Cancer and cardiovascular disease (CVD) are the leading causes of death in developed countries; this is particularly relevant considering that patients with cancer have a higher prevalence of CVD than the general population.1,2 The association between cancer and CVD is attributed to shared risk factors, such as age, smoking, obesity, and a sedentary lifestyle. In addition, the heart can be directly affected by cancer or its treatment. This interplay between cancer and CVD results in a complex clinical scenario potentially limiting the management of both diseases.3
As cancer therapies grow in number and range, we are seeing increasingly diverse cardiovascular adverse effects. Cancer therapy-related cardiotoxicity may require the interruption of otherwise effective treatments, negatively affecting prognosis. Prompt detection and treatment of cardiotoxicity in its early stages is therefore crucial.4
Specialist cardio-oncology-hematology (COH) units have emerged as a means of optimizing the treatment of CVD in patients with cancer and reducing the need to interrupt cancer therapy.5–7 The multidisciplinary nature of COH teams facilitates information sharing and improved decision-making.
Initiatives are needed to promote the creation of COH programs in order to standardize and implement strategies recommended by scientific societies for facilitating the detection and treatment of cardiovascular complications. COH is a new subspecialty, however, and its implementation still varies among hospitals and regions.8 To ensure that patients with cancer have equal access to COH care, it is essential to identify tools that promote best practices in this field.
SCIENTIFIC SOCIETY RECOMMENDATIONS AND QUALITY OF CARE INDICATORSRecommendations on the diagnosis and treatment of cardiovascular complications in patients with cancer have varied significantly over the years, as have the definitions of cardiotoxicity. Fortunately, a number of recent international guidelines and consensus statements have helped identify key issues, establish follow-up and treatment recommendations, and determine the main criteria for evaluating quality of care and specialist training in COH.
The first European guidelines on COH were published by the European Society of Cardiology (ESC) in 2022.4 The guidelines unified the criteria for diagnosing cardiotoxicity according to event type and severity and included recommendations on monitoring and treating cancer treatment-related cardiovascular toxicity. The ESC guidelines are the main point of reference used in the design of COH care protocols.
Another 2 more recent European documents published complementary information about 2 key aspects of COH: quality indicators and clinical competencies. The first document described the development and selection of ESC quality indicators for evaluating the prevention and management of cardiovascular toxicity induced by cancer treatment.9 Based on a systematic review of the evidence, the indicators cover 5 key domains: structural framework, baseline cardiovascular risk assessment, cardiotoxicity rates, cardiotoxicity treatment, and cardiotoxicity monitoring. The second document, the ESC Core Curriculum for cardio-oncology, is a consensus statement produced by specialists from various fields.10 It defines the experience and knowledge required for cardiologists to subspecialize in COH as well as the clinical competencies needed for research, evaluation, diagnosis, and treatment of cardiovascular disease in patients with cancer.
While it is important to consider international recommendations and expert opinions on COH, it is also important to adapt these to each country's health care system.11 To establish best practices and standards for COH units in Spain, the Spanish Society of Cardiology (SEC) set up a multidisciplinary committee to develop the SEC-Excellence accreditation program for COH. The committee included specialists in cardiology, hematology, medical oncology, radiation oncology, and family and community medicine.12
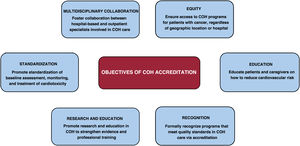
SEC-EXCELLENCE ACCREDITATION PROGRAM FOR COHThe SEC-Excellence accreditation program formally recognizes COH units that meet established quality standards with the ultimate goal of promoting high-quality care and best practices in the cardiovascular care of patients with cancer. Recognition must be given to the beneficial effects of COH units and the need for specialized training and multidisciplinary management. It is also important to secure sufficient resources to cover these needs and ensure the implementation of strategies recommended by leading scientific societies (figure 1).
From a care perspective, the SEC-Excellence accreditation program aims to create and optimize COH programs and secure the necessary material and human resources for their implementation. The objective is to ensure proper baseline stratification of cardiovascular risk during or after cancer treatment and to standardize the treatment of cardiotoxicity in its varying forms, ensuring equitable and appropriate management in each case.13 Improved identification, management, and monitoring of patients at increased risk of cardiovascular complications will help reduce these complications and enable their earlier detection; it will also require fewer interruptions to onco-hematology treatments. The aim is not only to facilitate and minimize interruptions to cancer treatment but also to prevent the onset and progression of CVD in patients with cancer, a particularly important consideration for long-term survivors.
The SEC-Excellence COH accreditation program also includes organizational criteria designed to enhance multidisciplinary collaboration in COH units. Recognition is given to the creation of organizational charts, multidisciplinary committees, and care pathways linking the different specialists and teams involved in patient care, including hospital departments, primary care,14 and occupational medicine.15 The goal is to facilitate smooth and rapid communication, thereby encouraging collaboration between different levels of care.
