Keywords
INTRODUCTION
The rupture of an atheromatous plaque in association with a variable degree of thrombosis, in relation to a local inflammatory process, is the underlying origin of acute coronary syndrome.1-3 There is a certain range of severity of coronary lesions, as well as a range of thrombogenic response.4 Although acute myocardial infarction is generally associated with obstructive coronary artery disease, between 8% and 12% of patients have normal coronary arteries.5-12 The differences in prevalence between published series arise, in part, because of the characteristics of the population included, such as the type of infarction (with or without ST elevation), whether troponin levels are used to define the infarction, or whether unstable angina with normal troponin levels is included. In terms of prognosis, there is a certain heterogeneity in the results. Although prognosis is better than for patients with obstructive coronary artery disease, there is a lack of agreement on how benign the disease is.8,10-15 The lack of a control group with which to compare the natural history has probably helped fuel this controversy.
The objective of our study was to analyze the characteristics related to coronary angiography showing no significant stenosis in a consecutive series of patients with non-ST elevation myocardial infarction (NSTEMI), who underwent cardiac catheterization during admission to hospital. In addition, long-term follow-up was conducted and the factors related to prognosis were analyzed. Finally, the disease course was compared with that of a control group of patients who were admitted for chest pain of possible coronary origin and who had normal troponin levels and normal coronary arteries.
METHODS
Study Group
The study included 504 consecutive patients who attended our hospital for chest pain and were admitted with diagnosis of NSTEMI between January 20, 2001 and April 1, 2008. The following criteria had to be met for inclusion in the study: a) no persistent ST elevation in the initial cardiogram; b) elevated troponin I in serial measurements on arrival at hospital and 8-12 hours after the onset of pain; c) no prior history of significant coronary artery stenosis determined by coronary angiography; and d) cardiac catheterization and coronary angiography during admission. The study population accounted for 62% of all patients admitted for NSTEMI without prior significant coronary artery stenosis recorded during the study period; the remaining 38% of the population did not undergo catheterization.
In our hospital, 2 different troponin I tests were used during the study: Immulite (Diagnostic Products Corporation, Los Angeles, California, US; upper limit of normal, 0.5 ng/mL) until October 2003 and Dimension (Dade Behring, Newark, Delaware, USA; upper limit of normal, 0.2 ng/mL) thereafter. The management of the patients and the indication for catheterization were according to the judgment of the attending cardiologist.
Variables Recorded
The following clinical variables were recorded for each patient: including coronary risk factors (age, smoking habit, hypertension, hypercholesterolemia, diabetes mellitus, family history), history of myocardial infarction, peripheral artery disease, stroke, and prior antiplatelet therapy. An ST-segment depression was recorded if more than 1 mm decrease ocurred, compared to the initial electrocardiogram (ECG). In all patients, creatinine was measured on admission and renal failure defined as levels greater than 1.3 mg/dL. Coronary stenosis was considered significant if it exceeded 50% in one of the 3 main epicardial vessels or the left coronary artery.
Objectives
The primary objective was to analyze the factors predictive of the absence of significant coronary stenosis (>50%). The secondary objective was to determine total mortality or acute myocardial infarction during follow-up. The median follow-up period was 3 years (interquartile range, 64-184 weeks). Follow-up exceeded 6 months in 97% of the patients and 1 year in 91%.
Control Group
Prognosis in patients with NSTEMI and normal coronary arteries was compared with that of a control group of 160 consecutive patients who were admitted during the same period for chest pain of possible coronary origin according to the judgment of the cardiologist on duty. These patients had normal troponin I levels, and the coronary angiography performed during hospitalization showed lack of significant coronary stenosis. In total, 37 patients showed ST-segment depression (>1 mm) in the initial ECG; 13 had a negative T wave (>1 mm), and 10 had left bundle branch block. Coronary angiography was done directly in 94 patients. For the remaining patients, prior to catheterization, exercise testing was done in 59 patients (28 with a positive result and 31 with an inconclusive result), and magnetic resonance imaging with dipyridamole in 15. The diagnosis on discharge was, in all cases, chest pain of unknown origin.
Statistical Analysis
The variables associated with the primary objective were analyzed using the c2 test. In order to transform age into a qualitative variable, its association with the primary outcome measure was analyzed using quartiles and the cutpoint corresponding to the upper limit of the first quartile (55 years) was chosen for its greater discriminative power. A multivariate logistic regression analysis was subsequently performed with the variables that were associated with the primary endpoint in the univariate analysis with P£.1. The entry criterion in the model was P<.05. Odds ratios (OR) and 95% confidence intervals (CI) were calculated.
