Patients with a Wolff-Parkinson-White (WPW) pattern in the electrocardiogram (ECG) show a short PR interval (<120ms), a wide QRS complex (>100ms) with a delta wave, and a normal PJ interval. Broad QRS complexes may simulate bundle branch block (BBB). Furthermore, premature depolarization of ventricular myocardium through an accessory pathway tends to conceal any electrocardiographic manifestation of a BBB. WPW syndrome cannot prolong the PJ interval; therefore, PJ interval prolongation plays an important role in the differential diagnosis between BBB and WPW syndrome. However, could a normal PJ interval rule out BBB in the presence of WPW syndrome?
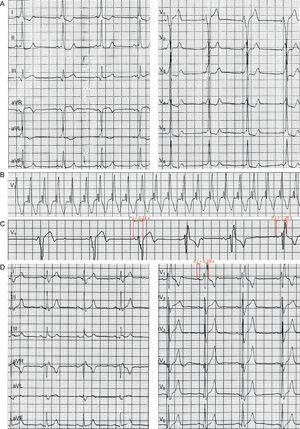
A 28-year-old man with a 3-year history of frequent attacks of tachycardia was admitted to our hospital because of palpitations. The ECG revealed a sinus rhythm of approximately 60 beats/min, a PR interval of 0.10s, and a QRS duration of 0.14 s (with a delta wave), with rS pattern in lead V1, suggestive of WPW syndrome type B (Fig. A). An ECG brought by the patient showed tachycardia of approximately 160 beats/min with broad QRS complexes of right bundle branch block (RBBB) morphology (Fig. B). The admission ECG demonstrated RBBB during the intermittency of preexcitation (Fig. C). Electrophysiological study and radiofrequency ablation (the accessory pathway [AP] located in tricuspid annulus 9:00) were performed. Postablation ECG showed RBBB with a PJ interval of 0.28s (Fig. D).
The PJ interval represents the time elapsed from the beginning of the P wave to the end of the QRS complex (J for junction between QRS and T wave) in the ECG. In addition, the PJ interval is equal to the sum of the PR interval (the time interval from the onset of atrial depolarization to the onset of ventricular depolarization) and the QRS interval (the total ventricular activation time), with a normal value of less than 0.27s. A prolonged PJ interval is mainly observed in patients with first-degree atrioventricular block (AVB) or BBB. The diagnosis of first degree AVB is usually made on the basis of a prolonged PR interval.1 Likewise, BBB is often diagnosed on the basis of the QRS morphology and duration. Consequently, the PJ interval is usually ignored in routine ECG analysis. However, the AVB or BBB is usually obscured by the antegrade conduction of AP in preexcitation syndrome. Consequently, a diagnosis of WPW coexisting with AVB or BBB cannot be made on the basis of the relationship between P waves and QRS complexes and the morphology of the QRS complex.2,3 During this time, analysis of the PJ interval is more important. In WPW syndromes, the PJ interval is normal. Accordingly, PJ interval prolongation plays an important role in the differential diagnosis between BBB and WPW syndrome. Furthermore, recent studies have confirmed that PJ interval prolongation was a diagnostic clue of WPW syndrome coexisting with AVB or BBB4–6: a) the PJ interval is prolonged during sinus rhythm, and the QRS complex is BBB pattern in the presence of atrioventricular reentrant tachycardia (can rule out third-degree AVB), suggestive of WPW syndrome coexisting with BBB; b) the PJ interval is prolonged during sinus rhythm, and the narrow QRS complex (rule out BBB) is observed in the presence of reentrant tachycardia indicating WPW syndrome accompanied by first-degree AVB in the normal His-Purkinje pathway; and c) the and PJ interval is prolonged during sinus rhythm, and the QRS complex is consistently full preexcitation (same as conducted sinus beat) during atrial fibrillation (reentrant tachycardia cannot be induced), suggesting WPW syndrome coexisting with third-degree AVB in the normal His-Purkinje pathway. In our case, the association of WPW syndrome type B and RBBB (with a PJ interval of 0.28s after ablation) was proven by ambulatory ECG, electrophysiological study, and radiofrequency ablation. However, the PJ interval was only 0.24s and the RBBB pattern was obscured in the presence of ipsilateral ventricular preexcitation. The mechanism is as follows: when the AP is on the same side as the ventricle with the blocked bundle branch, the ipsilateral ventricle is prematurely depolarized by antegrade conduction of AP, the ECG features of BBB are masked, and the total ventricular depolarization time via normal His-Purkinje pathway is reduced, which is responsible for the normal PJ interval. The findings of this article indicate that clinicians should measure the PJ interval before ablation of AP in patients with WPW syndrome. A prolonged PJ interval is often observed in the following conditions: a) when the AP is on the contralateral side to the ventricle with the blocked bundle branch; b) in those patients with AVB. When the PJ interval is prolonged, the region of block should be further analyzed according to the ECG characteristics of tachycardia; when the PJ interval is normal and the QRS complex is an ipsilateral BBB pattern of AP during the reentrant tachycardia (especially when the heart rate<150bpm), clinicians should consider the presence of BBB and inform the patient and his or her family of the clinical features.