Keywords
INTRODUCTION
Chagas disease (CD) is associated with infection caused by the protozoan Trypanosoma cruzi, and is commonly characterized by a chronic phase with cardiac and/or digestive involvement, observed in about 30% of infected individuals.1,2 In the first week of infection, a polyclonal B-cell activation occurs and the parasites induce a chemokine production by macrophages.3 This intensive response through parasite-induced chemokines, TNF-α and IL-12, leads to the activation of CD4+ and CD8+ T cells capable of producing γ-interferon and, as a consequence, to the destruction of the protozoan by nitric oxide derived from macrophages.4 Although chemokines and cytokines have a pivotal function in activation of the inflammatory process, necessary for parasite control, an excessive or uncontrolled heart inflammation may be associated with severe chronic forms of CD.1,5
The CRP is an acute phase protein, mainly synthesized in the liver and regulated by IL-6.6 The association of CRP to cardiovascular events, through the contribution to atherosclerotic lesions development, has been proven to arise from several biological pathways, such as complement activation,7 increased cell adhesion,7 enhancement of procoagulant activity,8 apoptosis regulation through the classical complement pathway and lipoprotein deposition in the plaque.9 Although an increasing number of studies corroborates the direct participation of CRP in the formation of atherosclerotic plaques, little information correlates this acute phase molecule to the development of heart failure and, more specifically, to Chagas disease.
The aim of this study was to establish the possible association of CRP levels and the progression of CD, suggesting a marker of clinical severity for the cardiac presentation in such patients.
METHODS
In the present study, 136 individuals were evaluated by the Chagas Disease Study Group of the UNICAMP University Hospital. All patients were aged between 20-60 years old and presented at least 2 positive serological results. Control groups (CT) for comparisons consisted of voluntary healthy blood donors and cardiac patients with negative CD serological tests (NCC), in the same age range. The Public Health Service in Brazil establishes regional patient services and the University Hospital of UNICAMP is a major center for complex tertiary care in the São Paulo state, which makes the population representative of that geographic area and socio-ethnic profile.
The conventional eletrocardiography was performed with patients at rest, using 12 leads. The echocardiography was performed using a Toshiba Xario® machine, with a 3.5 mHz transductor, according to the technical orientations of ACC/ AHA Guidelines for the Clinical Application of Echocardiography. A sistematic search for esophagopathies and colonopathies was made through diagnostic radiographic procedures with barium contrast in all patients with serologic positivity for CD.
The CD patients were firstly stratified in cardiac or indeterminate CD patterns, and the adopted criteria for the indeterminate CD (IND) were: a) serological positivity for CD; b) asymptomatic patients; c) normal thorax radiography; d) normal electrocardiograph; e) normal echocardiography; and f) absence of esophageal and/or colonic involvement.
Subsequently, the cardiac CD group was classified as mild cardiopathy (MC) (at least one of these findings: null or mild symptoms; atrioventricular first-degree block; intraventricular conduction abnormalities, defined as right bundle branch block and/or left anterior hemiblock; isolated and unifocal atrial extrasystole; isolated and unifocal ventricular extrasystole) and severe cardiopathy (SC) (at least one of these findings: evident exertional dyspnea; atrioventricular second-degree or third-degree block; multifocal atrial extrasystole; multifocal ventricular extrasystole; atrial fibrillation; presence of systolic dysfunction defined by echocardiography; cardiac hypertrophy defined by echocardiography; evidence of thromboembolic disease with characterized cardiac emboli source in echocardiography), criteria adapted from the WHO/ Panamerican Healthy Association Classification for Chagas Disease.10
Blood samples were stored at -20ºC and the CRP was quantified by immunophelemetry, utilizing high sensitivity kits (Dade Behring, Germany).
RESULTS
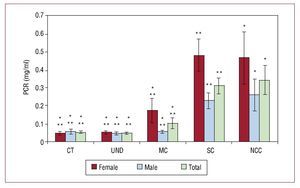
The characteristics of the studied population are shown in Table 1. The average CRP value in the whole group of women (0.24 [0.36] mg/dL) was higher than those observed in men (0.12 [0.18] mg/ dL), although not statistically significant (P>.05), due to the high variability of values. The analysis of the quantification of CRP in the serum, when stratified in the different clinical presentations of CD, demonstrated that the SC and NCC have statistically higher levels of CRP than other groups (P<.05). As such, a tendency towards increased CRP expression was observed, as CD worsens. In more intense cardiopathy diseases (SC and NCC), CRP reached higher levels, when compared to control, IND and MC, as seen in Figure. These results were observed even when the group was separated according to gender (Mann-Whitney Test).
