Dual left anterior descending (LAD) artery is a congenital coronary anatomical variant1 that has several recognized types,1–3 but a Y-shaped confluent dual LAD has not been previously described.
We present the case of a 69-year-old man admitted for elective coronary angiography due to stable exertional angina, with a reversible myocardial diffusion defect in the inferolateral left ventricular wall (single photon emission tomography with 99mTc-MIBI).
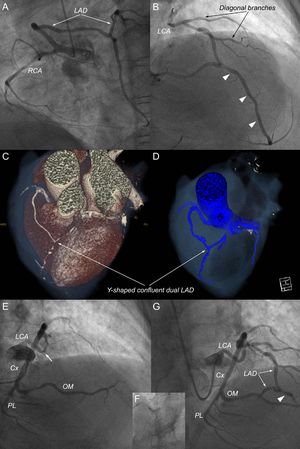
An angiogram of the right coronary artery (RCA) showed a nondominant artery with an unusual branch emerging from the proximal segment, passing above the right ventricular outflow tract (demonstrated on computed tomography angiography) and reaching the anterior interventricular sulcus, where it joined the LAD proper to form the vessel that normally reaches the apex (Figure 1A-D). shows retrograde entry of the contrast towards the left coronary artery (LCA), although the antegrade blood flow does not allow visualization of the circumflex artery.
A and B: unusual branch originating from the RCA and converging with the LAD (left anterior oblique view); the arrowheads indicate the distal LAD. C and D: multiplanar reconstruction of tomographic images. E: left coronary angiography (anteroposterior cranial view); dominant Cx and severe lesion of LCA (arrow). F: stent implantation. G: result of the coronary intervention and confluence of the 2 branches that continue as a single vessel (distal LAD, arrowhead) toward the apex. Cx, circumflex; LAD, left anterior descending artery; LCA, left coronary artery; OM, obtuse marginal; PL, posterolateral branches; RCA, right coronary artery.
Left coronary angiography showed a severe eccentric stenosis in the LCA, which was treated with a 3.0 × 15mm everolimus-eluding stent (Xience, Abbott Vascular), with a good angiographic result (Figure 1E-G). Spider view () shows the LCA lesion, left-dominance, and the competitive flow in the LAD.
This anatomical variant was beneficial because it worked as an arterial graft for the LAD; therefore, the ischemic consequences only affected the myocardial territory supplied by the circumflex artery. Without this variant, the patient would have had a worse clinical condition due to the severe LCA disease plus left dominance, which behaves like severe triple-vessel disease; however, this natural hemorheological adjustment explains the reversible perfusion defect found only in the inferolateral wall and minimized the risk during the percutaneous coronary intervention.
The LAD is the coronary artery with the most consistent origin, course, and distribution in the human heart.2 Normally it is the continuation of the LCA and runs along the anterior interventricular sulcus to the apex; however, some anatomical variants have been described that do not compromise the normal blood supply to the corresponding myocardial territory.1,2
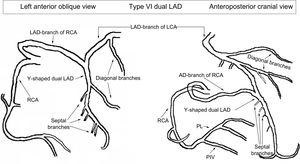
In 1983, Spindola-Franco et al.2 described and classified the dual LAD for the first time. Types I, II, and III are those with a bifurcation in the proximal segment, dividing the LAD into 2 branches, a short and a long branch,1,2 and in types IV and V, the long (or the short) branch has an anomalous origin from the RCA or close to it.3
Other variants and subtypes have been proposed,4 but none have described an anatomical distribution in which the branch that comes off the RCA converges with the LAD to form this single vessel that would usually supply the apex. For this reason, we describe it as a Y-shaped confluent dual LAD.
The importance of familiarity with all the dual LAD variants has significant implications in clinical practice and can be a powerful tool for interventional cardiologists and cardiovascular surgeons; therefore, it raises the question: is this anatomical variant really a congenital coronary anomaly or is it the result of a collateral circulation, stimulated by the severe LCA stenosis?
If the answer is the latter, it could be part of Vieussens anastomotic ring,5 which, in certain clinical or anatomical circumstances, such as ischemia, develops to increase the volume of blood flow to help the myocardial territory corresponding to the LAD; however, the branch coming off the RCA does not have the tortuous character or microvascular anastomoses (capillary network) of a collateral circulation, its caliber is similar to or larger than that of the other epicardial arteries, and its confluence with the LAD proper, at the level of the anterior interventricular sulcus, occurs much more distal than the emergence of the second diagonal branch.
To date, in all the known types of dual LAD, the long and short branches are divergent or have independent origins (ostia),1–4 but never before has an anatomical variant with convergent or confluent branches been described, such as the case presented here (Figure 2). Thus, it could be proposed as a type VI in the modified classification by Spindola-Franco et al.,2 although we cannot rule out that it may be a collateral circulation secondary to the LCA lesion.