An open-label study on the use of colchicine in acute pericarditis, recently published in Revista Española de Cardiología,1 challenges current practice and the recommendation of the 2015 European Society of Cardiology (ESC) guidelines2 to use colchicine as a first-line therapy for acute pericarditis (first episode). First of all, I have to declare my ideological conflict of interest, since I am an author of spontaneous trials to test the efficacy of colchicine to treat and prevent pericarditis. Nevertheless, I believe that my judgement and this article remain unbiased.
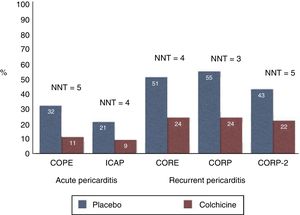
What is known on the topic?Colchicine was introduced for pericarditis, especially if recurrent, based on its positive results in the treatment and prevention of pericarditis in familial Mediterranean fever by Bayes-Genis et al.3 in the late 1980s. Following a number of case reports and series, I had the opportunity to design and conduct spontaneous randomized studies to test the safety and efficacy of colchicine for the treatment and prevention of acute and recurrent pericarditis. The first 2 trials were open-label4,5; the first was conducted in acute pericarditis (COPE trial) and the second in patients with a first recurrence (CORE trial). Subsequent trials were multicenter, double-blind trials either in acute (ICAP trial6) or recurrent pericarditis following a first (CORP trial7) or multiple recurrences (CORP-2 trial8). We learned to avoid loading doses and started using weight-adjusted doses to improve patient adherence, reducing gastrointestinal adverse effects, which occurred in up to 8% to 10% of patients. The addition of colchicine on top of standard anti-inflammatory therapy achieved an earlier response to medical therapy, increased remission rates, and reduced the recurrence rate by at least one half in all the settings explored (first episode of acute pericarditis, first episode of recurrent pericarditis, multiple recurrences) (Figure 1). On this basis, the 2015 ESC guidelines2 have recommended the use of colchicine for the treatment and prevention of pericarditis either in acute pericarditis (0.5mg twice a day [BID] for 3 months in patients weighing> 70kg or 0.5mg once daily in those weighing <70 kg) or recurrent pericarditis (same doses but for 6 months).
Main trials on colchicine for the prevention of pericarditis in acute and recurrent cases. When colchicine is added on top of standard anti-inflammatory therapy (red bars) the recurrence rate is halved (at least) and the NNT is 3 to 5, meaning that only 3 to 5 patients with pericarditis need to be treated to prevent 1 recurrence. NNT, number needed to treat.
This editorial comment discusses an open-label, multicenter trial comparing one group receiving conventional anti-inflammatory therapy (aspirin or nonsteroidal anti-inflammatory drug) with another group receiving conventional therapy plus colchicine (1mg BID or 0.5mg BID for 3 months). Acute pericarditis was defined according to only 3 criteria: a) chest pain, b) pericardial rubs, and c) electrocardiogram changes. This definition does not include pericardial effusion as a criterion for pericarditis. In contrast, pericardial effusion is considered for the definition of recurrences. After a follow-up of at least 24 months for each patient, the recurrence rate was 13.5% in the colchicine group and 7.8% in the conventional group (P=.34).
WHY SHOULDN’T THIS STUDY CHANGE CURRENT RECOMMENDATIONS TO USE COLCHICINE IN ACUTE PERICARDITIS?Despite the statement by Sambola et al. in the introduction that “until now, no medical treatment has been shown to be unquestionably effective for the treatment of recurrences”, a number of trials have shown that colchicine is the only proven medical therapy to prevent pericarditis recurrences at present.4–8 In their study, the patients were not treated with corticosteroids, but in real life this treatment is sometimes necessary and cannot be excluded from an adequate evaluation in a trial. The sample size of the study population was 110 patients, based on the assumption that the expected recurrence was 30% in the control group vs 10% in the colchicine group. In the COPE trial,4 the sample size was 120 patients and was based on a similar assumption. On this basis, the sample size of the present study seems slightly underpowered to check the suggested hypothesis. Moreover, only 102 of the initial 110 patients completed follow-up.
Diarrhea was reported in 13.5% of patients treated with colchicine, but the authors used higher than recommended doses (1mg BID or 0.5 BID instead of 0.5mg BID as the highest dose in the ESC guidelines). As a justification, the authors reported that they wanted “to guarantee the clinical effect of colchicine”. However, that is a real mistake, since it has been demonstrated that higher doses lead to more adverse effects and more drug withdrawals, and not to higher efficacy.
Overall this study seems underpowered and to have selected a low-risk population of patients with acute pericarditis with a low frequency of pericardial effusion (around 30%) and with no patients treated with corticosteroids. Moreover, colchicine dosing was too high with double dosing compared with recommended levels. This study population rarely corresponds to what can be seen in real life, thus making the results questionable and not applicable to clinical practice. Colchicine is especially efficacious in inflammatory pericarditis with fever, pericardial effusion, and elevated C-reactive protein, and there is no mention of C-reactive protein in this study.
For these reasons, although in the past I have greatly appreciated the contributions of these authors to the evaluation and triage of patients with pericarditis, at this time, I believe they have provided misleading data that cannot change my approach to acute pericarditis, consisting of colchicine added to aspirin or nonsteroidal anti-inflammatory drugs as first-line options, as correctly pointed out by 2015 ESC guidelines. When assessed in an appropriately large population, colchicine has been shown to significantly decrease the recurrence rate of pericarditis, regardless of prednisone use and the cause of pericarditis.8,9
Conflicts of interestAuthor of spontaneous trials on the use of colchicine to treat and prevent pericarditis. Institutional research grants from ACARPIA.