For the secondary objective, a univariate analysis using a c2 test was performed, along with a multiple Cox regression (backward conditional method) with the variables of prognostic value in the univariate analysis. The hazard ratio (HR) and corresponding 95% confidence intervals (CI) were calculated.
Statistical significance was set at a value of P less than .05. The SPSS statistical analysis program, version 9.0 (SPSS Inc., Chicago, Illinois, USA) was used.
RESULTS
Characteristics of the Study Population
Table 1 shows the characteristics of the study population. Normal coronary arteries were observed in 64 patients (13%; 95% CI, 15.6-9.7). Sixty-five patients (13%) died during follow-up, 80 (16%) had an acute myocardial infarction, and 122 (24%) had an acute myocardial infarction or death.
Factors Related to Normal Coronary Angiogram
Table 1 shows the differences in the baseline characteristics between patients with and without significant coronary stenosis. Table 2 shows the results of the multivariate analysis. Female sex was the variable most strongly associated with absence of significant coronary stenosis (OR=6.6; 95% CI, 3.5-12.5; P=.0001). Other variables were age less than 55 years (OR=3.0; 95% CI, 1.5-5.8; P=.001), absence of diabetes (OR=2.4; 95% CI, 1.2-4.8; P=.02), prior antiplatelet therapy (OR=3.9; 95% CI, 1.5-10.2; P=.007), and presentation without ST-segment depression in the ECG (OR=2.4; 95% CI, 1.2-4.4; P=.008). The C statistic for the model with the 5 variables was 0.80, indicating an optimum predictive capacity.
In order to assess what proportion of patients were appropriately classified with the model, a variable indicative of high probability of coronary arteries without significant stenosis was created. This consisted of being a woman (given the greater OR) and at least another 2 of the 4 remaining variables. This variable identified a coronary angiogram without significant stenosis with a specificity of 85% and a sensitivity of 53%.
Prognosis of Acute Non-ST-Elevation Myocardial Infarction With Normal Coronary Arteries
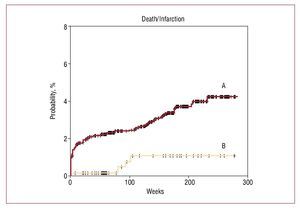
In the NSTEMI population, the lack of significant coronary artery stenosis was associated with a lower rate of death or infarction during follow-up (6% vs 27%; P=.0001) after adjusting for other variables of prognostic value (HR=0.3; 95% CI, 0.2-0.9; P=.03) (Figure). The other associated variables were heart failure on admission (HR=2.6; 95% CI, 1.7-4.0; P=.0001), age (per year, HR=1.02; 95% CI, 1.0-1.04; P=.05), diabetes mellitus (HR=1.5; 95% CI, 1.0-2.2; P=.04), prior myocardial infarction (HR=1.6; 95% CI, 1.1-2.4; P=.03), and renal failure (HR=1.7; 95% CI, 1.1-2.6; P=.02).
Figure. Kaplan-Meier curves for death or myocardial infarction according to presence of normal coronary arteries or significant stenosis. A: coronary stenosis; B: coronary arteries without significant stenosis.
The outcomes for the patients with NSTEMI and normal coronary arteries were compared with those of the control group. Table 3 shows the baseline differences between the 2 groups. Patients in the control group were older and more frequently had hypercholesterolemia and prior treatment with antiplatelet agents. Likewise, there was a tendency toward a greater proportion of men and systemic hypertension. During follow-up, among the entire population of patients with normal coronary arteries (n=224), 23 patients (10%) died or had an infarction. The death rates and rates of infarction in the subgroup with elevated troponin and normal troponin were 4 (6%) and 19 (12%) (HR=0.7; 95% CI, 0.2-2.2; P=.6).
DISCUSSION
In our series, we found that 13% of the patients with NSTEMI lacked significant coronary stenosis according to the coronary angiogram procedure performed during the initial stay in hospital. Female sex, younger age, absence of diabetes, and prior antiplatelet treatment, and presentation without ST-segment depression in the ECG were the variables associated with coronary angiography showing no significant lesions. The long-term prognosis of this population was good.