The SEC-Excellence COH accreditation program acknowledges that patients should be at the center of care. They should not only be informed about their condition and the associated risks but also be actively engaged in their health and care. They therefore need to be educated about everyday actions they can take to reduce their cardiovascular risk in the short-, mid-, and long-term. To this end, COH teams must offer patients and families educational resources.
The final goal of the SEC-Excellence accreditation program is to improve education and research in COH. Continuous professional development is crucial in this field. Initially, COH units focused on the early detection of cardiotoxicity manifesting as ventricular dysfunction or heart failure due to well-known treatments, such as anthracyclines and human epidermal growth factor receptor 2 targeted therapies. Over the years, however, the complexity of cancer treatments has increased dramatically, as has the range of potential cardiovascular adverse effects and associated treatment options.16 Education and training for health care professionals involved in COH care, whether subspecialists in this field or not, should include specific updates on COH.17 The scientific evidence is still limited. More than 70% of the recommendations in the 2022 ESC cardio-oncology guidelines are based on expert consensus.4,11 It is therefore important to foster research in COH to continue generating evidence on which to base routine clinical practice.
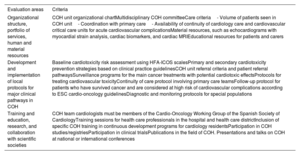
The main accreditation criteria used in the SEC-Excellence in COH program (table 1) were based on international recommendations and adapted to the Spanish health care system.
Summary of the main criteria used in the SEC-Excellence accreditation program for cardio-oncology-hematology (COH)
| Evaluation areas | Criteria |
|---|---|
| Organizational structure, portfolio of services, human and material resources | COH unit organizational chartMultidisciplinary COH committeeCare criteria- Volume of patients seen in COH unit- Coordination with primary care- Availability of continuity of cardiology care and cardiovascular critical care units for acute cardiovascular complicationsMaterial resources, such as echocardiograms with myocardial strain analysis, cardiac biomarkers, and cardiac MRIEducational resources for patients and carers |
| Development and implementation of local protocols for major clinical pathways in COH | Baseline cardiotoxicity risk assessment using HFA-ICOS scalesPrimary and secondary cardiotoxicity prevention strategies based on clinical practice guidelinesCOH unit referral criteria and patient referral pathwaysSurveillance programs for the main cancer treatments with potential cardiotoxic effectsProtocols for treating cardiovascular toxicityContinuity of care protocol involving primary care teamsFollow-up protocol for patients who have survived cancer and are considered at high risk of cardiovascular complications according to ESC cardio-oncology guidelinesDiagnostic and monitoring protocols for special populations |
| Training and education, research, and collaboration with scientific societies | COH team cardiologists must be members of the Cardio-Oncology Working Group of the Spanish Society of CardiologyTraining sessions for health care professionals in the hospital and health care districtInclusion of specific COH training in continuous development programs for cardiology residentsParticipation in COH studies/registriesParticipation in clinical trialsPublications in the field of COH. Presentations and talks on COH at national or international conferences |
COH, Cardio-Oncology-Hematology; ESC, European Society of Cardiology; HFA-ICOS, Heart Failure Association-International Cardio-Oncology Society; MRI, magnetic resonance imaging; SEC, Spanish Society of Cardiology.
COH accreditation is not just a stamp of excellence in COH care; it is an opportunity to promote the creation of new units and to improve existing ones, ultimately enhancing cardiovascular care for patients with cancer and improving the overall quality of health care services.
FUNDINGNone.
CONFLICTS OF INTERESTP. Moliner has received speaker fees, consultancy fees, or financial support for attending conferences from AstraZeneca, Bayer, Bristol, Novartis, Janssen, and Vifor Pharma. T. López-Fernández has received speaker or consultancy fees from Phillips, Bayer, Beigene, AstraZeneca, Myocardial Solutions, Daiichi-Sankyo, and Janssen.
The creation of the SEC-Excellence COH accreditation program was made possible by the efforts of a large number of individuals and scientific societies that recognized the significant impact the process would have on the quality of care for patients with cancer. We would like to thank the following individuals and organizations for their support and involvement in the project: the SEC, in particular the members of the SEC Executive Committee and the SEC-Quality program; the Spanish Society of Medical Oncology; the Spanish Society of Radiation Oncology; the Spanish Society of Hematology and Hemotherapy; and the Spanish Society of General and Family Medicine.
Members of the SEC: Antonio Castro, Nuria Coma, Teresa López-Fernández Rebeca Lorca, Ana Martín, Amparo Martínez-Monzonís, Pilar Mazón, Lola Mesa, Cristina Mitroi, Pedro Moliner, Nieves Romero, Eduardo Zatarain. Representatives of other societies: Javier de Castro (Spanish Society of Medical Oncology), Raúl Córdoba (Spanish Society of Hematology and Hemotherapy), Isabel Egocheaga (Spanish Society of General and Family Medicine), and Isabel Rodríguez (Spanish Society of Radiation Oncology).
The members of the SEC Scientific Committee for the accreditation of cardio-oncology-hematology units are listed in Appendix A.