Figure 1. Quantitative analysis of CRP and SD, stratified by gender and clinical pattern of CD (mean [SD]). The CRP levels presented significantly higher values in SC and NCC compared to CT, UND and MC (P<.001, Kruskal-Wallis test). CRP indicates c-reactive-protein; SD, standard deviation; SC, severe cardiopathy; NCC, non-chagas cardiopathy; MC, mild cardiopathy.
The CRP presented mean values superior (P<.001, Kruskal-Wallis Test) among SC and NCC groups in comparison to CT, IND and MC groups, even when the sample was stratified according to age (<40 and ≥40 years old). The Spearman coefficient also did not demonstrate a correlation of the CRP levels and specific groups of cardiac CD.
The covariance analysis (ANCOVA) was performed by comparing the variables in groups, adjusted for gender and age and rank converted, and the CRP was higher among SC and NCC when compared to CT, IND and MC (P<.001). There was no difference in CRP levels between NCC and SC patients (Table 2).
DISCUSSION
Many inflammatory cytokines have been implicated in the development of chronic heart failure, such as TNF-α, (IL-6), IL-1β, and IL-2.1,8,11 It has been demonstrated that CRP participates in early atherogenesis via monocyte recruitment, classical complement pathway activation and opsonization through C1q, and upregulation of lectin-like oxidized LDL receptor-1 (LOX-1), which promotes a higher degree of oxidized LDL binding to LOX-1 receptor in endothelial cell surface.12 It has also been demonstrated that CRP inhibit fibrinolysis by increasing the expression and activity of plasminogen activator inhibitor-1 (PAI-1), and modulates the overexpression of adhesion molecules such as ICAM-1, VCAM-1, and E-selectin in endothelial cells.6,7,9 All these mechanisms contribute to an endothelial cell phenotype that is pro-coagulant, pro-oxidant and atherogenic, which may explain the reported association of CRP to cardiovascular disease.9
The quantification of CRP in serum showed higher levels in SC and NCC, compared to other clinical groups. The elevation of CRP in the most severe cases of cardiomyopathy suggests that it may be related to the progression of myocardial injury. A possible inference of CRP overproduction associated with chronic heart disease progression could be made, as there is considerable data suggesting a chronic inflammatory process in the most severe forms of heart failure. When the patients were stratified according to age, utilizing the boundary limit of 40 years old, the SC and NCC groups were found to maintain higher levels of CRP in serum. Indeed, covariance analysis showed that, even with age and gender adjustment, the CRP production was augmented in SC and NCC individuals.
The available data demonstrate the elevation of circulating IL-6 in the serum of patients with heart failure and the concentration of IL-6 is related to the degree of left ventricular dysfunction. Despite the known overexpression of IL-6 in the acute phase of CD, when the parasites reach the highest levels in the acute onset of infection, the role of IL-6 in the chronic progression to cardiomyopathy in CD is still not well characterized.2,13 It was demonstrated that individuals with CRP elevation experienced a 2.2-fold higher risk of progression to heart failure, as did the patients presenting concomitant increment in IL-6, CRP level, mononuclear peripheral blood cells and TNF-α, which elevated the risk of developing chronic failure 4.1-fold.14 López et al analyzed IL-6 in CD patients, observing that both IL-6 and CRP serum levels were increased in the most advanced phase of disease and that there was a positive correlation between high left ventricular mass index and IL-6 production.13
In conclusion, taken together, these data reinforce the association of a chronic inflammatory event in the development of heart failure: the CRP elevation can not be associated exclusively with CD progression, but instead must be understood as a part of a more intriguing role of the inflammation and the cytokines in the myocardial degeneration in the heart failure onset. Although CRP is not specifically related to CD, it may be used as a feasible marker of CD evolution for more advanced phases of cardiac impairment.
Correspondence: Prof. Dr. A. Fattori,
Departamento de Clínica Médica,
Rua Alexander Fleming, 40. Caixa Postal 6111. (13083-970) Campinas. São Paulo. Brazil
E-mail: afattori@fcm.unicamp.br; afattori@unicamp.br
Received November 25, 2008.
Accepted for publicaction September 22, 2009.