To the Editor,
Congenital pulmonary artery agenesis is a rare cardiovascular malformation, frequently oligosymptomatic,1,2 that can be complicated with unilateral pulmonary edema3 or pulmonary hypertension.1,2,4 We report the case of a patient with congenital pulmonary artery agenesis and pulmonary hypertension who developed unilateral pulmonary edema and discuss the role of sildenafil in pulmonary hypertension.
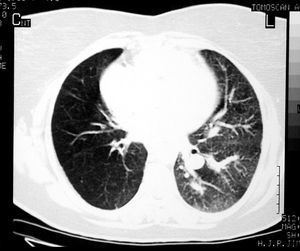
A 47-year-old woman, smoker of 20 cigarettes/day, with recurrent pulmonary infections, consulted for a hypertensive crisis. The physical examination was normal. The hemogram, biochemistry, coagulation tests, and electrocardiogram showed no alterations; there was mild hypoxemia in the arterial blood gas study. The chest x-ray revealed right pulmonary hyperlucency and a prominent left pulmonary artery. The echocardiogram showed concentric left ventricular hypertrophy with normal systolic function and dilation of the right ventricle with tricuspid regurgitation of 4.55 m/s. Pulmonary scintigraphy (ventilation-perfusion) disclosed the absence of right pulmonary perfusion. Computed tomography of the chest ruled out pulmonary thromboembolism, extrinsic compression of the pulmonary artery, and unilateral emphysema. The left pulmonary parenchyma showed a mosaic pattern and the right was hyperaerated (Figure 1). The respiratory functional tests showed mild obstruction with a moderate reduction of diffusion. Other causes of pulmonary hypertension were ruled out, and the patient was discharged. Two weeks later, the patient was readmitted for frank left ventricular failure. Blood pressure was 190/80 mm Hg, the ambient air saturation was 47%, and left crepitant rales were detected in the pulmonary auscultation. The ECG showed sinus tachycardia. A chest x-ray (Figure 2) revealed a left alveolar infiltrate, and the patient was started on oxygen therapy, nitroglycerin, furosemide, and antibiotics. She was clinically stabilized within 24 h, and the infiltrate disappeared. The hemodynamic study showed the following: pulmonary arterial pressure 87/25 mm Hg (mean, 49), right ventricular pressure 91/10 mm Hg, pulmonary capillary pressure 7 mm Hg, and blood pressure of 119/61 mm Hg (mean, 85). Oxygen saturation in venous blood was 56.5%, with no evidence of shunting. The pulmonary arteriography showed dilation of the main artery and of the left pulmonary artery and branch with absence of the right pulmonary artery. From the descending thoracic aorta and the right coronary, collateral "bronchial" arteries arose toward the right lung. The coronary arteries showed no lesions. She was discharged with oxygen, nifedipine, furosemide, enalapril, and coumarin derivatives, agreeing to an indication of cardiopulmonary transplantation at a referral hospital. Twenty months later, the patient worsened (New York Heart Association class III dyspnea); the 6-min walk test was 362 m and tricuspid regurgitation, estimated by echocardiography, was 3.5 m/s. Treatment with sildenafil (50 mg/24 h) was started with evident clinical improvement, remaining at 12 months in functional class II with a 6-min test of 428 m. Systolic pulmonary pressure estimated by echocardiographic study was 30 mm Hg.
Figure 1. Chest computed tomography reveals a mosaic pattern in the left lung and hyperlucency in the right.
Figure 2. Chest x-ray shows left pulmonary edema.
Unilateral pulmonary edema is seen in various clinical scenarios. It is classified as ipsilateral or contralateral,3 with the latter occurring in the opposite lung to the perfusion defect. Patients with congenital pulmonary artery agenesis can present contralateral unilateral pulmonary edema during heart failure.
It is estimated that 19%-25% of patients with congenital pulmonary artery agenesis present pulmonary hypertension1,2 in adulthood,1,4 which implies a poor prognosis.2,4 Production of nitric oxide, which has a vasodilator and antiproliferative effect on the pulmonary artery, is poor in pulmonary hypertension.5 Sildenafil inhibits the enzyme that degrades nitric oxide (PDF-5) and results in long-term hemodynamic and functional improvement in patients with pulmonary hypertension due to various conditions,5,6 without deteriorating the ventilation/perfusion ratio6 and even improving it (supraselective or exclusive vasodilation effect in ventilated pulmonary areas).7 In our case, sildenafil treatment improved the patient's functional capacity and normalized the hemodynamic parameters, probably because of a selective and supraselective vasodilator effect.
In conclusion, unilateral pulmonary edema can complicate the clinical progress in adults with congenital pulmonary artery agenesis. Add-on therapy of pulmonary hypertension with sildenafil should be considered in this clinical context.