The incidence of pulmonary embolism (PE) has been on the rise in Spain and other European countries, potentially influenced by factors such as longer life expectancy and the presence of conditions that increase the risk of venous thromboembolism.1,2 Other factors that could have contributed to the observed increase are improved diagnostic methods and increased awareness of PE. However, despite the higher incidence, in-hospital and age-standardized mortality rates have decreased in Spain, suggesting improved identification of low-risk cases and advancements in treatment.3,4 Age-standardized mortality rates (ASMRs) have generally decreased in European Union countries, including Spain.4 Nevertheless, previous studies on PE mortality in Spain have primarily focused on older age groups, necessitating an examination of all age groups and the differentiation of younger populations.
This study collected data on population and PE-related deaths from the National Institute of Statistics in Spain, covering the period from 1999 to 2021. International classification of diseases (ICD-10) codes, including “acute pulmonary embolism with or without acute cor pulmonale” (I26) and nonfatal venous thromboembolic (VTE) manifestations (eg, deep vein thrombosis [DVT] or phlebitis/thrombophlebitis), were used to identify PE-related deaths, as used in previous studies.5 ASMRs were calculated using the European standard population. We used joinpoint regression models to identify significant changes in mortality trends and calculated annual percentage changes (APC) for each segment. To assess the overall trend from 1999 to 2021, we derived a geometrically weighted average of the different APCs, providing a concise summary of the overall trend.
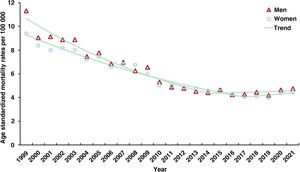
Figure 1 depicts the ASMRs (all ages) due to PE in Spain from 1999 to 2021 by sex. The ASMRs demonstrated a significant decrease in both sexes, with an APC of −3.8% in men and −3.3% in women. From 1999 to 2021, ASMRs decreased from 11.3 to 4.8 deaths per 100 000 person-years for men and from 9.4 to 4.5 deaths per 100 000 person-years for women. For both men and women, a change in the trend occurred in 2014 for men and in 2017 for women, marking a division between 2 distinct trends. Initially, there was a substantial annual decline in mortality rates for both males (−5.8%) and females (−4.5%). This positive trend was followed by a subsequent period of stabilized rates for both sexes.
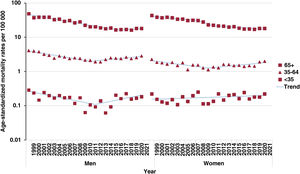
Figure 2 illustrates the truncated ASMRs for different age groups (< 35, 35-64, and ≥65 years) by sex. Globally, rates remained stable in the population aged <35 years, but with differences in the pattern between sexes. A detailed joinpoint analysis showed a significant change in trend among males in 2012, with an initial decrease (−6.6%) followed by stabilization. Females in this age group did not show a significant change in trend. Overall, in the group aged 35 to 64 years, rates decreased for men but remained stable for women. The joinpoint analysis identified a turning point in 2011 for men and in 2010 for women, dividing the study period into 2 phases: an initial decline (−5.6% for men and −4.3% for women), followed by a period of increasing rates (3.3% for men and 3.4% for women). In the group aged ≥65 years, rates decreased steadily throughout the study period for both men and women (−4.2% and −3.6%, respectively). Joinpoint analysis for men revealed a turning point in 2016, indicating an initial period of decline (−5.9%), followed by stabilized rates. For women, 2 turning points were observed (in 2008 and 2011), indicating an initial decline (−3.6%), followed by stabilization and subsequent decline (−2.3%).
Throughout most of the study period, PE ASMR was higher in men than in women, particularly in the group aged 35-64 years.
These findings align with those of similar studies conducted in the United States, which reported a stabilization or increase in PE mortality rates in recent years.5 PE-related mortality in adults aged 25 to 44 years has increased over the last 2 decades in the United States.6
Improved disease management, including the use of advanced therapies and interventions, such as anticoagulants and surgical procedures, may have contributed to the declining trend in PE-related mortality. However, PE remains a significant contributor to overall mortality, highlighting the need for awareness campaigns and improved management of this preventable condition.
This study also observed a reversal or stabilization of trends in certain age groups and sexes since the early 2010s. These trends may have been influenced by factors such as increased obesity rates and other risk factors like smoking, trauma, and hormone therapies.
Due to the lack of incidence data, we rely on mortality data, as in similar studies. However, when interpreting trends, it is important to recognize the impact of small numbers of deaths on estimates in certain age and sex groups. On the other hand, we would like to emphasise that the chosen method of analysis is still relevant and is used in epidemiological studies. Despite their limitations, epidemiological mortality studies are essential for understanding disease burden and its determinants.
In conclusion, this study highlights the ongoing need for efforts to prevent, detect, and treat PE effectively, especially in specific age and sex groups with higher PE-related mortality rates. Including PE in global mortality estimates could support these efforts and help assess the effectiveness of interventions. Further research is necessary to understand the underlying factors driving recent trends in PE mortality and evaluate the role of risk stratification, treatment specifications, and adherence to guidelines in hospitals.
FUNDINGThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ETHICAL CONSIDERATIONSIn compliance with the regulations and ethical principles established by the Committee on Publication Ethics (COPE), our study was conducted with integrity and transparency. Since the data extracted from the National Institute of Statistics were anonymized, our study conforms to the principles of good clinical practice and complies with the Declaration of Helsinki. To carry out this study, it was not necessary to request informed consent from the individuals or approval by an ethics committee, since the aggregate data is anonymous. In this regard, we confirm that all data were anonymized, and that no personal information was accessed during the research process. Both the design and the results of the study were carried out based on sex following the international guidelines of the SAGER guidelines. We were unable to follow the international guidelines of the SAGER guidelines based on gender as this information is not available in the data obtained.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCEArtificial intelligence has not been used to carry out this work.
AUTHORS’ CONTRIBUTIONSAll authors contributed to the conception and design of the work; the acquisition, analysis, and interpretation of data; drafting the work and revising it critically for important intellectual content; approval of the version to be published; and are responsible for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are properly investigated and resolved.
CONFLICTS OF INTERESTL. Jara-Palomares reports personal fees from Bayer Hispania, Actelion, Rovi, Pfizer, Menarini, and Leo Pharma, outside the submitted work. The other authors have no conflicts of interest to declare regarding this manuscript.