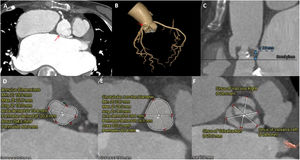
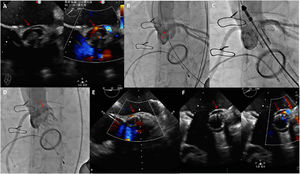
A 65-year-old Asian woman presented with severe aortic valve stenosis and a history of mechanical valve replacement for rheumatic mitral stenosis. Coronary computed tomography angiography revealed an anomalous origin of the left coronary artery (LCA) from the noncoronary cusp with an intramural course (figure 1A,B; arrows). The LCA was 8mm from the aortic annular plane (figure 1C). The diameters of the aortic annulus, sinotubular junction, and 3 sinuses of Valsalva were small (figure 1D-F). Transapical transcatheter aortic valve replacement with a J-valve self-expandable device (Genesis MedTech, China) was planned. The 3 U-shaped nitinol graspers of the J-valve surrounding the valve protected the coronary artery ostium and facilitated valve deployment. During the procedure, aortography was performed using a standard 3-cusp coplanar view; the projection angle was left anterior oblique 17°/caudal 2°. The anomalous origin of the LCA was confirmed by aortography and transesophageal echocardiography (TEE) (figure 2A,B; arrows). Postballoon valvuloplasty, 3 U-shaped graspers were placed in the 3 aortic sinuses (figure 2C) and a 21-mm transcatheter heart valve was deployed. Immediate aortography and TEE revealed LCA occlusion (figure 2D,E; arrow). A median sternotomy was performed and the aorta was opened. The self-expanding nitinol structure of the J-valve had occluded the LCA ostium. The J-valve was removed, the intramural aortic segment of the LCA was unroofed and expanded, and the J–valve was reimplanted through the aorta. TEE revealed unobstructed blood flow in the LCA ostium (figure 2F; arrows). Thus, anomalous origin of the LCA with a small aortic root can cause coronary artery occlusion during transcatheter aortic valve replacement.
The study was approved by the ethics committee of our institution. Informed consent was obtained from the participant.
FUNDINGNo financial relationships.
AUTHORS’ CONTRIBUTIONSAll authors have read and approved the manuscript and take full responsibility for the manuscript.
CONFLICTS OF INTERESTNo conflicts of interest.