Prevalence of NSTEMI and Normal Coronary Arteries
The frequency of myocardial infarction and normal coronary arteries reported in the literature ranges from 8% to 12%.8,11,12,16,17 The differences in prevalence between the studies could depend on the different characteristics of the populations studied. Thus, in some series troponin is not used as a marker of necrosis, while others include patients if they have an ECG consistent with diagnosis of acute coronary syndrome in absence of elevated necrosis biomarkers. In addition, all studies represent the subgroup of patients with NSTEMI selected for catheterization, and the criterion used for this selection, whether broader or more restrictive, can also influence the angiographic results obtained. In the present study, diagnosis of infarction was done with troponin and catheterization was indicated in 62% of the patients with NSTEMI; this rate of catheterization is congruent with normal clinical practice in Spain for NSTEMI.18
Factors Predictive of Acute Non-ST-Elevation Myocardial Infarction With Normal Coronary Arteries
Female sex was the variable most strongly associated with absence of significant coronary artery stenosis. Other associated factors were age less than 55 years, absence of diabetes, lack of prior antiplatelet treatment, and presentation without ST-segment depression in the ECG. The predictive model with these 5 variables showed an optimal discriminative power (C statistic = 0.80). In addition, we constructed a simple model consisting of an obligatory variable (female sex) and at least 2 of the 4 remaining variables. This simple model allowed us to identify a coronary angiogram without stenosis with good specificity (85%), although the sensitivity was low (53%).
Age and female sex are the predictive variables detected in other studies.8,11,17,19 In the PURSUIT study, a model was developed for predicting normal coronary angiography. This model included the variables of female sex, younger age, and absence of elevated necrosis markers, prior angina, diabetes, or ST-segment depression.11 In that study, unlike ours, patients were included without elevated necrosis markers.
Prognosis
The lack of significant coronary artery stenosis was associated with better prognosis within the NSTEMI population. While there is agreement about the lower risk in patients with NSTEMI who have normal coronary arteries,15 their prognosis in the long term is subject of some debate.8,10-13,16,17,19,20 Thus, some series question the good prognosis of these patients.10,13,16 In our series, the long-term prognosis was better than that of the remaining patients with NSTEMI and similar to those of patients with chest pain, without elevated troponin levels and coronary angiography showing no significant stenosis. These data reinforce the good prognosis of this entity.
Mechanisms
Several mechanisms might explain why some patients with NSTEMI had no significant stenosis in the coronary angiogram, such as a thrombotic process that has already resolved when catheterization is done, microvascular dysfunction, or coronary embolism.19,21-24 This could also underlie substantial arterial disease that leads to an eccentric expansion of the atherosclerotic plaque that cannot be detected by coronary angiography.5-7 However, only a minority of patients have etiologic factors related to myocardial infarction and normal coronary arteries. Thus, a vasospasm test with ergonovine was positive in 15% of the patients and a coagulation disorder was detected in 12%.13
CONCLUSIONS
Clinical practice guidelines recommend an early invasive strategy in NSTEMI.25 In our study, we found coronary arteries without significant stenosis in 13% of the patients with NSTEMI and associated factors have been identified. Likewise, a predictive model has been constructed. Although this information could be relevant for assessing the strategy of systemic cardiac catheterization in certain patients with a high probability of normal coronary angiography, the predictive model has not been compared with any external cohort, and so it is hard to gauge its true usefulness.
Limitations
As the primary objective was to analyze the variables predictive of coronary arteries without significant stenosis, patients were excluded with a prior documented history of coronary artery stenosis. In addition, catheterization was indicated according to the judgment of the attending cardiologist. All these factors might have influenced the proportion of patients whose coronary angiogram showed no significant stenosis. Finally, the small number of patients in the group without significant coronary artery stenosis (n=224), where comparison is made between the subgroup with NSTEMI and the control group with normal troponin, means that any conclusions concerning the relationship with the prognostic value of troponin should be drawn with caution.
ABBREVIATIONS
CI: confidence interval
HR: hazard ratio
NSTEMI: non-ST-elevation myocardial infarction
OR: odds ratio
This study was supported by a grant from the HERACLES Cardiovascular Research Network (RD06/0009 Ministry of Science and Innovation, Instituto de Salud Carlos III, Madrid, Spain). Drs Juan Sanchis, Vicent Bodí, Julio Núñez, Luis Mainar, and Ángel Llácer also received grant support from FIS PI070640 (Instituto de Salud Carlos III, Madrid, Spain).
Correspondence: Dr. J. Sanchis.
Servicio de Cardiología. Hospital Clínico Universitario. Blasco Ibáñez, 17. 46010 Valencia. España.
E-mail: Sanchis_juafor@gva.es
Manuscript received November 28, 2008.
Accepted for publication July 7, 2009.