Coronary artery obstruction (CAO) is an uncommon complication of transcatheter aortic valve replacement (TAVR), with an incidence of less than 1%. Preemptive action is essential, as CAO is associated with high in-hospital mortality (30%-50%).1 CAO occurs when the percutaneously implanted valve displaces the native or prosthetic valve leaflets towards the coronary ostium or the sinotubular junction and “sequesters” the sinuses of Valsalva. The most common technique used to prevent CAO in high-risk patients is coronary protection with an angioplasty guidewire and chimney stenting. The technique, however, is associated with long-term complications,2 such as stent thrombosis and future difficulties accessing the coronary circulation for selective catheterization. These limitations have prompted the search for alternative CAO prevention methods. One noteworthy technique is BASILICA, which stands for bioprosthetic or native aortic scallop intentional laceration to prevent iatrogenic coronary artery obstruction (figure 1).3 Although the BASILICA technique is promising, little has been published on its effectiveness in Spain. The aim of this study was to describe preliminary outcomes in patients at high risk of CAO who underwent BASILICA during TAVR.
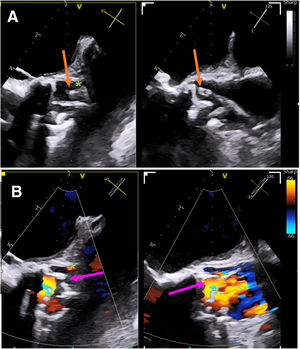
Transesophageal echocardiographic images acquired during the BASILICA procedure (short-axis view of aortic valve with biplanar imaging). A: the arrows show the tip of the catheter over the aortic cusp before laceration; the asterisk shows the left main coronary artery. B: the arrows show the lacerated cusp.
We studied 13 consecutive patients at high risk for CAO who underwent the BASILICA procedure during TAVR at our hospital between December 2021 and March 2023. These patients accounted for 4.1% of all patients who underwent TAVR during this period. The study was approved by the ethics committee of our institution and all patients provided signed informed consent. Baseline characteristics, procedure details, and long-term follow-up events are summarized in table 1. Most of the patients (77%) were women. Computed tomography (CT) was used to identify high-risk features for CAO,3 namely, low origin of coronary artery (<10mm), cusp height < coronary artery height, virtual valve-to-coronary artery distance <4 mm, and, in the case of native valve procedures, calcium volume in the culprit cusp >600 m2 based on the threshold established by Khan et al. in 2023.3 Prior to this, calcium volume was assessed qualitatively. In all patients, the procedure was performed under general anesthesia with orotracheal intubation and transesophageal echocardiographic monitoring. BASILICA was performed on a bioprosthetic aortic valve (valve-in-valve procedure) in 4 patients (31%). Overall, the technique was successful in 12 (92%) of the 13 patients. It failed in 1 patient undergoing a valve-in-valve procedure who had a severely calcified prosthetic cusp that could not be lacerated. Self-expanding valves were used in 77% of patients. A protective guidewire was implanted in 54% of procedures, but chimney stenting was not necessary. Two patients developed procedure-related complications: 1 uncomplicated aortic intramural hematoma (without coronary obstruction or aortic dissection), which resolved completely, and 1 transient ST-segment elevation. TAVR was successful in all patients. None of the patients developed CAO or required bailout treatment with chimney stenting. Subsequent coronary catheterization was performed successfully and without complications in all patients. There were no deaths or cardiovascular events (including delayed CAO) over a median follow-up of 7.6 months [4.9-13.1] months. During follow-up, 1 patient was admitted for a pseudoaneurysm requiring surgical intervention at the primary femoral access site.
