To the Editor,
We describe the case of a 77-year-old woman, ex-smoker, with mild emphysema, and bronchial hyperreactivity, admitted 2 years earlier at another hospital for bronchospasm with severe concomitant heart failure, who required treatment with vasoactive amines and ventilation support. The clinical condition was associated with generalized T-wave negativity, inversion mild enzyme elevation and alterations in cardiac contractility assessed as "consistent with myopericarditis"; the symptoms had all resolved at the time of discharge.
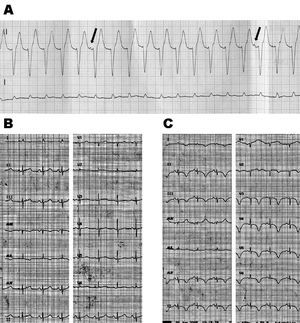
The patient was asymptomatic when she suddenly experienced sudden severe exertional dyspnea followed shortly afterwards by cardiorespiratory arrest. Basic cardiopulmonary resuscitation maneuvers were started immediately, followed by advanced maneuvers at 3 min. After monitoring the patient, sustained monomorphic ventricular tachycardia at 150 bpm was observed (Figure 1A); electrical cardioversion was applied and sinus rhythm recovered (Figure 1B). The patient was hemodynamically stable upon arrival to the emergency room. Echocardiography showed akinesia of the apical and middle segments with a left ventricular ejection fraction of 25%. Creatine kinase and troponin I concentrations were initially normal, but increased at 12 h to 374 U/L and 3.6 µg/L, respectively. NT-pro-BNP, a marker of acute heart failure,1 was raised to 15 944 pg/mL.
Figure 1. A: sustained monomorphic ventricular tachycardia with atrioventricular dissociation (arrows). B: ECG in sinus rhythm at the time of admission. C: ECG on day 2, showing deep, extensive T-wave negativity, and QT interval prolongation.
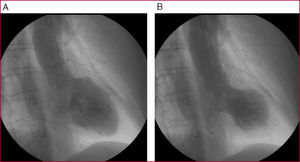
Clinical progress was favorable with diuretic and inotropic treatment. An electrocardiogram performed at 48 h shown deep, generalized T-wave inversion with QT interval prolongation (Figure 1C). The patient underwent catheterization, with no significant coronary lesions observed. Left ventriculography showed severe systolic dysfunction in the apical and middle segments (Figure 2). The endomyocardial biopsy was nonspecific.
Figure 2. Ventriculography at third day of hospitalization. A: end-diastole. B: end-systole; an apical aneurysm is evident, with normal contractility of the basal segments.
On day 6 post-admission, the patient underwent an electrophysiological study. Sustained ventricular tachycardia with 2 extrastimuli was induced, and on the basis of these findings, an automatic defibrillator was implanted. At the time of discharge, she presented mild apical hypokinesia with left ventricular ejection fraction of 55% and electrocardiographic persistence of negative T-wave, which had normalized in the 4-month follow-up.
Transient apical ballooning can simulate an acute coronary syndrome due to the onset of chest pain or sudden dyspnea and ECG alterations. It is characterized by transient akinesia of the apical and middle segments of the left ventricle with absence of significant coronary lesions.2.3 The condition mainly affects elderly women (82%-100%) and is usually associated with emotional or physical stress. A relationship with strenuous physical exertion and episodes of asthmatic bronchitis has been reported.2,4
Between 3% and 46% of patients develop severe acute heart failure. The majority recover ventricular function within 2-3 weeks. Associated tachycardia and/or ventricular fibrillation5 is described in 9% of patients, with the origin possibly related to the etiology (transient ischemia or catecholaminergic release) or the consequences of transient apical ballooning (QT interval prolongation, ventricular dysfunction).
Over the long-term, the condition can recur in up to 8% of patients.5 In our case, the patient presented a clinical picture consistent with transient apical ballooning two years before, which had been attributed to myopericarditis.
Therefore, transient apical ballooning should be considered in the differential diagnosis of ventricular arrhythmia and sudden death, particularly after physical or emotional stress.