neither did he display ST segment elevation after cardioversion; the possibility of silent vasospasm cannot be ruled out.7
In conclusion, we reported an episode of VF without apparent trigger 2 hours after a successful angioplasty due to a NSTE ACS. This is probably an exceptional case, as predictors of this event have not been found in the literature.