Baseline patient characteristics, procedure characteristics, and follow-up events
| Total(n=13) | |
|---|---|
| Baseline characteristics | |
| Age, y | 80 [75-82] |
| Female | 10 (77) |
| Previous stroke | 1 (8) |
| Previous ischemic heart disease | 7 (54) |
| Previous GFR, mL/min/m2 | 1.12 [1.03-1.5] |
| NYHA class >II | 12 (93) |
| EuroSCORE II, % | 5.9 [2.6-13.7] |
| STS score | 6.08 [3.2-12.8] |
| Echocardiogram and computed tomography characteristics | |
| LVEF, % | 55 [37-60] |
| Peak aortic gradient, mmHg | 88 [66-110] |
| Mean aortic gradient, mmHg | 48 [40-70] |
| Aortic valve area, cm2 | 0.76 [0.58-0.85] |
| Coronary artery height, mm | 8 [6-8.9] |
| Cusp height, mm | 11.3 [10.5-12.8] |
| Cusp height >coronary artery height, % | 13 (100) |
| Virtual distance from TAVR prosthesis to coronary artery, mm | 3.3 [2.7-5] |
| Calcium volume in culprit cusp, mm3 | 398 [217-511] |
| Eccentric ostium (>15°) | 0 |
| Procedure characteristics and complications | |
| Valve-in-valve | 4 (31) |
| Left cusp | 13 (100) |
| Successful BASILICA | 12 (92) |
| Predilation | 7 (54) |
| Cerebral embolic protection | 7 (54) |
| Transcatheter aortic valve implanted | |
| Self-expanding | 10 (77) |
| Balloon-expandable | 3 (23) |
| Prosthetic valve size, mm | 25 [23-25.5] |
| Use of coronary guidewire protection, % | 7 (54) |
| Chimney stent implantation | 0 |
| Successful TAVR | 13 (100) |
| Procedure time, min | 208 [168-237] |
| Fluoroscopy time, min | 58 [47-73] |
| Contrast, mL | 187 [140-280] |
| Intraprocedural complicationsa | 2 (15) |
| Definitive pacemaker implantation | 2 (16) |
| Aortic valve regurgitation ≥moderate | 0 |
| Medium-term events; median follow-up, 7.6 [4.9-13.1] mo | |
| Mortality | 0 |
| Cerebrovascular accident | 0 |
| Coronary artery obstruction | 0 |
| Acute myocardial infarction | 0 |
| Endocarditis | 0 |
| Mean gradient, mmHg | 10 [7-13] |
| Aortic valve regurgitation ≥moderate | 0 |
BASILICA, bioprosthetic scallop intentional laceration to prevent coronary artery obstruction; GFR, glomerular filtration rate; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; STS, Society of Thoracic Surgery; TAVR, transcatheter aortic valve replacement.
Values are expressed as No. (%) or median [interquartile range].
Careful patient selection using CT scanning is crucial for preventing CAO during TAVR. Several anatomic and procedure-related factors have been linked to an increased risk of CAO.3 Surgical aortic valve replacement is the method of choice for patients with a high risk of CAO, but prohibitive risk precludes surgery in a significant number of patients. The alternative is to perform TAVR and accept the risk of CAO. One method for mitigating risk is prophylactic coronary prevention with a guidewire and placement of a chimney stent to be deployed in the event of obstruction. The stent, however, can be deformed by the TAVR prosthesis, leading to thrombosis, long-term antithrombotic treatment, and the risk of harmful bleeding events and future engagement difficulties as the stent is left “floating” in the aorta. The BASILICA technique was developed to overcome these limitations.4 The safety and effectiveness outcomes observed for this technique in our series are similar to previous reports.5 Early experience, however, is limited, and randomized trials will be needed to demonstrate the true impact of BASILICA. The main limitations of our study are its small sample size and the absence of a control group. In conclusion, based on our preliminary effectiveness and safety findings, the BASILICA technique may be a promising alternative for patients at high risk of COA during TAVR.
FUNDINGNone.
AUTHORS’ CONTRIBUTIONSThe authors accept full responsibility for the content of this manuscript as defined by International Committee of Medical Journal Editors. A. Regueiro conceived the study and designed the analysis. P. Cepas-Guillén and R. Gabani conducted the analysis. A. Regueiro, M. Giménez-Milà, L. Sanchis, and X. Freixa revised and edited the manuscript.
CONFLICTS OF INTERESTP.L. Cepas-Guillen has a research grant from Hospital Clínic de Barcelona (Contractes Clínic de Recerca Emili Letang-Josep Font). A. Regueiro is a proctor for Abbott Vascular and Meril Life. L. Sanchis is an associate editor for Revista Española de Cardiología. The journal's editorial procedure was followed to guarantee the impartial handling of the manuscript. The rest of the authors declare no conflicts of interest.